Sudden cardiac arrest kills about 300,000 people worldwide each year. Once a year, at least, the media reports another death from sudden cardiac arrest: an athlete right on the field during a game or a schoolchild in physical education class. But many people die for the same reason, falling asleep and not waking up.
Like 43
162127
According to the Ministry of Health, in Russia alone, from 8 to 16 people per 10 thousand of the population die annually from sudden cardiac arrest, which is 0.1-2% of all adult Russians. In the whole country, 300 thousand people die this way every year. 89% of them are men. In 70% of cases, sudden cardiac arrest occurs outside the hospital. In 13% - at the workplace, in 32% - in a dream. In Russia, the chances of survival are low - only one person out of 20. In the USA, the likelihood that a person will survive is almost 2 times higher. The main cause of death is most often the lack of timely assistance.
Unfortunately, 22% of patients experience sudden death, the first manifestation of the disease. Sudden death most often occurs in older children and adolescents, but is rare in children under 10 years of age. Approximately 60% of sudden deaths occur at rest, the rest after heavy physical exertion.
- 171
More details - 234
More details
- 234
More details
- 171
More details
Most people who experience sudden cardiac arrest have:
- mental disorders in 45%;
- asthma in 16%;
- heart disease in 11%;
- gastritis or gastroesophageal reflux disease (GERD) in 8%.
Causes of cardiac arrest
Among the causes, one can distinguish directly cardiac (cardiac) and external (extracardiac).
The main cardiac factors are:
- myocardial ischemia and inflammation;
- acute obstruction of the pulmonary vessels due to thrombosis or embolism;
- cardiomyopathy;
- high blood pressure;
- atherosclerotic cardiosclerosis;
- rhythm and conduction disturbances due to defects;
- development of cardiac tamponade with hydropericardium.
Extracardiac factors include:
- oxygen deficiency (hypoxia) caused by anemia, asphyxia (suffocation, drowning);
- pneumothorax (the appearance of air between the layers of the pleura, unilateral compression of the lung);
- loss of a significant volume of fluid (hypovolemia) due to injury, shock, persistent vomiting and diarrhea;
- metabolic changes with a deviation towards acidosis;
- hypothermia (hypothermia) below 28 degrees;
- acute hypercalcemia;
- severe allergic reactions.
Indirect factors that influence the stability of the body’s defenses are important:
- excessive physical stress on the heart;
- elderly age;
- smoking and alcoholism;
- genetic predisposition to rhythm disturbances, changes in electrolyte composition;
- suffered electrical trauma.
A combination of factors significantly increases the risk of cardiac arrest. For example, drinking alcohol in patients with myocardial infarction causes asystole in almost 1/3 of patients.
Pathogenesis
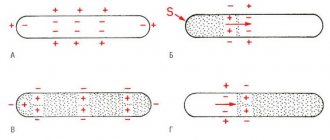
Cardiac arrest is based on shifts in the gas composition of the blood and acid-base balance towards oxidation, which leads to disruption of metabolic processes, inhibition of conductivity, changes in excitability in the heart muscle and, as a result, disruption of the contractile function of the myocardium. A wide range of pathologies, different causes and types of contributing factors form different mechanisms of cardiac arrest. The cessation of cardiac activity may be based on different types of cardiac arrest, the main of which are: cardiac asystole and ventricular fibrillation .
What is cardiac asystole? Asystole means the complete cessation of contractions of the muscles of the atria and ventricles in the genesis of which is the complete cessation of the process of transfer of excitation from the sinus node in the absence of impulses in secondary foci of automaticity. This includes:
- asystole of the entire heart with impaired/complete blockade of conduction between the sinus node and the atria;
- ventricular asystole in the presence of complete transverse block;
- pronounced ventricular bradycardia against the background of incomplete blockade of conduction between the ventricles and atria.
Asystole can occur reflexively (suddenly) with still preserved myocardial tone or gradually (with preserved myocardial tone or with its atony). Cardiac arrest most often occurs in diastole and is much less common in systole. In Fig. The ECG below shows an agonal rhythm turning into asystole .
