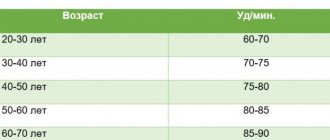
A heart rate (HR) of more than 90 beats/min is considered elevated. in a minute. It can be like this in normal conditions and in pathologies. If the heart rate is increased in a healthy person, the reason for this is increased air temperature, high physical activity or emotional overload.
But the heartbeat often accelerates in pathologies. Among them are diseases of the cardiovascular, endocrine, respiratory, nervous systems, as well as infectious diseases. In these cases, patients require immediate medical attention to relieve stress on the heart muscle.
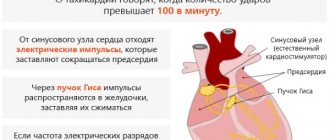
What happens in the heart
Most often, such a pulse occurs in paroxysms and reflects the development of supraventricular tachycardia. What kind of rhythm disturbance is this:
- with supraventricular tachycardia, the heart rate ranges from 140 to 220 per minute (usually in the range of 160 to 180 per minute);
- the source of electrical signals is not the usual sinus node, but a cluster of cells between the atria and ventricles; therefore, the atria are excited retrogradely (from bottom to top), and their contractility is impaired;
- due to the “bifurcation” of the atrioventricular node into 2 paths, with this arrhythmia the impulse quickly circulates through the resulting loop, constantly stimulating the ventricles with a frequency of 140 per minute and higher;
- little blood enters the ventricles, and just as little of it is thrown into the aorta, so the body experiences a pronounced lack of blood circulation.
Another reason why the pulse can be in the range of 140 – 150 or more is the tachysystolic form of atrial fibrillation, or atrial fibrillation. With this disorder, the muscle fibers of the atria contract irregularly, as if twitching, with a very high frequency (up to 450 per minute). Only a portion of these signals are carried to the ventricles.
The tachysystolic form is said to occur when the number of heart contractions during atrial fibrillation exceeds 100 per minute.
When it increases to 140 per minute, a pulse deficit often occurs. This is a discrepancy between heartbeats and palpable pulse waves, since some of them are “empty”; very little blood is thrown into the aorta at this time.
Therefore, if the pulse is 150 beats per minute or higher, and it is rhythmic, we are most likely talking about supraventricular tachycardia.
Such a pulse during exercise can normally be observed in young people and children. However, prolonged sinus tachycardia up to 170 per minute can adversely affect the heart muscle. Therefore, it is necessary to develop a sports training regimen individually, with gradual adaptation of the body.
Reasons for increased heart rate
There are practically no physiological reasons for such tachycardia. These include only cases of significant stress in children and young people. Supraventricular tachycardia can appear at any age, but most often first develops in people between 20 and 40 years of age. Sometimes attacks of rapid heartbeat suddenly occur at night, awakening the patient. Up to 2/3 of all cases of increased heart rate up to 150 – 170 – 220 per minute are recorded in healthy people with risk factors:
- neurocirculatory dystonia with a tendency to increase blood pressure and palpitations;
- drinking large amounts of strong tea, coffee, energy drinks, alcohol, excessive smoking;
- frequent viral infections suffered “on your feet”.
Diseases that can cause heart rate to increase to such limits in people under 40 years of age:
- myocarditis of a viral or rheumatic nature;
- congenital and acquired heart defects, primarily mitral valve stenosis.
- In people 40 – 60 years of age and older, attacks of heart rate of more than 140 per minute can appear due to the growth of connective tissue in the heart muscle, that is, with atherosclerotic cardiosclerosis. With age, the severity of this process increases, so in most older people, during daily monitoring, a small number of attacks of rapid heartbeat are recorded, which they may not feel.
- Other possible reasons for increased heart rate to 140 - 170 per minute:
- hypertonic disease;
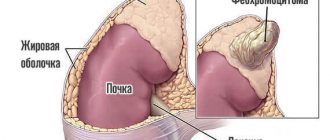
- adrenal tumor pheochromocytoma;
- myocardial infarction;
- lung diseases with the development of “pulmonary heart”;
- surgical operations on the heart, for example, for a congenital defect or organ injury.
