In most cases, an increase in blood pressure is accompanied by increased work of the myocardium, due to which the heartbeat accelerates. However, some hypertensive patients have a low pulse with high pressure, which may indicate the development of concomitant pathologies both from the cardiovascular system and serve as a sign of impaired cerebral circulation. So, if blood pressure readings exceed 145/95 mm. rt. Art., and the heart rate decreases to 60 beats/min., then the patient should consult a specialist to diagnose the cause of the disorder. What are the causes of this disorder and how to independently identify its first signs?
What is "bradycardia"?
A decrease in heart rate (HR) below the established norm (60 beats per minute) is called “bradycardia”.
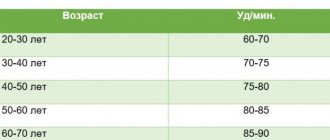
It can occur both in healthy people and in patients with various pathologies. Compared to tachycardia (increased heart rate more than 90 beats per minute), bradycardia is less common. It is typical for people over 60 years of age, since heart disease is more common at this age. Heart rate usually corresponds to the pulse, since with each release of blood into the aorta under pressure, rhythmic vibrations of the arterial walls occur.
What is the normal heart rate?
In adults, the heart rate should be 60–90 beats per minute (bpm); for children, normal heart rates depend on age. Thus, in babies under one year old, heart rate fluctuates between 100–170 beats/min. As the child grows up, normal heart rate values gradually decrease. By age 12–15, your resting heart rate should approach 70–90 beats per minute.
How to measure pulse?
The pulse can be measured by feeling the arteries that are located shallow to the surface of the skin and where they can be pressed against the bones. Then you can feel the movement of the vessel wall with your fingertips (Fig. 1). It occurs with every heartbeat. The pulse is measured in the following arteries: temporal, carotid, brachial, radial (at the wrist), femoral, popliteal, dorsalis pedis, posterior tibial (at the ankle of the foot).
Figure 1. How to measure pulse Source: MedPortal
Physiological and pathological bradycardia
Low heart rate as a physiological phenomenon is typical for professional athletes. Due to constant intense training, the body gets used to increased stress, which affects autonomic regulation. The heart rate naturally slows down in a sleeping person. When the body is at rest, the pulse becomes low and blood pressure decreases. This is the norm. After waking up, when a person begins to engage in vigorous activity, the heart rate increases.
If there is a slowing of the heart rate while awake for unknown reasons, this condition requires the attention of specialists. Most often it is caused by diseases of the cardiovascular or nervous system, endocrine disorders, and injuries. Low heart rate occurs in both adults and children.
Causes of bradycardia
A decrease in heart rate can occur not only with cardiac lesions, but also with non-cardiac pathologies. Common reasons for a decrease in heart rate include:
- coronary heart disease, heart defects, atherosclerotic cardiosclerosis, heart attack, myocarditis, cardiomyopathies, pericarditis;
- jaundice and kidney failure, in which toxins slow the heart's impulses;
- connective tissue diseases (rheumatism, rheumatoid arthritis, scleroderma, lupus erythematosus);
- hypothyroidism - decreased function of the thyroid gland;
- infections (diphtheria, borreliosis, syphilis, toxoplasmosis, viral hepatitis, etc.);
- disturbance of the electrolyte composition of the blood - decreased potassium levels and increased calcium;
- increased intracranial pressure due to brain tumors, stroke, trauma, developmental defects;
- lymphogranulomatosis, multiple myeloma, amyloidosis, sarcoidosis, hemochromatosis are conditions in which myocardial damage is possible.
Drug-induced bradycardia often occurs. This occurs when taking or overdosing on beta blockers, cardiac glycosides, calcium channel blockers, and antiarrhythmic drugs.
The heart rate is affected by the work of the nervous system: the parasympathetic system reduces the heart rate, and the sympathetic system increases it. Reflex bradycardia occurs as a result of the influence of the parasympathetic nervous system on the sinus node. The causes of such bradycardia may be:
- diseases of the nervous system;
- gastrointestinal pathology (peptic ulcer of the stomach and duodenum, cholecystitis, cholelithiasis);
- diseases of the esophagus and diaphragm;
- low body temperature, hypothermia;
- blow to the upper abdomen (up to cardiac arrest);
- pressure on the eyeballs or neck in the area of the carotid artery;
- cough, vomiting.
When the heart rate slows, blood pressure (BP) can be normal, high or low.
Bradycardia with high blood pressure is an uncommon occurrence. It is dangerous due to respiratory arrest, loss of consciousness, risk of blood clots, insufficient blood supply to the brain and heart with the development of stroke and heart attack. The combination of hypertension and bradycardia requires special treatment approaches so as not to aggravate the slowing of the rhythm.
