Heart rate is considered one of the main indicators of the state of the cardiovascular system and the body as a whole. The heart rate level is a dynamic value: it changes every second, but is always within certain limits.
The boundaries that are considered reference have long been named by both the World Health Organization and national cardiology communities. These are considered numbers in the range from 70 to 80 beats per minute, plus or minus, depending on the cardiological concept or “school”.
How adequate is a level of 110-115 beats per minute at rest? According to the generally accepted classification, this is moderate tachycardia, which approaches pronounced tachycardia in frequency.
This condition does not bode well for the patient: if bradycardia in many cases occurs as a result of the influence of physiological factors: fatigue, overabundance of medications, climate change, everything is much more complicated here.
Statistics speak directly: 70-80% of cases of accelerated heart rate are the result of pathology. And already within this system, cardiac problems account for about 60% of situations. That is, most people with tachycardia are patients with severe pathologies in latent or early forms.
Natural Factors to Increase Heart Rate
There are not many of them. It is possible to distinguish a pathogenic process from a relatively harmless condition through diagnosis.
If no organic pathologies are identified, it makes sense to work through the problem with a neurologist and psychotherapist.
Interesting:
You can try to distinguish one from the other based on the clinical picture: with physiological deviations there are almost no symptoms, and if there are, they are short-lived.
What are we talking about:
- A stressful situation that develops over a long period. For example, the moment before an exam or a public speaking. The body mobilizes and produces more specific hormones: catecholamines and corticosteroids. Hence tachycardia and increased blood pressure, as well as other autonomic symptoms. No treatment is required, everything returns to normal after the stressful situation ends.
- Psychological overload, nervous breakdown or shock. It develops like a snowball; the body simply cannot stand it. The pressure jumps sharply, the heart rate rises to significant levels, up to 110-150 beats per minute, the patient falls into a stupor or completely loses consciousness for a short period. Autonomic manifestations are obvious, clearly visible even to a person without medical education: tachycardia, cyanosis of the nasolabial triangle, pallor of the skin, sweating, affective manifestations (laughter, tears, inhibition of thinking, anger or irritability). Therapy is carried out with sedatives or tranquilizers until the condition stabilizes.
- Too much tonic. This can be either harmless coffee or cocaine with heroin, which also cause persistent tachycardia. The difference is in the duration of the effect: when consuming the first, the heartbeat continues for 2-4 hours, while drugs cause persistent deviation for 12-24 or more hours, and we are not talking about the effect of opiates, but as a result of the influence of harmful impurities of homemade street psychoactive substances . Treatment in the second case is urgent, with detoxification and neutralization of the harmful effects.
- Moving to a damp or humid climate. At the same time, it is not necessary to move anywhere; unfavorable weather conditions can come on their own. This is especially noticeable in the summer months in regions with a harsh continental climate. The entire central zone of Russia is like this. Heavy weather is difficult to bear, you need to move less, drink more and better not go outside.
- Nightmares. They differ from other processes in their short duration. Autonomic symptoms cease to exist as quickly as they appeared. Within 2-5 minutes. No specialized medical care is required.
In 30% of cases, a pulse of 110 means that there are physiological deviations as a result of the subjective controlled actions of the patient himself or the influence of external stimuli. Correction is almost never required.
Interesting facts about the influence of external conditions on heart rate
The Institute of Clinical Cardiology conducted experiments to study the causes of disruptions in the circulatory system. Laboratory rabbits were restricted in movement for 70 days. This led to atrophy of their muscle fibers (myofibrils), a decrease in the lumen of blood vessels, an increase in capillary walls and disruption of intercellular connections, which immediately affected the pulse rate. Watching a film with a sad plot by volunteers reduced the volume of current in the blood by 35%, and increased it by 22% when watching a comedy. Daily consumption of dark chocolate increases the efficiency of the human circulatory system by 14%.
Pathological factors
They occur much more often. Possible diseases include:
- Diabetes. Systemic endocrine condition. Requires lifelong therapy. In the early stages, it is difficult to identify; there is often a latent course: the patient can walk with the problem for years; it is discovered by chance or when it is too late for a total correction. You need to pay attention to the following manifestations: sudden attacks of hunger, tremors (shaking hands), pallor, weakness in the legs, fainting. Objectively, glucose does not always increase; you need to examine the sugar curve throughout the day. The heart and blood vessels suffer “for company”, diabetes affects all organs and systems.
- Problems with blood circulation in the brain. The result of osteochondrosis and compression of the arteries feeding the cerebral structures. The normal regulation of cardiac activity at the level of the central nervous system is disrupted. Therapy is carried out under the supervision of a neurologist.