In 3 out of 100 patients, supraventricular tachycardia is caused by Wolff-Parkinson-White (WPW) syndrome. Unlike the usual form of the disease, with this syndrome there is an additional bundle that connects the conduction system of the atria and ventricles, bypassing the AV node. It turns out that the excitation loop is formed not between two longitudinally separated parts of the AV junction, but between it and the additional bundle, which provides additional opportunities for successful surgical treatment. Such attacks occur in 2/3 of patients with WPW and often occur in young people.
More rare non-cardiac causes of rapid heart rate up to 150 – 170 – 200 per minute:
- diseases of the abdominal organs (cholecystitis, pancreatitis);
- urolithiasis (kidney stones);
- brain diseases;
- thyrotoxicosis;
- pathological course of menopause;
- pregnancy;
- overdose of cardiac glycosides.
Symptoms
Oddly enough, an increase in heart rate of more than 140 per minute that occurs suddenly is usually well tolerated by patients. Such an attack can even last for several days, and the patient does not notice it or only feels weakness that is incomprehensible to him.
The more the heart muscle is affected and the more severe the heart disease, the more signs appear during an attack of tachycardia:
- chest pain;
- shortness of breath, lack of air, especially when lying down;
- sweating, severe weakness;
- dizziness, clouding of consciousness;
- fainting, loss of consciousness.
In the most severe cases, there is a risk of developing a stroke.
Symptoms of the disorder
Depending on the symptoms and characteristics, three types of tachycardia are distinguished:
- sinus (nodular);
- supraventricular;
- ventricular
A pulse of 150 indicates the presence of sinus or supraventricular tachycardia.
Sinus tachycardia
The main symptoms of the disorder are:
- strong heartbeat is accompanied by pain (a feeling of squeezing) in the chest;
- fainting;
- feeling of weakness;
- panic attack (feeling of fear for your life);
- severe lack of air;
- blurred vision.
Diagnostics
From laboratory tests, it is perhaps important to determine the level of TSH and T4 in the blood to assess the function of the thyroid gland. Also, general and biochemical blood tests and rheumatic tests will not be superfluous.
Usually, special studies are required to confirm the very fact of the presence of such a rhythm disorder. After all, increased heart rate occurs in attacks and cannot always be recorded on a regular ECG. Therefore, additional research methods are prescribed:
- 24-hour ECG monitoring – the patient wears a small device with receiving electrodes that constantly record the ECG for 20–24 hours;
- cardiac event monitor - a less common research method in which the device can be worn on the body indefinitely, and when an attack occurs, press a button and send the data to the hospital;
- Echocardiography, or ultrasound of the heart, helps identify organ defects, heart failure and other diseases;
- transesophageal electrophysiological study necessary to determine the source of the arrhythmia;
- intracardiac electrophysiological study, which is carried out immediately during surgery to search for a focus of pathological signals or an additional pathway in WPW syndrome.
Additionally, an ultrasound scan of the adrenal glands, gallbladder, pancreas and thyroid gland, and cerebral vessels may be prescribed.
Treatment
If your heart rate suddenly increases to 140 - 170 per minute or more, you can try to help yourself, but then still call an ambulance, especially if the paroxysm occurs for the first time.
For a pulse with a heart rate exceeding 140 beats, the following is used for treatment:
- Home remedies.
- Medicines.
- Surgery.
Home Remedies
If the attack was not accompanied by fainting or a drop in blood pressure, vagal tests can be used to stop it:
- inhale and strain, as during bowel movements;
- wash with cold water;
- Drink a glass of cold water in small sips.
In young children, it is permissible to use carotid sinus massage, that is, gently rubbing the area of the carotid artery for several seconds. If the child is right-handed, the maneuver should be performed on the right, if left-handed, then on the left, that is, from the side of the non-dominant hemisphere.
Medicines
Ambulance doctors who arrive at the scene can administer medications from the following:
- adenosine;
- verapamil or diltiazem;
- amiodarone.