For newborns (especially premature ones), bradycardia can occur against the background of apnea - stopping breathing for more than 20 seconds (Fig. 2). This occurs due to the immaturity of the nervous and muscle tissue of the newborn.
Figure 2. Bradycardia and apnea in infants. Source: MedPortal
What is blood pressure?
Blood pressure, or blood pressure, is the force with which blood presses from the inside onto the walls of blood vessels. Due to the fact that in nature there is also atmospheric pressure, which exerts its influence on all living organisms and objects, blood pressure is the amount by which blood pressure exceeds atmospheric pressure.
Each heartbeat sets the blood in motion, creating upper pressure (systolic) and lower pressure, which is measured at the moment the heart muscle relaxes, that is, in the intervals between beats. This pressure is called diastolic.
Upper pressure shows the force with which the heart, at the moment of compression, pushes blood out of the left ventricle. At this point the highest indicator is noted. As the force of the push is distributed throughout the circulatory system, the pressure loses its original value and a lower value is noted at the entry point into the heart.
At the moment when the heart relaxes after a beat and its valve closes, blood fills the small vessels and capillaries. Pressure may increase during this period due to the response of the arteries to the blood flow. Generally, the higher the systolic pressure, the more resistance the artery walls have. This means that when the upper pressure is high, the lower pressure often increases.
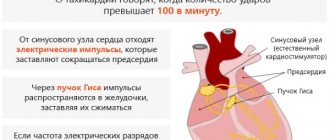
Classification of bradycardia
The work of the heart is impossible without the normal functioning of the conduction system. These are special muscle fibers that form nodes and bundles and provide coordinated contraction of the atria and ventricles of the heart. A normal rhythm is generated with a frequency of 60–90 per minute in the sinus node (SU), which is located in the right atrium. Along the internodal bundles, the electrical impulse is conducted to the atrioventricular node (atrioventricular - AV), located in the interatrial septum. From the AV node, the impulse goes directly to the muscles that provide contraction of the ventricles of the heart.
Depending on the mechanism of occurrence, bradycardia occurs:
- Sinus. Associated with a slowdown in impulse generation in the sinus node itself (Fig. 3).
- Sinoatrial, in which the transmission of impulses from the sinus to the atria is blocked.
- Atrioventricular, when there is a blockade of excitation transmission in the AV node.
Figure 3. Development of sinus bradycardia.
Source: mayoclinic.org Bradycardia can be pathological and physiological - a decrease in heart rate is typical for young athletes and during sleep. Pathological bradycardia occurs:
- acute and chronic;
- with symptoms and without clinical manifestations;
- cardiac and extracardiac (depending on the reasons).
What happens in the body when the heart rate slows down?
Heart rate decreases due to malfunction of the sinus node. It is responsible for the production of electrical impulses, due to which the heart contracts at a physiological frequency. If the sinus node is malfunctioning, the signals are distributed incorrectly along the pathways. This primarily concerns the conduction of electrical impulses between the sinus node and the components of the heart muscle.
With a moderately low heart rate, a person does not notice a pronounced deterioration in well-being. If the heart rate continues to slow down, negative symptoms appear. They are caused by impaired blood supply to tissues. Together with the blood, nutrients and oxygen are supplied to the tissues, therefore, with a prolonged state of low heart rate, a person develops oxygen starvation. Oxygen starvation manifests itself as weakness, lethargy, and other signs of deterioration in health.
A pulse less than 40 beats indicates severe bradycardia. This condition is dangerous for the body due to severe circulatory disorders. The patient is advised to take medication, but in severe cases, drug therapy is not enough, and surgery is performed to install a pacemaker.
Why is bradycardia dangerous?
A decrease in heart rate can cause heart failure, chronic attacks of bradycardia, and the formation of blood clots.
Heart failure
It rarely develops when the decrease in heart rate is significant (less than 40 per minute). Bradycardia results in insufficient cardiac output, which means that the heart can no longer supply oxygen to all organs and systems of the body at the proper level. In this case, the brain and the heart itself suffer first. The risk of developing coronary artery disease and myocardial infarction also increases, and fainting and cardiac arrest may occur.
Blood clots
With prolonged or frequently occurring bradycardia with an irregular rhythm, as a result of slowing down the movement of blood flow in the chambers of the heart, blood thickens and the gradual formation of blood clots occurs. When they enter the vessels of the brain or heart, strokes and heart attacks occur.
Chronic attacks of bradycardia
When the cause of bradycardia cannot be identified and eliminated, attacks occur that reduce the quality of life and are difficult to correct. During an attack, the patient experiences weakness, dizziness, and decreased performance. Sometimes fainting is possible.
