© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
If the human heart always worked correctly and contracted with the same regularity, there would be no diseases such as arrhythmias, and there would not be a vast subsection of cardiology called arrhythmology. Thousands of patients around the world experience one or another type of arrhythmia due to various reasons. Arrhythmias have not been spared in very young patients, in whom registration of an irregular heart rhythm on a cardiogram is also quite common. One of the common types of arrhythmias are disorders such as ectopic rhythms.
What happens with ectopic heart rhythm?
the cardiac cycle is normal - the primary impulse comes ONLY from the sinus node
In a normal human heart, there is only one path for conducting an electrical impulse, leading to sequential excitation of different parts of the heart and to productive cardiac contraction with sufficient release of blood into large vessels. This path begins in the right atrial appendage, where the sinus node (1st order pacemaker) is located, then passes through the atrial conduction system to the atrioventricular (atrioventricular) junction, and then through the His system and Purkinje fibers reaches the most distant fibers in the tissue of the ventricles.
But sometimes, due to the action of various reasons on the cardiac tissue, the cells of the sinus node are not able to generate electricity and release impulses to the underlying sections. Then the process of transmitting excitation through the heart changes - after all, in order for the heart not to stop completely, it should develop a compensatory, replacement system for generating and transmitting impulses. This is how ectopic or replacement rhythms arise.
So, ectopic rhythm is the occurrence of electrical excitation in any part of the conducting fibers of the myocardium, but not in the sinus node. Literally, ectopia means the appearance of something in the wrong place.
The ectopic rhythm can originate from the tissue of the atria (atrial ectopic rhythm), in the cells between the atria and the ventricles (rhythm from the AV junction), and also from the tissue of the ventricles (ventricular idioventricular rhythm).
Causes and mechanisms of occurrence
Etiological factors are divided into two groups:
- congenital - these include Wolff-Parkinson-White syndrome;
- acquired - diseases suffered by the patient during his life and contributing to the development of reciprocal tachycardia (myocarditis, etc.).
The heartbeat increases in this case due to the presence in the atrioventricular node of two types of electrical impulse conduction, which are interconnected (the phenomenon of longitudinal dissociation of the AV connection). They are called the “fast” or beta path, and the “slow” - alpha path.
A specific start is the occurrence of spontaneous extrasystole (extraordinary contraction of the heart). In this case, the first of the paths should not be ready to receive the signal (refractory state). Thus, AV conduction will be carried out along the alpha beam. Along the “fast” tract that has emerged from rest, the excitation wave travels in the opposite direction and merges with the first one. Subsequently, they circulate in the AV junction, and the re-entry circuit (circular movement of the impulse) is closed.
Why does ectopic rhythm appear?
Ectopic rhythm occurs due to a weakening of the rhythmic functioning of the sinus node, or a complete cessation of its activity.
In turn, complete or partial inhibition of the sinus node is the result of various diseases and conditions:
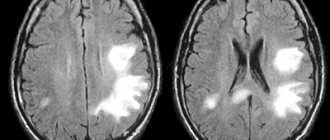
- Inflammation. Inflammatory processes in the heart muscle can affect both the cells of the sinus node and the muscle fibers in the atria and ventricles. As a result, the ability of cells to produce impulses and transmit them to underlying sections is impaired. At the same time, the atrial tissue begins to intensively generate excitation, which is supplied to the atrioventricular node at a frequency higher or lower than usual. Such processes are caused mainly by viral myocarditis.
- Ischemia. Acute and chronic myocardial ischemia also contributes to impaired activity of the sinus node, since cells deprived of sufficient oxygen cannot function normally. Therefore, myocardial ischemia occupies one of the leading places in the statistics of the occurrence of rhythm disturbances, including ectopic rhythms.
- Cardiosclerosis. The replacement of normal myocardium with growing scar tissue due to previous myocarditis and infarctions interferes with the normal transmission of impulses. In this case, in persons with ischemia and post-infarction cardiosclerosis (PICS), for example, the risk of ectopic heart rhythm increases significantly.
In addition to pathology of the cardiovascular system, vegetative-vascular dystonia, as well as hormonal imbalances in the body - diabetes mellitus, pathology of the adrenal glands, thyroid gland, etc., can lead to ectopic rhythm.
