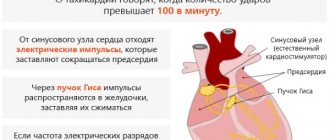
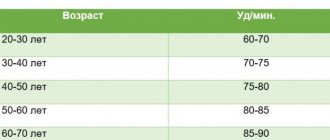
A rapid heartbeat of 100 beats per minute attracts the attention of doctors, since it exceeds the norm, which for a healthy adult is 60-80 beats. It is considered absolutely normal for a person without heart pathologies if he does not feel his heartbeat. Increased heart rate during arrhythmia is called tachycardia; this condition requires normalization.
Causes of rapid heartbeat
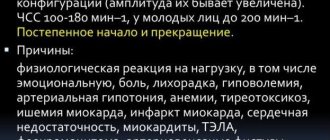
If a person is at rest, then it is considered normal when he does not feel his own heartbeat. Tachycardia (increased heart rate above 100 beats per minute) can occur in healthy people under the following circumstances:
- strong emotional experiences;
- increased physical activity;
- changes in environmental parameters - lack of oxygen in the air;
- fever - with an increase in body temperature by 1 degree, the heartbeat increases by an average of 10 beats/minute.
In such situations, tachycardia does not indicate the presence of heart disease, but is a normal physiological reaction of the body.
The presence of physiological tachycardia is noted when hormonal levels change - in women during menopause. Sometimes the heart begins to beat faster due to an allergic reaction or after eating a large meal. Eating foods rich in caffeine is another cause of tachycardia.
The key feature of physiological tachycardia is the absence of accompanying symptoms:
- increased blood pressure;
- burning or pain in the heart area;
- dizziness and darkening of the eyes;
- fainting state;
- panic attack.
When the heart rate increases due to external factors, normalization of the heart rate occurs within a few minutes - for this it is enough to assume a state of rest.
During active physical activity, you should monitor your own pulse and be able to calculate the maximum heart rate. To do this, you need to subtract your own age from the number 220. So, for a 40-year-old person during sports training, the pulse should not exceed 180 beats per minute.
For a person leading a sedentary lifestyle, any physical effort (change of body position, sudden standing up) can cause an attack of tachycardia. In such cases, you can get rid of increased heart rate only through gradual and feasible training.
Is there a connection between pulse and blood pressure?
In any critical situation, in order to assess the severity of a person’s condition, I primarily focus on blood pressure and pulse numbers.
Blood pressure and pulse are closely related. Thanks to their regulation, normal blood supply to all internal organs is ensured.
In a physiological sense, the pulse always “adjusts” to the pressure value. For example, when blood pressure decreases, the heart rate increases compensatoryly to maintain blood circulation at the proper level.
However, if the pulse is too fast (pathological), the diastole time (the phase of the cardiac cycle during which the chambers of the heart fill with blood) decreases. As a result, when the ventricles contract, less blood is released into the systemic circulation, which leads to a decrease in blood pressure and a deterioration in general circulation.
Tachycardia as a symptom of the disease
Tachycardia at normal pressure can be caused by:
- obesity;
- diabetes;
- diseases of the stomach, thyroid gland.
The causes of tachycardia in women of physiological type are observed during menopause, with hormonal changes in the body and a decrease in estrogen levels. Estrogen stimulates the autonomic nervous system, affects the intestines, breathing, and heartbeat. For this reason, during menopause, when the concentration of estrogen decreases, the following symptoms of tachycardia occur in women:
- dizzy;
- shortness of breath appears;
- hot flashes occur;
- feeling of pulsation and fluttering in the chest.
The cause of the pathological disease is cardiac, vascular problems, disruptions in the functioning of other systems. The main extracardiac factors include:
Advertising:
- psoriasis;
- dehydration of the body;
- blood loss;
- temperature during a sore throat.
Often, when the disease is tachycardia, the causes may be pain syndromes of various origins and an increase in temperature. Frequent heartbeat can be observed in most heart and vascular diseases.
- Heart attack.
- Myocarditis, pericarditis.
- Heart defects.
In the case of idiopathic increased heart rate, it is impossible to determine the obvious factors of the disturbed rhythm. Therefore, if there is a rapid heartbeat, having eliminated the causes, treatment will be aimed at combating the disease.
When blood pressure changes, most patients feel worse. If the condition is not controlled in a timely manner, there is a high risk of sudden death and hypertensive crisis. Read more in the article: “Ascophene: increases or decreases blood pressure.”
How to diagnose tachycardia
With sinus tachycardia, when the increase in contractions of the heart muscle is associated only with external factors, a special examination, as a rule, is not required. But in cases where the increase in the number of heartbeats is not a consequence of stress or increased physical activity, it is necessary to undergo a number of manipulations to help diagnose tachycardia:
- electrocardiogram (ECG) - to determine the level and rhythm of contractions of the heart muscle at the time of the study;
- 24-hour Holter monitoring – helps to find out how the heart rate changes over a 24-hour period during physical activity, with low mobility and during sleep;
- Ultrasound examination of the heart, echocardiography – detects pathological abnormalities in the functioning of the heart.