What you should never do
- Be physically active. Some particularly active patients begin to do push-ups, run, jump, and breathe heavily. It's too much. Such measures entail excessive stimulation of cardiac activity. If there is a mismatch between needs and possibilities, cardiac overload and tissue ischemia will occur. It’s hard to say how this will end. Nothing good for sure.
- Take unfamiliar drugs. Just what the doctor prescribed. In the absence of recommendations, they are limited to tinctures. They should be in every person's first aid kit.
- Go to the bath, shower. Wash with cold water. Any thermal effect will lead to disruption of vascular tone. A spasm is possible, then cardiac arrest occurs. Or expansion and strengthening of peripheral blood flow with insufficient supply to the myocardium. The outcome is the same.
First aid is aimed at preventing complications and stabilizing the patient's condition. Everything else is the task of the doctors.
Symptoms of bradycardia
Manifestations of bradycardia are caused by a lack of blood supply to vital organs: the brain, heart and lungs. Bradycardia can manifest itself (Fig. 4):
- decrease in blood pressure;
- presyncope and loss of consciousness;
- dizziness, headache;
- rapid fatigue;
- chest pain;
- shortness of breath and poor tolerance to any physical activity;
- pale skin.
Figure 4. Symptoms of bradycardia. Source: MedPortal
Symptoms requiring an ambulance call
Among the characteristic dangerous manifestations:
- Chest pain. Moderate or weak intensity. Not always present.
- Heart rhythm disturbances. Decrease, weakening. There may be a sensation of skipping beats, slowing down, or fluttering.
- Dyspnea. In a state of complete rest. The manifestation intensifies with physical activity.
- Drowsiness, weakness, decreased performance within significant limits.
- Headache, vertigo. Cerebral moments. Indicate insufficient blood circulation to the brain.
- Impaired consciousness. Up to deep repeated fainting during one episode of low pulse.
- Panic, a feeling of fear, impending death or threat. This is a mental reaction of the body to a violation of the conditions of existence. You need to pull yourself together. In the hospital, intravenous sedation with mild drugs (mild tranquilizers) is performed.
- Pale skin in the system with hyperhidrosis, tremor, cyanosis of the nasolabial triangle.
In general, any suspicion should be grounds for calling an ambulance. There is no point in being shy or afraid of overloading doctors with work or taking someone else’s place. The dispatcher ranks cases according to urgency.
When to see a doctor?
If you have symptoms of bradycardia and a pulse less than 60 beats per minute, you should consult a physician or cardiologist. The doctor will determine the causes of this condition and prescribe effective treatment.
Not all bradycardia causes symptoms. However, low heart rates cannot be ignored. A repeated decrease in heart rate is the “first bell” that will force the timely diagnosis of heart disease and non-cardiac pathology, and prevent the development of dangerous complications.
How to quickly increase your heart rate?
If a rare pulse is not a symptom of heart disease and appears for physiological reasons, you can speed it up and eliminate unpleasant symptoms by using simple remedies available in almost every home. Before starting activities, it is important to take into account the circumstances under which the heart rate decreased.
| Initiating factor | How and with what is it manifested? |
| Stress, shock, nervous disorders | If the heart rate decreases to forty beats per minute or below, you can take sedatives:
|
| Decreased blood pressure and pulse | The best option is to take decoctions for:
|
| Increased blood pressure and decreased heart rate | The best solution would be:
|
| Pregnancy |
|
If a person is sufficiently resilient and healthy, physical activity (from running, jumping and squats to cardio exercises) would be a good option.
Diagnosis of bradycardia
Only a doctor can differentiate physiological or pathological bradycardia. To do this, he uses several diagnostic methods.
Auscultation
A simple diagnostic method is to listen to the heart using a phonendoscope. Auscultation of the heart allows not only to determine a rare rhythm, but also to suspect certain diseases of the cardiovascular system.
Electrocardiography
ECG is a method of instrumental diagnostics of the heart, which records not only heart rate, but also helps to diagnose cardiac causes of bradycardia (myocardial ischemia and infarction, sinus node pathology, AV block). This is important for effective therapy. In some cases, daily ECG monitoring is necessary - a Holter study.
Phonocardiography
Phonocardiography (PCG) is a method of hardware diagnostics of sound phenomena that are created during the work of the heart. The study is carried out in conjunction with an ECG. At the same time, the heart sounds that are created during the operation of the valves, as well as additional noise, are assessed.
To diagnose the causes of bradycardia, the doctor may also prescribe:
- EchoCG - ultrasound examination of the heart;
- blood test for markers of damage to the heart muscle (troponins, creatine kinase);
- study of inflammation indicators (C-reactive protein, rheumatic tests, markers of collagenosis);
- blood test for thyroid function indicators (TSH, T4, T3);
- study of blood electrolytes (potassium, magnesium, calcium, sodium);
- biochemical blood test (glucose, bilirubin, cholesterol, creatinine, etc.).