Symptoms of ectopic rhythm
The clinical picture of replacement heart rhythms can be clearly expressed or not manifested at all. Usually, the symptoms of the underlying disease come first in the clinical picture, for example, shortness of breath on exertion, attacks of burning pain in the chest, swelling of the lower extremities, etc. Depending on the nature of the ectopic rhythm, the symptoms may be different:
- With ectopic atrial rhythm , when the source of impulse generation is located entirely in one of the atria, in most cases there are no symptoms, and disturbances are detected by the cardiogram.
- With a rhythm from the AV junction, a heart rate close to normal is observed - 60-80 beats per minute, or below normal. In the first case, no symptoms are observed, but in the second, attacks of dizziness, a feeling of lightheadedness and muscle weakness are noted.
- With extrasystole, the patient notes a feeling of fading, cardiac arrest, followed by a sharp jolt in the chest and a further absence of sensations in the chest. The more often or less often the extrasystoles, the more varied the symptoms in duration and intensity.
- With atrial bradycardia , as a rule, the heart rate is not much lower than normal, within 50-55 per minute, as a result of which the patient may not notice any complaints. Sometimes he is bothered by attacks of weakness and sudden fatigue, which is caused by a reduced flow of blood to the skeletal muscles and brain cells.
- Paroxysmal tachycardia manifests itself much more clearly. During paroxysm, the patient notes a sharp and sudden sensation of accelerated heartbeat. According to many patients, the heart flutters in the chest like a “hare’s tail.” The heart rate can reach 150 beats per minute. The pulse is rhythmic, and may remain around 100 per minute, due to the fact that not all heartbeats reach the peripheral arteries at the wrist. In addition, there is a feeling of lack of air and chest pain caused by insufficient oxygen supply to the heart muscle.
- Atrial fibrillation and flutter can be paroxysmal or permanent. The basis of atrial fibrillation is a chaotic, non-rhythmic contraction of different parts of the atrium tissue, and the heart rate in the paroxysmal form is more than 150 per minute. However, there are normo- and bradysystolic variants, in which the heart rate is within the normal range or less than 55 per minute. The symptoms of the paroxysmal form resemble an attack of tachycardia, only with an irregular pulse, as well as a feeling of irregular heartbeat and interruptions in heart function. The bradysystolic form may be accompanied by dizziness and lightheadedness. With a permanent form of arrhythmia, the symptoms of the underlying disease that led to it come to the fore.
- Idioventricular rhythm is almost always a sign of serious cardiac pathology, such as severe acute myocardial infarction. In most cases, symptoms are noted, since the myocardium in the ventricles is capable of generating electricity at a frequency of no more than 30-40 per minute. In this regard, the patient may experience Morgagni-Edams-Stokes (MES) episodes - attacks of loss of consciousness lasting several seconds, but no more than one or two minutes, since during this time the heart “turns on” compensatory mechanisms and begins to contract again. In such cases, they say that the patient is “massing.” Such conditions are very dangerous due to the possibility of complete cardiac arrest. Patients with idioventricular rhythm are at risk of developing sudden cardiac death.
Classification and types
Modern cardiological communities have recognized the division of atrioventricular nodal reciprocal tachycardia into the following 3 types:
- slow-fast - a typical option in which the electrical impulse from the atria through the Aschoff-Tavara node passes along the “slow” path, and back along the “fast” path;
- fast-slow - an atypical form, which is the opposite of the first option;
- slow-slow - a rare type: the current passes through two “slow” beams.
The course of the disease can be paroxysmal (attacking) and chronic. The latter option is rarely observed. Over time, it leads to expansion of the cavities of the heart and the formation of tachycardiomyopathy. Paroxysms, in turn, are characterized by an acute spontaneous onset and the absence of long-term complications.
Wolff-Parkinson-White syndrome (WPU, WPW)
WPW syndrome is caused by the presence of an abnormal bundle of Kent, a connection between the atrium and one of the ventricles. With this pathology, the formation of atrioventricular reciprocal tachycardia through the re-entry mechanism is also possible. There are two types:
- orthodromic - forward along a specialized conduction system, back from the ventricles along an additional atrioventricular connection;
- antidromic - from the atria through the anomalous bundle of Kent and back through the AV node.
Ectopic rhythms in children
In children, this type of arrhythmia can be congenital or acquired.
Thus, ectopic atrial rhythm occurs most often with vegetative-vascular dystonia, with hormonal changes during puberty (in adolescents), as well as with pathology of the thyroid gland.
In newborns and young children, a right atrial, left or lower atrial rhythm may be a consequence of prematurity, hypoxia or pathology during childbirth. In addition, the neurohumoral regulation of heart activity in very young children is immature, and as the baby grows, all heart rate indicators can return to normal.