Blood pressure must be measured; in addition, bicycle ergometry may be prescribed (hardware monitoring of the performance of the cardiac system during exercise on an exercise bike).
Rapid heartbeat can be caused not only by cardiac pathology, but also by other diseases of the internal organs. Therefore, in addition to specialized studies, it is advisable to take blood tests (biochemistry, electrolyte content, thyroid hormones) and urine.
Diagnostics
It is carried out primarily by a specialized cardiology specialist. Then, if necessary, by third-party doctors.
A sample list of studies is as follows:
- Assessment of complaints, their nature and duration. Helps determine the likely root cause pathology.
- Anamnesis collection. Lifestyle, bad habits, family history, medication use, somatic diseases and other factors.
- Blood pressure measurement.
- Listening to heart sounds.
- Electrocardiography. Basic technique. Provides comprehensive information about the functional state of the type of tachycardia.
- Echocardiography. A visual way to study organ structures.
- Blood tests (general, biochemical, thyroid hormones, adrenal cortex, pituitary, reproductive), urine (clinical, according to Zimnitsky, if necessary).
- It is possible to conduct stress tests for dynamic monitoring of the onset of tachycardia. But with great caution.
A study of the degree of dysfunction and the nature of the disorders is shown. There are 3 types of heart rate increases:
- Sinus.
- Supraventricular.
- Ventricular.
It is possible to select based on other criteria. Paroxysmal tachycardia is of greatest individual interest, since the treatment for this condition is different.
First aid for an attack
Advertising:
The first step is to create maximum rest conditions for the patient (half-sitting or lying down), unbutton his clothes to ensure a flow of fresh air. It should be noted that those around the patient should express calm and not cause panic. A person having an attack should take a deep breath and hold it, and then exhale slowly.
The most common service in dentistry is prosthetics. If the dentist performs it correctly, a person’s teeth will become straight and their smile will be attractive. Read more in the article: “repairing dentures at home.”
By performing such breathing exercises, the attack can be stopped. Emergency care for tachycardia can be as follows: changing the patient’s body position from horizontal to vertical and vice versa, straining for 50 seconds, inducing a gag reflex, Usher’s test (pressure on the eyeballs).
It should be noted that pressing on the eyeballs is not recommended if emergency care is provided for paroxysmal tachycardia in children, as this action may result in retinal detachment. If the first emergency aid for an attack of tachycardia does not work, drug methods should be used.
Take sedatives: 40-50 drops of valocardine, motherwort or valerian preparations and others (thus, emergency assistance can be provided for sinus tachycardia). When emergency care is provided for tachycardia, you must immediately call an ambulance.
Emergency care for ventricular tachycardia should be provided by qualified specialists, as it involves administering intravenous injections. Injections are given with antiarrhythmic drugs, cardiac glycosides, and sometimes electrical pulse therapy can be used.
Emergency care for supraventricular tachycardia with a medical approach is very quickly eliminated by using antiarrhythmic drugs (as a rule, the patient himself can know which drug will help him), but you can try to cope on your own without using serious medications.
Drug treatment
The sinus variety is treated in the system. Medicines that can be used if the pulse is 100 or more:
- Sedatives. Calms the central nervous system and reduces heart rate. Diazepam, Motherwort, Valerian, Phenobarbital in various preparations.
- Calcium channel blockers. They do not allow Ca+ ions to penetrate into the structures of blood vessels and cause their stenosis. Hence the impossibility of rapidly increasing heart rate.
- Magnesium-based products (Magnelis, Magne B6). Helps normalize cardiac activity.
- Beta blockers. Used to relieve irritation of the third reflex zone of the organ. Can be used as emergency aid.
Supraventricular tachycardia:
- Additionally, cardiac glycosides are prescribed.
- Antiarrhythmic drugs.
Ventricular arrhythmia is treated much more seriously, since it is the most dangerous and lethal type. The same groups of media are used, but strictly in combination.
How to reduce heart rate?
When the pulse quickens for no apparent reason, it causes fear and anxiety. The main thing in such a situation is not to be nervous and try to determine what is happening in the body. If tachycardia remains the only symptom, you should breathe deeply and remain calm. Warning signs may include pain in the heart area that radiates to the neck or arm, as well as numbness and trembling of the limbs. In most cases, they are absent, and you can calm your heartbeat at home quickly, thanks to several useful methods.
Advertising:
In many home medicine cabinets you can find drugs to reduce heart rate. They are available without a doctor's prescription and will help you quickly restore your performance. However, before taking them, it is important to find out the cause of this symptom, since different groups of drugs have different compositions and are indicated for tachycardia of different origins. So, the doctor may recommend the following medications:
- Valocordin, Corvalol
- drugs based on phenobarbital and plant extracts, available in the form of drops that need to be diluted in water; - valerian officinalis
- comes in the form of drops and tablets, it helps well with tachycardia caused by nervous tension; - rosehip or hawthorn fruits, motherwort root
- raw materials for the preparation of soothing decoctions, useful for calming the heartbeat; - if necessary
, medications to replenish potassium or magnesium deficiency (Asparkam, Panangin).