Iron deficiency conditions in gynecological diseases and methods for their correction
Iron deficiency anemia (IDA) is a hematological syndrome characterized by impaired hemoglobin synthesis due to iron deficiency. Anemia is based on tissue hypoxia, which develops as a result of a decrease in the amount of hemoglobin due to blood loss, impaired formation of red blood cells, their destruction, or a combination of these reasons [1, 2].
Iron deficiency occurs in almost 1/3 of the world's inhabitants, and iron deficiency anemia accounts for 80–90% of all anemias. The prevalence of anemia varies depending on gender, age, climatic-geographical and environmental-industrial causes [1, 3, 4].
A corresponding deficiency develops when iron losses exceed iron intake of 2 mg/day, and is observed in various physiological conditions and diseases [5, 6].
Iron deficiency (hypochromic, microcytic) anemia usually occurs due to a decrease in iron resources in the body due to chronic blood loss or insufficient external iron supply.
The most vulnerable to the development of iron deficiency are women of reproductive age due to monthly physiological blood loss during menstruation, pregnant women due to their high need for microelements, children and adolescents due to the high needs of a growing body, elderly people suffering from chronic diseases and having poor nutrition.
Iron is an essential microelement that plays an important role in the functioning of cells in many body systems, the main of which is the participation of iron in the processes of tissue respiration. The total amount of iron in a woman’s body reaches 2–3 g, and its concentration is 40–50 mg per kg of body weight.
There are two types of iron: heme and non-heme. Heme iron is part of hemoglobin, is found only in meat products, is easily absorbed, and its absorption is practically not affected by the composition of food.
Non-heme iron is found in free ionic form - ferrous or ferric iron. The absorption of non-heme iron (found primarily in vegetables), which accounts for up to 90% of the iron in the total diet, depends on a number of factors. The main part of iron is included in hemoglobin and myoglobin - 70%; iron depot - 18% (intracellular accumulation in the form of ferritin and hemosiderin); functioning iron - 12% (myoglobin and iron-containing enzymes); transported iron - 0.1% (iron bound to transferrin) [7–9].
The most important iron-containing compounds include: hemoproteins, the structural component of which is heme (hemoglobin, myoglobin, cytochromes, catalase, peroxidase), non-heme enzymes (succinate dehydrogenase, acetyl-CoA dehydrogenase, xanthine oxidase), ferritin, hemosiderin, transferrin.
In the mucous membrane of the small intestine, only divalent non-heme iron is absorbed from food. In order for iron to contact proteins and enter the cell, ferric iron is reduced to divalent iron in the presence of an acidic environment; in most cases, ascorbic acid plays the main role in this process [10–13]. Then, to enter the blood plasma and bind to transferrin, iron is again oxidized to trivalent. In the transferrin-bound state, iron is delivered to tissues through endocytosis, where it is either utilized by the cell or deposited in ferritin. Ferritin stores iron in an easily accessible and non-toxic form. Ferritin level is the “gold” standard indicator of the amount of stored iron in the body. Each microgram of ferritin corresponds to 8 mg of deposited iron and for women is normally 15–150 mg/ml [2, 14–16]. The concentration of serum iron is subject to significant daily fluctuations and averages 6.6–26 µmol/l in women. Therefore, its definition is not of paramount importance [2].
Hemoglobin is an oxygen transport protein containing heme iron. The hemes are combined into a protoporphyrin framework, in the center of which there is one divalent iron atom. One hemoglobin molecule can carry a maximum of 4 oxygen molecules. Thus, the number of red blood cells and hemoglobin plays an important role in oxygen transport [2].
During iron deficiency, successive stages are distinguished: latent iron deficiency, in which iron losses exceed iron intake without changes in hemoglobin concentration, and iron deficiency anemia itself, which, depending on the severity, is divided into compensated, subcompensated and decompensated forms [3].
Hemoglobin concentration is expressed in grams per liter. The normal hemoglobin level in women is considered to be 115-145 g/l (MCHC, Mean Corpuscular Hemoglobin Concentration - the average concentration of hemoglobin in a cell is 320-360 g/l); anemia is indicated when hemoglobin decreases below 110 g/l. The severity of anemia is judged by the level of hemoglobin. According to the severity of anemia, there is a mild degree - 90-109 g/l, a moderate degree - 70-89 g/l and a severe degree - less than 70 g/l [3, 14, 15].