- Hyperthyroidism. Excessive production of thyroid hormones as a result of poor nutrition, natural factors, and the development of tumors. Accompanied by increased body temperature, headaches, shortness of breath, weakness, fatigue, inability to sleep, bulging eyeballs, changes in the relief of the neck (goiter), and mental disorders of a depressive-affective nature. Treatment under the supervision of an endocrinologist.
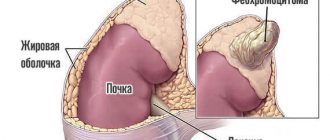
- Hypercorticism. Another pathology of the same profile. The concentration of adrenal hormones, primarily cortisol, only increases. Secondary Itsenko-Kushang disease occurs with sudden weight gain, uneven fat deposition, destruction of the spine and entire skeleton, and mental problems. Often results from a tumor of the adrenal gland or pituitary gland. Treatment under the supervision of an endocrinologist and neurosurgeon.
- Violations from the heart itself. As a result of irritation of the third reflex zone of the organ, the heart rate accelerates. The assessment is carried out by a cardiologist. Despite the variety of diseases, their symptoms are almost the same: chest pain of a pressing nature, radiating to the arms and back, shortness of breath even at rest, especially after physical activity, sweating, blue discoloration of the nasolabial triangle, pallor of the dermal integument, fatigue, arrhythmias ( not only by type of tachycardia). Mandatory electrocardiography is carried out, and, if possible, stress tests.
- Vascular diseases. First of all, atherosclerosis, with narrowing or blockage of the lumen by cholesterol plaque. Lipid deposits grow radially, along the entire diameter of the blood supply structure, making it more difficult for blood to overcome resistance. That's why the heart speeds up. This is the only visible symptom. Another, less obvious one is increased blood pressure.
- Panic attack, affective disorders. Psychotherapeutic problems.
A pulse of 107-112 beats per minute is the result of hemodynamic and endocrine pathologies. Often in the system. Therefore, treatment is carried out under the supervision of a group of doctors of different profiles.
How to measure a sleeping person's pulse
There are several ways to check the pulse rate of a sleeping person. The first is the traditional pressing of the fingers on the wrist and counting the number of blows. You can ask a close relative who will measure your pulse in different phases of sleep.
Another way is a modern heart rate monitor device with a built-in alarm clock. Its functions are to count the rhythmic beats of the arteries. During sleep, the device reads various indicators related to the body:
- reflects the position;
- draws up schedules;
- records sleep phases and number of beats.
A heart rate monitor is a device that allows you to measure your heart rate during sleep.
Then it analyzes all the collected data and determines a favorable time to wake up, which gives a signal to the built-in alarm clock to vibrate. The “heart rate monitor” is a great way to determine the quality of sleep and check the functioning of the cardiovascular system at rest. These are also analytical system indicators that reflect the health of a sleeping person.
What can you do at home?
Quite a bit. This level of tachycardia is difficult to correct on your own, but it’s worth a try. The main thing is to strictly follow the recommendations and not skip steps:
- Take 1 tablet of Karevdilol or, better, Anaprilin. They should stabilize within 10-15 minutes.
- Secure the result by drinking herbal preparations (motherwort or valerian), phenobarbital (Corvalol, Valocordin).
- You can replace sedatives with folk recipes: 1 tablespoon of a mixture of lemon and honey or 1 glass of tea with St. John's wort, chamomile, peppermint and the same motherwort and valerian.
After 30 minutes everything should return to normal. If this does not happen, you should try to lower your heart rate with a breathing exercise. Inhale, 5 seconds, exhale the same amount. And so on for 10 minutes.
All this time you need to lie down and move less. Loosen tight clothing constricting your neck and remove jewelry.
If there is no effect, or if the pulse starts to jump, call an ambulance to resolve the issue on the spot or in a hospital.
Attention:
A heartbeat of 110 beats per minute requires drug correction in the hospital if the phenomenon lasts more than 30 minutes. or the presence of accompanying manifestations.
Expected duration of attack
The duration of a pulse increased to 110 beats per minute depends on its cause:
- the heartbeat as a result of the fever will return when the body temperature returns to normal;
- rapid pulse caused by blood loss is corrected after intravenous administration of solutions or blood components;
- in case of pathology of the thyroid gland, it is necessary to suppress its synthesis of excess thyroid hormones;
- a rapid pulse caused by excessive coffee consumption or the effects of medications is restored after about an hour, when the active substances begin to be eliminated from the body;
- in case of heart or lung diseases, increased heart rate persists for a long time, including at rest.