When paroxysm of atrial fibrillation develops, medications (amiodarone, flecainide, propafenone) or electrical restoration of sinus rhythm are used to stop it. Atrial fibrillation, even paroxysmal, increases the risk of stroke, so anticoagulant therapy is recommended for this disease - from traditional warfarin to the newer dabigatran, rivaroxaban and apixaban.
In the future, many patients who have suffered an attack of increased heart rate are offered treatment with beta blockers or calcium antagonists.
Surgery
Before the advent of percutaneous radiofrequency catheter ablation (RFA), the only treatment for severe paroxysmal tachycardias was open cardiac surgery. Now they are practically not carried out, and RFA is considered the first treatment for recurrent attacks of rapid pulse, accompanied by unfavorable symptoms. In many cases, the intervention is performed under local anesthesia and requires only 1 to 3 days of hospitalization.
RFA is used to treat arrhythmias accompanied by an increase in heart rate of more than 140 per minute - atrial, AV nodal tachycardia, flutter and, in some cases, atrial fibrillation.
Candidates for surgery are people whose frequent palpitations cause dizziness and other symptoms and do not respond to drug therapy. Surgery is also performed for symptomatic WPW syndrome.
The effectiveness of RFA is often higher than with long-term medication. In this case, the patient no longer has to spend money on purchasing them, and, naturally, does not experience side effects. RFA is also more effective for the prevention of severe paroxysms, when palpitations can only be relieved by defibrillation (electric shock using a special device).
In the treatment of paroxysmal supraventricular tachycardia, which is the most common cause of increased heart rate to 160 - 190 at rest, the effectiveness of RFA reaches 90%. The surgical technique is well developed, and intervention should never be refused if doctors offer it.
Therapeutic measures
The disease is always better and easier to prevent. But if it does affect the body, it is necessary to provide adequate first aid to a patient with tachycardia. A number of potent medications are used for this. In the future, such patients are prescribed a special drug regimen for lifelong use.
Preventive measures
In order to prevent a pathological increase in heart rate, the patient must adhere to the following rules:
- Lead a healthy lifestyle. Quitting smoking and alcohol and substance abuse will help reduce the risk of tachycardia.
Avoid excessive stress. To do this, you need to study mental hygiene and try to adhere to all its rules.- Attend diagnostic examinations regularly. This is especially true for patients at risk who are prone to atherosclerotic vascular damage and have a high concentration of low-density lipoproteins in the blood.
- Engage in moderate physical labor. Exercise within reasonable limits is beneficial for the body, as it stimulates cells and tissues to renew themselves.
First aid
Faced with an increase in heart rate, a person asks the question: what to do in such a situation, how to help yourself or a loved one? First of all, the patient needs to calm down. To do this, he must take a sitting or lying position and, if possible, seek help from others or call an ambulance. If tachycardia is accompanied by chest pain, you should take a Nitroglycerin tablet.
To stop an attack of tachycardia, the treatment regimen includes the following drugs:
- antiarrhythmics Amiodarone, Cordarone;
- some calcium channel blockers: Verapamil, Amlodipine, Nifedipine;
- beta blockers: Propranolol, Bisoprolol, Atenolol and Carvedilol.
Forecast
Short-term attacks of increased heart rate up to 170 per minute are not dangerous to health. The likelihood of complications arises in the following situations:
- severe heart disease;
- the first month after myocardial infarction;
- unstable angina, increased frequency of attacks, increased need for nitroglycerin;
- drop in blood pressure and fainting during an attack.
In all these cases, the patient should be a candidate for RFA surgery, which will help completely get rid of palpitations.
Danger and consequences
A pulse of 140 is not dangerous if it develops with adequate physical or emotional stress. When the room is too hot, a person is forced to move or is wearing tight synthetic or thick clothing, such indicators are also not a pathology. But if a symptom accompanies a disease of a particular organ, it poses a danger to human health and life.
Persistent tachycardia leads to arterial hypotension, decompensation of cardiac output, and decreased blood supply to organs. Through a pathological circle, this can lead to recurrent myocardial infarction or ischemic coronary syndrome.