In addition, iron deficiency anemia is characterized by a decrease in hematocrit, hypochromia (MCH, Mean Corpuscular Hemoglobin - the average absolute content of hemoglobin in one erythrocyte), microcytosis (MCV, Mean Corpuscular Volume - the average volume of an erythrocyte), hyposiderosis (a decrease in the amount of serum iron, an increase in total iron-binding ability of blood serum, decrease in ferritin level in blood serum and in hemolysate) [3, 5]. The number of red blood cells, hematocrit and hemoglobin constitute the measured values, and MCV, MCH, MCHC are derivatives of these values [2].
The clinical picture of anemia is caused by oxygen starvation of tissues, progressive hemic hypoxia with the subsequent development of secondary metabolic disorders. Clinical symptoms appear as the severity of the disease increases: general weakness, dizziness, headache, palpitations, shortness of breath, fainting, decreased performance, insomnia. Symptoms characteristic of IDA include changes in the skin, nails, hair, muscle weakness, and distortion of the sense of taste. The skin becomes dry and cracks appear on it. Due to impaired carotene metabolism, iron deficiency causes yellowness of the skin. The shape of the nails changes, they flatten, become concave and brittle. Hair becomes thinner, breaks and falls out profusely, and gray hair appears. With IDA, symptoms of damage to the cardiovascular system are also possible: palpitations, shortness of breath, chest pain and sometimes swelling in the legs [6, 14].
The main compensatory mechanisms are circulatory and ventilatory adaptation, including an increase in cardiac output, vasodilation, a decrease in vascular resistance, an increase in tissue perfusion, blood redistribution, an increase in minute volume of respiration, and an increase in erythropoietin activity. Acute, severe and uncompensated anemia can lead to circulatory collapse and shock [2].
The main cause of the development of iron deficiency anemia in women is blood loss of various etiologies. Iron deficiency is 6 times more common in women than in men. A significant amount of blood is lost during menstruation, pregnancy, and childbirth. With heavy menstruation, iron loss of 50–250 mg of iron is possible [2]. Most often, hyperpolymenorrhea is associated with the presence of uterine fibroids, adenomyosis, hyperplastic processes of the endometrium, and dysfunctional uterine bleeding. Metrorrhagia with uterine fibroids is most often associated with submucosal localization of nodes, in which the menstrual surface increases, the permeability of blood vessels supplying the fibroids increases, and the contractility of the uterus decreases. With fibroids, the regeneration of the bleeding surface of the uterus slows down after desquamation of the endometrium. With adenomyosis, the uterine myometrium is affected, which leads to prolonged heavy menstruation and secondary iron deficiency anemia.
Menstrual irregularities occur in women at different ages. Various reasons can lead to the development of hypermenstrual syndrome - severe emotional shocks, malnutrition, vitamin deficiencies, obesity, occupational hazards, infectious and septic diseases, immaturity of hypothalamic structures in puberty and involutive changes in premenopause. In a significant proportion of cases of menometrorrhagia in women, they are accompanied by anemia of varying severity, which contributes to the development of trophic disorders in various organs and tissues. Prevention and treatment of anemia in women with menstrual irregularities and organic gynecological diseases are the most important factors in restoring their health [1, 4, 17].
Regardless of the cause of menometrorrhagia (fibroids, endometriosis, ovarian dysfunction) and the need to influence the corresponding factor, long-term therapy with iron preparations for oral administration is required. The dose, dosage regimen and specific drug are selected individually, taking into account the iron content in the drug, its tolerability, etc.
When choosing a specific drug and the optimal dosage regimen, it is necessary to keep in mind that an adequate increase in hemoglobin levels in the presence of IDA can be ensured by the intake of 30 to 100 mg of ferrous iron into the body [18]. Dietary measures alone cannot compensate for iron deficiency and achieve a therapeutic effect.
Antianemic therapy should be carried out with oral medications and should not be stopped after hemoglobin normalization. Indications for parenteral administration are quite limited: intestinal pathology with malabsorption, intolerance to oral drugs, social reasons (use in patients with personality changes, the mentally ill). According to many studies, parenteral forms do not have advantages over oral ones, and a large number of serious side effects are noted [4, 10, 19]. Blood transfusions for IDA should be carried out only for health reasons.
Modern oral ferrous preparations are salts of ferrous iron (ferric ions are not absorbed in the digestive tract) or compounds consisting of a hydroxide-polymaltose complex of ferric iron (the absorption mechanism differs from that of ionic preparations) [20].
Ferric sulfate salt has the highest bioavailability, therefore ferrous sulfate is mainly contained in ferrous preparations [19, 21]. Ferrous sulfate is the most studied, proven form, which has proven itself with long-term use, therefore it is most often included in preparations for oral administration. It has the highest degree of absorption of all iron preparations.