If the child does not have any pathology of the heart or central nervous system, then the atrial rhythm should be considered a transient, functional disorder, but the baby should be regularly monitored by a cardiologist.
But the presence of more serious ectopic rhythms - paroxysmal tachycardia, atrial fibrillation, atrioventricular and ventricular rhythms - require more detailed diagnosis, as this may be due to congenital cardiomyopathy, congenital and acquired heart defects, rheumatic fever, viral myocarditis.
Diagnosis of ectopic rhythm
The leading diagnostic method is the electrocardiogram. If an ectopic rhythm is detected on the ECG, the doctor should prescribe a further examination plan, which includes cardiac ultrasound (ECHO-CS) and daily ECG monitoring. In addition, patients with myocardial ischemia are prescribed coronary angiography (CAG), and patients with other arrhythmias are prescribed transesophageal electrophysiological examination (TEPE).
ECG signs for different types of ectopic rhythm differ:
- With an atrial rhythm, negative, high, or biphasic P waves appear, with a right atrial rhythm - in additional leads V1-V4, with a left atrial rhythm - in V5-V6, which may precede or overlap the QRST complexes.
accelerated ectopic atrial rhythm
- The rhythm from the AV junction is characterized by the presence of a negative P wave, superimposed on the QRST complexes, or present after them.
AV nodal rhythm
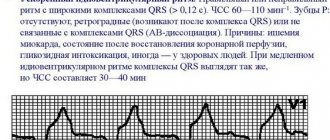
- Idioventricular rhythm is characterized by a low heart rate (30-40 per minute) and the presence of altered, deformed and widened QRST complexes. There is no P wave.
idioventricular (ventricular) ectopic rhythm
- With atrial extrasystole, premature, extraordinary, unchanged PQRST complexes appear, and with ventricular extrasystole, altered QRST complexes appear followed by a compensatory pause.
atrial and ventricular ectopia (extrasystoles) on the ECG
- Paroxysmal tachycardia is characterized by a regular rhythm with a high frequency of contractions (100-150 per minute), P waves are often quite difficult to determine.
- Atrial fibrillation and flutter on the ECG are characterized by an irregular rhythm, the P wave is absent, and fibrillation f waves or flutter waves F are characteristic.
Expert advice: how to treat
To reduce the heart rate at home, I allow vagal tests to be used independently. For example, you can use one of the following recommendations:
- strain at the height of inspiration (Valsalva method);
- press on the eyeballs (Aschner);
- massage the area of the carotid sinus (anterolateral parts of the neck at the level of the thyroid cartilage).
These methods make it possible to reduce the heart rate, and in some cases even stop an attack of nodal reciprocal tachycardia.
Of the pharmacological agents, the drugs of choice are ATP or Isoptin. The route of administration is intravenous. To prevent paroxysms, I use the following antiarrhythmic medications:
- retard (long-acting) forms of "Verapamil";
- "Allapinin";
- "Etatsizin";
- "Propaphenone".
I often recommend surgical intervention to my patients, which consists of catheter ablation (destruction by electric current) of the “slow” pathway of the atrioventricular node. Cure occurs in 95% of patients. But I want to warn that in 0.5% of cases, a serious complication develops during the operation - persistent AV block of the II-III degree. It requires the installation of a pacemaker.
Treatment of ectopic rhythm
Treatment is not carried out in cases where the patient has an ectopic atrial rhythm that does not cause unpleasant symptoms, and pathologies of the heart, hormonal and nervous systems have not been identified.
In the case of moderate extrasystole, the prescription of sedatives and restorative drugs (adaptogens) is indicated.
Therapy for bradycardia, for example, with an atrial rhythm with a low contraction frequency, with the bradyform of atrial fibrillation, consists of prescribing atropine, ginseng preparations, Eleutherococcus, Schisandra and other adaptogens. In severe cases, with a heart rate less than 40-50 per minute, with attacks of MES, implantation of an artificial pacemaker (pacemaker) is justified.
Accelerated ectopic rhythm, for example, paroxysms of tachycardia and atrial fibrillation-flutter require emergency assistance, for example, the administration of a 4% solution of potassium chloride (panangin) intravenously, or a 10% solution of novocainamide intravenously. Subsequently, the patient is prescribed beta blockers or antiarrhythmic drugs - Concor, Coronal, verapamil, propanorm, digoxin, etc.
In both cases - both slow and accelerated rhythms, treatment of the underlying disease , if any, is indicated.