Symptoms requiring an ambulance call
There are quite a lot of them, you should pay attention to the following signs of problems with the heart:
- Chest pain of a pressing type, radiating to the arms or back.
- Breathing problems. Dissatisfaction after inhalation, even at rest. The frequency of movements increases, the phenomena of hypoxia also increase.
- Dizziness.
- Cephalgia (headache). Pulsating in time with the beat of the heart.
- Fatigue, drowsiness for no apparent reason. Decreased performance.
- Weakness in the legs, inability to navigate in space.
- Visual impairment.
- Decreased hearing.
In these cases, an ambulance must be called to correct the condition and possible transportation to a hospital for diagnostics.
If there is at least one of these manifestations, the issue of saving life will already be resolved:
- Acute headache in the back of the head, accompanied by neurological symptoms.
- Blindness.
- Facial distortion.
- Paralysis of half the body, paresis of the limbs.
- Inability to speak normally.
- Complete lack of orientation in space.
110 beats per minute at rest is already grounds for calling an ambulance. Adequate regulation of heart rate occurs in a matter of minutes, if not faster. Otherwise, a pathological process takes place.
Normal pulse waves, possible deviations
Pulse is a value that reflects the frequency of contractions of the heart muscle. It is measured in the number of beats per unit of time (minute). This value is very unstable, since it can change under the influence of external factors. Most often, pulse fluctuations are affected by:
- Times of Day;
- body position;
- physical activity;
- eating;
- emotional experiences.
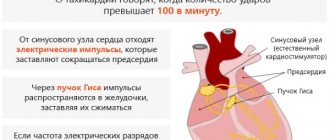
The process of pulse wave formation
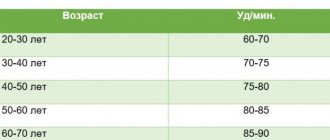
When measuring heart rate, it is very important to determine the indicators that are typical for a person at rest. In this case, fluctuations from 50 to 100 beats per minute are considered normal. For an adult patient, there are certain limits of pulse activity, which depend on the following factors:
- Age. For a young person, a good indicator in a calm state is from 60 to 80. For older people, an increase in pulse fluctuations to 90 or more beats is typical.
- Gender. It is generally accepted that women are more emotional, so even at rest their heart rate is slightly elevated. This condition is especially pronounced after menopause.
- Degree of fitness of the body. For example, athletes are able to control their heartbeat.
Heart rate characteristics
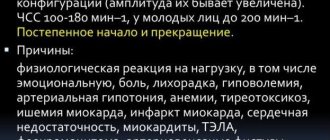
A heart rate of 110 is definitely considered too high. If such an indicator occurs systematically, you should consult a doctor and undergo an examination. If a patient has 110 pulse wave beats per minute, this indicates the development of tachycardia (heart rhythm disturbance). She may be:
- physiological - manifests itself as a reaction to external influences;
- pathological - is a symptom of diseases of internal organs;
- sinus - manifested by a constant increase in pulse to more than 115 beats with a normal rhythm;
- paroxysmal - has a paroxysmal character, begins and goes away unexpectedly.
The normal rate for a person is considered to be a heart rate of up to 90 beats per minute. Excess may be due to external irritants or the presence of a particular disease in the body.
Diagnostics
It is carried out in an outpatient or inpatient setting. Everything goes faster in the hospital. Patient management is the prerogative of the cardiologist. As needed, third-party specialists are involved: neurologist, neurologist, endocrinologist, psychotherapist.
Sample list of studies:
- Oral assessment of health complaints.
- Anamnesis collection. Often doctors neglect the moment. But this is the most important procedure. You need to take the initiative into your own hands and tell as much as possible about the problem and its possible origins.
- Measurement of blood pressure and heart rate. It is carried out using an automatic device or the “old-fashioned” method, using a watch and a stethoscope. Which is not so accurate.
- Electrocardiography. Basic technique. Gives an idea of the nature of functional abnormalities in the work of the heart. It is also possible to differentiate between the types of arrhythmias, the main thing is that the doctors have enough experience.
- Echocardiography. It shows only gross changes, therefore it has minimal information content.
- Blood tests (hormones, biochemistry and general), urine tests.
- Examination of neurological status.
- Angiography.
- CT and MRI.
Depending on the nature of the process, tachycardia should be differentiated into:
- Sinus.
- Supraventricular.
- Ventricular
Based on the results, a therapeutic course is prescribed.
Therapeutic methods
Tachycardia occurs for various reasons, depending on which certain treatment methods are used. Therapy is selected for each patient individually, taking into account his individual characteristics and age.