In the process of absorption of divalent iron in the intestine, ascorbic acid is of great importance, which helps maintain iron in divalent form, so its presence in the preparation is very important [22]. In hematopoiesis, folic acid plays a significant role, enhancing nucleic acid metabolism. For normal folic acid metabolism, cyanocobalamin is necessary, which promotes the formation of its active form. Deficiency of these substances, which often occurs in anemia associated with blood loss, leads to disruption of DNA synthesis in hematopoietic cells, while the inclusion of these components in the drug increases the active absorption of iron in the intestine and its further utilization. The presence of ascorbic and folic acids, as well as cyanocobalamin in the drug significantly increases the rate of hemoglobin synthesis and increases the effectiveness of therapy for iron deficiency conditions and iron deficiency anemia [14, 23, 24].
The listed components that increase the bioavailability of iron are part of the complex antianemic drug Ferro-Folgamma® [24], which was developed and produced in accordance with the recommendations of the World Health Organization (1998).
1 capsule contains 112.6 mg of ferrous sulfate (elemental iron 37 mg), which is the optimal dose for therapy and reduces the incidence of side effects.
Absorption of iron from salt preparations (Fe2+) occurs in the form of passive diffusion according to a concentration gradient, does not depend on pH and motor activity of the gastrointestinal tract (GIT), which ensures rapid saturation.
Ascorbic acid improves the absorption of iron in the intestine, prevents its transition from divalent to trivalent form, accelerates the transport of iron and its inclusion in heme, and also participates in the process of releasing iron from the depot.
Ascorbic acid is necessary for the formation and preservation of the reduced form of folic acid - tetrahydrofolic acid.
In turn, folic acid is an essential factor for the synthesis of DNA and RNA, protein metabolism and the formation of red blood cells, and also acts as an additional stimulator of erythropoiesis and hematopoiesis [21, 23, 25].
Cyanocobolamine is necessary for the formation of hemoglobin, red blood cells, metabolism of proteins, fats, carbohydrates, and energy production.
Ferro-Folgamma® is highly effective, providing an average increase in hemoglobin of 2.5 g/l/day (the highest rate of increase in hemoglobin among ferrous sulfate preparations). When using the drug Ferro-Folgamma®, a weakening of the clinical symptoms of posthemorrhagic anemia is observed during the first 10 days of use [6].
Ferro-Folgamma® is prescribed 1 capsule 3 times a day after meals for 3–4 weeks for mild forms of anemia, for moderate forms — 1 capsule 3 times a day for 8–12 weeks, and for severe forms of anemia — 2 capsules 3 times a day for 16 weeks or more. During pregnancy, it is prescribed to prevent folic acid and iron deficiency, 1 capsule 3 times a day in the II and III trimesters, in the postpartum period during breastfeeding.
After cessation of treatment with Ferro-Folgamma®, the positive effect and stabilization of blood serum parameters (hemoglobin level, red blood cells, serum iron, total iron-binding capacity of blood serum) are guaranteed to persist for at least one month [4].
The active components of Ferro-Folgamma® are in a special neutral shell, which ensures their absorption in the upper part of the small intestine, which eliminates irritating effects on the stomach. The components are dissolved in rapeseed oil, which improves the absorption of iron and at the same time reduces the irritating effect of iron on the gastric mucosa, promoting good tolerability of the drug in the digestive tract [1, 13]. Due to the absence of an aggressive effect on the gastrointestinal mucosa, Ferro-Folgamma® can be successfully used to correct anemic syndrome, with a deficiency of vitamin B12 and folic acid against the background of impaired absorption in the gastrointestinal tract (atrophy of the gastric and duodenal mucosa).
In addition, Ferro-Folgamma® is effectively used for combined iron-folate-B12-deficiency anemia caused by chronic blood loss, chronic alcoholism, infections, taking anticonvulsants and oral contraceptives, anemia during pregnancy and breastfeeding.
The effectiveness of Ferro-Folgamma® for the treatment and prevention of iron deficiency anemia with good tolerability and favorable pharmacoeconomic characteristics (cost/iron dose/efficacy) was proven in several Russian studies that included a wide range of patients, including pregnant women and women with gynecological diseases [4, 18, 19]. Indications for the use of the drug Ferro-Folgamma® are anemia caused by a combined deficiency of iron, folic acid and vitamin B12, occurring against the background of chronic blood loss (menorrhagia and metrorrhagia, etc.), as well as with chronic alcoholism, infectious diseases, taking anticonvulsants and oral contraceptives. The drug is approved for the prevention and treatment of iron and folic acid deficiency in the second and third trimesters of pregnancy, in the postpartum period and during lactation.