After taking medications, you should avoid physical activity. It is better to spend this day in a calm environment, avoiding stress and nervous tension.
Video - Rapid heartbeat. How to calm your heart
What does the heart need?
Of all the chemical elements, the heart needs most:
- iodine (products containing it have a beneficial effect on metabolism: these are sea fish, squid, shrimp, seaweed and other gifts of Neptune),
- potassium (it improves the activity of the heart muscle, promotes the removal of excess fluid: most of it is found in potatoes, pumpkin, cabbage, apricots, prunes, dried apricots, figs, rose hips, black and red currants, parsley),
- magnesium (this element has a calming, vasodilating and diuretic effect, maintains the tone of the walls of blood vessels, and therefore do not neglect porridges: oatmeal, millet, barley, buckwheat, as well as walnuts, peas, beets, carrots, salad; wheat bran is rich in magnesium, soy flour, sweet almonds, bananas.American scientists have concluded that those who receive at least half a gram of magnesium daily (that’s how much it is contained in one banana) have a minimal risk of heart attack).
Advertising:
And another gastronomic addiction of your heart is dairy and vegetarian soups: from cereals, vegetables. Do you remember the last time these dishes were on your table?
Traditional medicine to normalize heart rate
Along with medications, traditional medicine recipes can also prevent increased heart rate. Most often, medicinal plants are used in the treatment of tachycardia, which contain natural glycosides and herbs with a calming effect.
| Product name | Ingredients and preparation | Mode of application |
| Viburnum and cranberry balm | Viburnum and hawthorn (berries) - 1 kg each. Rose hips, cranberries - 0.5 kg each. Place in layers in a 5-liter container, sprinkle with sugar (you can use honey). Pour vodka to the level of the berries. Leave in a dark place for 21 days | 30 g twice a day - morning and evening. You can use berries from balsam to make compotes |
| Oriental Heart Balm | Lemon (with peel) – 500 grams. Dried apricots, raisins – 500 grams each. Walnuts (kernels) – 500 grams. Grind using a blender, add 1 kg of honey. Store in a cool place | 1 teaspoon per day in the morning |
| Clover tincture | Place fresh clover flowers in a container (liter jar) and fill with vodka. Infusion time: 30 days in a dark place | 1 teaspoon three times a day, after meals |
Take a medium sized head of garlic and make a paste from it. We put everything in a jar, fill it with unrefined sunflower oil and leave it at home inside the refrigerator for the whole next night. In the morning, cut out the top of a ripe lemon with a knife and squeeze fresh juice into a teaspoon. Let's add a little garlic oil.
Advertising:
We make butter this way. Peel 2 garlic heads and cut them into small pieces. Place in a jar made of any glass and fill with vegetable oil (about half a glass). We store the jar in the sun for 11 days, stirring it every day. After 11 days, filter and add 1 drop of purified glycerin (sold at the pharmacy). Let's put everything into a bottle, but now from darkish-colored glass with a good cork. It belongs in the refrigerator. Treatment at least three times in one day. The course is usually allowed for up to 90 days.
Prevention of tachycardia
The best method for preventing tachycardia is to reduce the risk of developing one of the many heart diseases. It is often because of them that irregularities in the heart rhythm appear. To avoid illness, you should constantly monitor your indicators - this will help you notice any deviations in a timely manner and eliminate the problem at an early stage. To reduce the risk of tachycardia, it is recommended to take simple measures of the following nature:
- Regularly engage in physical training to the best of your ability;
- Lead a healthy lifestyle, including a healthy diet with enough fruits, whole grains and vegetables;
- Limit consumption of fatty foods and quit alcohol, drugs and smoking;
- Maintain body weight in the optimal range for your gender, age, weight and professional activity;
- Control blood cholesterol levels;
- Reduce your consumption of coffee and caffeinated drinks to a minimum.
It is also important to use any medications with great caution. From a young age you need to monitor the normalization of blood pressure, and especially in old age. It is necessary to try to avoid psychological stress. Regular visits to the doctor will help you take preventive measures in a timely manner and prevent the development of tachycardia.
You should be aware that caffeine can have an extremely negative effect on your heart rhythm and lead to arrhythmic conditions. It is impossible to say unequivocally what excessive caffeine consumption is, since it is very individual for each person. For some, a cup of coffee a day will not do any harm, but for others, even one cup a week may do a disservice.
Possible complications
Among the likely consequences of untreated tachycardia:
- Thromboembolism as a result of platelet destruction. The result is delayed death.
- Heart failure. Sudden, uncontrollable and not noticeable during the period before the onset of the condition.
- Heart attack.
- Organ dysfunction due to prolonged overload.
- Cardiogenic shock. The outcome of physical stress against the background of increased heart rate.
- Fainting “out of the blue” with the prospect of injury.