First aid
Many people do not know what to do when an attack of tachycardia occurs. Do I need to call doctors? Medical attention is required if the following symptoms are present:
- severe pain in the heart area;
- fainting;
- headache;
- a sharp increase in blood pressure;
- pale skin;
- breathing problems;
- bloody vomiting;
- diarrhea in the presence of black stool.
Before the ambulance arrives, the patient should be given first aid. To do this you need:
- Provide the patient with oxygen access.
- Place it in a horizontal position.
- Remove oppressive and confining clothing from the person.
- Take heart drops (Valocordin, Valerian).
- Ask the patient to take a deep breath, hold the air for 5 seconds and exhale. This breathing exercise will help calm your heart activity.
- Cool your face by applying ice or a towel soaked in cold water.
Such manipulations can significantly improve the patient’s condition. Then he will need specialized medical care.
Drug treatment
The use of medications to normalize heart rhythm is the most effective method of therapy. The most commonly used means are:
Sedatives. They can be plant-based (Persen, Novopassit, tincture of valerian, motherwort) or synthetic (Phenazepam).- Drugs with antiarrhythmic effects. Among them are Verapamil, Metoprolol.
- Vitamin complexes.
- Potassium and magnesium supplements.
But the most important thing is to eliminate the cause of the tachycardia. For this, the patient undergoes a thorough examination. After a survey and examination, he is prescribed the following diagnostic methods:
- biochemical and hormonal blood analysis;
- electrocardiogram;
- ultrasound examination of the heart and blood vessels;
- Magnetic resonance imaging.
Additional consultation with a cardiologist, endocrinologist, neurologist, infectious disease specialist and psychiatrist may also be required.
It should be remembered that tachycardia is a symptom that indicates a malfunction in the body. If you get rid of the cause, problems with heart rhythm will disappear.
Treatment options
Determined by the type of pathological process. However, these are subtleties.
The approximate diagram is always the same:
- Use of medications.
- Using folk recipes.
- Surgical correction.
- Lifestyle changes.
Drug treatment
Several groups of drugs are indicated:
- Cardiac glycosides to normalize organ activity. Lily of the valley tincture.
- Beta blockers. Reduce the sensitivity of specific receptors to adrenaline and other substances: Carvedilol, Anaprilin.
- Calcium channel blockers. They prevent blood vessels from narrowing, normalizing blood pressure and, at the same time, heart rate. Diltiazem and Verapamil.
- Herbal sedatives. Motherwort and Valerian.
- Tranquilizers. Calm the nervous system and inhibit its activity. Diazepam and analogues.
- Potassium and magnesium preparations (Magne B6, Magnelis, Asparkam). Prescribed to nourish the heart muscle.
Using folk recipes
Only as a help. Not the main method at all.
- Honey with lemon (a tablespoon 2 times a day or more).
- Chokeberry tincture (200 g of berries per 400 ml of vodka or alcohol, take 2 teaspoons 2 times a day).
- St. John's wort, motherwort, valerian, mint, chamomile in tea form. 100 g of mixture per 300 ml of water. A glass 1 time per day or more, as needed.
Surgery
For congenital and acquired defects of a muscular organ, tumors, advanced stage atherosclerosis, thrombosis, destruction of the atria, persistent tachycardia (installation of a pacemaker). They resort to this technique in extreme, hopeless cases.
Lifestyle change
- Quitting smoking and alcohol.
- Normalization of sleep (8 hours per night).
- Drinking regime: 1.8 liters per day.
- 2 hours of walking during the day.
Diet optimization
Can:
- Vegetables, fruits (especially potatoes, apricots, bananas, apples and carrots).
- Lean meat and broths, soups.
- Cereal porridge
- Natural sweets.
- Nuts.
- Eggs.
- Dairy products.
- Oils (butter and vegetable).
- Kissels, berry decoctions.
- Coarse bread.
- Fish.
It is forbidden:
- Canned food.
- Semi-finished products.
- Chocolate.
- Tea.
- Coffee.
- Energy.
- Fast food.
- Salt over 7 grams per day.
- Muffins, fried pies and similar products.
- Fat meat.
Cooking method: boiling, steaming, baking. Frying, especially in oil, is prohibited or strictly limited. It is necessary to observe the principle of fractionalization: more often is better, less. You can’t eat at all at night (2-3 hours before bedtime).
Treatment tables No. 3 and No. 10 are shown, with limited amounts of salt and liquid. You can create a menu yourself or contact a nutritionist. The approximate one is already ready, all that remains is to adjust it.