Thus, anti-anemic therapy using the drug Ferro-Folgamma® with optimal iron content is highly effective with a rapid increase in hemoglobin (complete clinical and hematological remission in 93% of patients after 3 weeks of therapy). There is good tolerability - the absence of side effects in 95% of patients, allergic reactions and negative effects on the body of women, as well as the stability of the results achieved and the maintenance of a positive effect for a month after treatment, which makes it possible to recommend the drug Ferro-Folgamma® to a wide range of patients.
Literature
- Transcript of the scientific symposium “Iron deficiency conditions in obstetrics and gynecology.” III Russian Forum “Mother and Child”. M., 2001, 29.
- Hook R., Breiman K. Anemia during pregnancy and the postpartum period. M., 2007, 74.
- Gorodetsky V.V., Godulyan O.V. Iron deficiency conditions and iron deficiency anemia: diagnosis and treatment. Guidelines. M.: Medpraktika-M, 2005; 28.
- Konovodova E. N., Dokueva R. S.-E., Yakunina N. A. Iron deficiency conditions in obstetric and gynecological practice // Breast Cancer. 2011; 20: 1228–1231.
- Dolgov V.V., Lugovskaya S.A., Morozova V.T., Pochtar M.E. Laboratory diagnosis of anemia. M., 2001. P. 84.
- Kozlovskaya L.V. Hypochromic anemia: differential diagnosis and treatment // New Med. magazine 1996; 56:8–12.
- Shekhtman M. M. Guide to extragenital pathology in pregnant women. M., 2005, 816, 373–399.
- Johnson-Wimbley TD, Graham DY Diagnosis and management of iron deficiency anemia in the 21st century // Therap. Adv. Gastroenterol. 2011; 4 (3): 177–184.
- UNICEF/UNU/WHO. Iron Deficiency Anemia: Assessment, Prevention, and Control. A Guide for Program Managers. Geneva: WHO/NHD, 2001.
- Arkadyeva G.V. Diagnosis and treatment of iron deficiency conditions. Educational and methodological manual. M.: 1999: 22–25.
- Burlev V. A., Gasparov A. S. et al. Epocrine in the treatment of iron deficiency anemia in patients with uterine fibroids after hysterectomy // Problems of reproduction. 2003; 6:59–64.
- Kasabulatov N.M. Iron deficiency anemia in pregnant women // Breast cancer. 2003; 11, 1: 18–20.
- Lebedev V. A., Pashkov V. M. Principles of treatment of iron deficiency anemia in gynecological patients // Difficult patient. 2013, 11, 11: 3–7.
- Dvoretsky L.I., Zaspa E.A. Iron deficiency anemia in the practice of an obstetrician-gynecologist // Breastfeeding. 2008; 29.
- Kazyukova T.V., Samsygina G.A., Kalashnikova G.V. et al. New possibilities of ferrotherapy for iron deficiency anemia // Klin. pharmacology and therapy. 2000; No. 9 (2): 88–91.
- Pasricha SR, Flecknoe-Brown SC, Allen KJ et al. Diagnosis and management of iron deficiency anemia: a clinical update // Med. J. Aust. 2010; 193(9):525–532.
- Fernandez-Gaxiola AC, De-Regil LM Intermittent iron supplementation for reducing anemia and its associated impairments in menstruating women // Cochrane Database Syst. Rev. 2011. 12. CD009218.
- Burlev V.A., Konovodova E.N., Ordzhonikidze N.V., Serov V.N., Elohina T.B., Ilyasova N.A. Treatment of latent iron deficiency and iron deficiency anemia in pregnant women // Russian Bulletin of Obstetrics- gynecologist. 2006. No. 1. P. 64–68.
- Vertkin A.L., Godulyan O.V., Gorodetsky V.V., Skotnikov A.S. Iron deficiency anemia and the choice of drug for its correction // Russian Medical Journal. 2010. No. 5.
- Gratsianskaya A.N. Iron deficiency anemia: Ferro-Folgamma // Breast cancer. 2013; No. 29.
- Arvas A., Gur E. Are ferric compounds useful in the treatment of iron deficiency anemia? // Turk J Pediatr. 2000. Vol. 42(4). R. 352–354.
- Teucher B., Olivares M., Cori H. Enhancers of iron absorption: ascorbic acid and other organic acids // Int J Vitam Nutr Res. 2004. Vol. 74(6). R. 403–419.
- Konovodova E. N., Burlev V. A. Ferro-Folgamma + Erythropoietin - new possibilities for the treatment of anemia in patients with uterine fibroids // Farmateka. 2004. No. 15 (92). pp. 70–73.
- Ferro-Folgamma. Therapy with iron, folic acid, vitamin B12 and ascorbic acid. Scientific review. Werwag Pharma. M., 2001.
- Ghinea MM Treatment of iron deficiency anemia with Ferro-Folgamma // Rom J Intern Med. 2004. Vol. 42(1). R. 225–230.
A. Z. Khashukoeva1, Doctor of Medical Sciences, Professor S. A. Khlynova, Candidate of Medical Sciences M. V. Burdenko, Candidate of Medical Sciences M. R. Narimanova O. V. Kozlova, Candidate of Medical Sciences, Associate Professor
GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information
Abstract. The role of Ferrum in the human organism has been analyzed, mechanisms of its digestion from food, clinical presentations of hypoferric conditions and women's hypoferric anemia, as well as approaches to therapy and prophylaxis of hypoferric anemia with modern oral preparations.
Treatment of bradycardia
Not all bradycardia requires treatment. Only a doctor can determine the need for treatment by excluding physiological causes of a decrease in heart rate.
Conservative treatment
For conservative treatment use:
- anticholinergics - drugs that prevent the influence of the parasympathetic nervous system on the heart;
- adrenaline analogues - drugs that stimulate heart rate;
- antiarrhythmic drugs.
Treatment is carried out with tablets and injections. Their doctor can prescribe them occasionally during attacks and for a long time.
Surgery
In cases where conservative treatment is ineffective or there is damage to the conduction system of the heart, surgical treatment is indicated - installation of an electrical pacemaker (pacemaker). This is an electronic device that is implanted subcutaneously in the left subclavian region and sets the necessary rhythm to the heart through electrodes (Fig. 5). The pacemaker not only stimulates impulses to contract the heart, but also controls its natural electrical activity.
Figure 5. Installation of a pacemaker for bradycardia. Source: MedPortal
Treatment with folk remedies
To treat bradycardia at home, infusions of herbs are mainly used, which reduce the tone of the parasympathetic nervous system, increase myocardial contractions, and maintain blood pressure. These are Chinese lemongrass, tartar, immortelle, yarrow, walnuts, a mixture of lemon, honey and garlic and others.
Important! Treatment with folk remedies should be carried out very carefully and only after consultation with a doctor. It is possible with mild degrees of bradycardia (heart rate of at least 40), in the absence of complications and manifestations such as fainting, shortness of breath, dizziness, chest pain.
Therapeutic measures
The main goal of treatment for bradycardia is to increase the heart rate in order to ensure adequate blood supply to the organs. For this purpose, medications are often prescribed whose action is aimed at increasing blood pressure, since these two indicators are closely interrelated. Drugs are prescribed taking into account the reason that provoked the decrease in pulse, the individual characteristics of the body and the age of the patient.
The most commonly prescribed medications include:
- Citramon, Koficil, Askofen contribute to an increase in blood pressure due to the caffeine they contain.
- Atropine hydrochloride has an effect on cardiac tissue receptors and is used in emergency cases.
It is worth understanding that only a qualified specialist can prescribe the most suitable drug to increase the pulse, after receiving the results of the examination.
You should not self-medicate, since illiterate use of any medications can only complicate the course of the disease.
Prevention
To prevent complications of bradycardia, you need to consult a specialist as soon as possible if your pulse decreases and heart rate is less than 60, and undergo a full examination to identify the causes of the condition. It is equally important to strictly follow your doctor's recommendations for treating episodic or prolonged bradycardia.
To prevent bradycardia, it is necessary to adhere to a lifestyle that reduces the risk of heart disease:
- stop smoking and drinking alcohol;
- eat well: limit animal fats, salt, caloric content of food should correspond to energy costs;
- reduce excess weight if you are overweight;
- avoid nervous stress;
- normalize blood pressure.
What can you do at home?
Little. It is not known what caused the violation. Therefore, any amateur activity is excluded. An ambulance is required.
If this is not the first attack of bradycardia and there are doctor’s recommendations, you can limit yourself to basic measures, then visit a specialist as planned.
The general algorithm is:
- Open a window or window to ensure room ventilation and oxygen saturation of the blood. If this is not done, fainting and problems with the central nervous system are possible. The risk of stroke increases.
- Remove tight body jewelry and loosen the collar. Pressure on the carotid sinus will reflexively lead to a drop in heart rate, which will have a fatal effect on hemodynamics.
- Sit down. Relax. Before this, if you have tincture of eleutherococcus or ginseng in your medicine cabinet, take it. Not all together, just one thing. 25-35 drops. This will help increase your heart rate by 10-15 beats.
- Take prescribed medications (if you have consulted a doctor).
Wait for the brigade to arrive. Talk about how you feel. Hospitalization is rarely required, but doctors may suggest this option as a preventative measure. There is no point in refusing.