Ventricular fibrillation is understood as an asynchronous (chaotic and scattered) contraction of the muscle fibers of the heart, leading to disruption of the function of blood supply to organs and tissues. In this case, vigorous fibrillary contractions are observed (with normal myocardial tone) or sluggish (with its atony).
The main mechanism of cessation of blood circulation in most cases (85%) is ventricular fibrillation, the development of which is facilitated by factors that reduce the electrical stability of the myocardium: decreased cardiac output, increased heart size ( aneurysm , hypertrophy , dilatation ), increased sympathetic activity.
The cause of ventricular fibrillation is disturbances in the conduction of excitation in the conduction system of the ventricles. The preliminary stages of cardiac fibrillation are:
- ventricular fibrillation and flutter;
- paroxysmal tachycardia , which is caused by impaired intraventricular/intraatrial conduction.
In Fig. Below is an ECG for large-wave and small-wave ventricular fibrillation.
There are several theories to explain the mechanisms of heart rhythm disturbances during fibrillation, the most significant of which are:
- The theory of heterotopic automatism, which is based on the appearance of numerous foci of automatism that arise as a result of “overexcitation” of the heart.
- The theory of "ring" rhythm. According to its provisions, excitation continuously circulates throughout the myocardium, which leads to contraction of individual fibers instead of simultaneous contraction of the entire muscle.
An important mechanism for the occurrence of ventricular fibrillation is the acceleration of the excitation wave. In this case, only muscle fibers contract, which by that time had left the refractory phase, which causes chaotic contraction of the myocardium.
Also, disturbances in electrolyte balance (potassium and calcium) are of great importance in the development of pathology. Under conditions of a hypoxic state, intracellular hypokalemia , which in itself increases the excitability of the heart muscle, which is fraught with the development of paroxysms of disruption of sinus rhythm. Also, against the background of intracellular hypokalemia, myocardial tone decreases. However, cardiac activity is disrupted not only with the development of intracellular hypokalemia, but also with a change in the ratio/concentration of K+ and Ca++ cations. Such disorders lead to changes in the cell-extracellular gradient with a disorder in the processes of excitation/contraction of the myocardium. In addition, a rapid increase in plasma potassium concentration against the background of its reduced level in cells can cause fibrillation. Intracellular hypocalcemia can also contribute to the loss of the myocardium's ability to fully contract.
In general, regardless of the genesis of SCD, cardiac arrest must be based on a factor leading to the occurrence of SCD and disability of the heart muscle. The BCC formula can be presented as: BCC = substrate + trigger factor.
Where the substrate refers to anatomical/electrical abnormalities caused by heart disease, and the trigger factor refers to metabolic, mechanical and ischemic influences.
What happens during cardiac arrest
After a few seconds from its beginning, the following develops:
- weakness and dizziness;
- after 10-20 seconds - loss of consciousness;
- after another 15-30 seconds, so-called tonic-clonic convulsions develop, breathing is rare and agonal;
- at 2 minutes clinical death occurs;
- pupils dilate and stop responding to light;
- the skin turns pale or takes on a bluish tint (cyanosis).
The chances of survival are slim. If the patient is lucky and there is a person nearby who can perform chest compressions, the likelihood of surviving sudden cardiac arrest syndrome increases. But for this it is necessary to “start” the heart no later than 5-7 minutes after it stops.
Prevention
General nonspecific measures to prevent cardiac arrest include:
- Timely diagnosis and treatment of diseases of the cardiovascular system.
- Control blood pressure and cholesterol levels.
- Quitting alcohol abuse and smoking.
- Moderate physical activity.
- Rational and balanced nutrition.
- Monitoring the correct intake of medications.
- Elimination of hypothermia, extensive injuries with large blood loss.
Diagnostic signs of cardiac arrest
Cardiac arrest syndrome includes early signs of clinical death. Since this phase is considered reversible with effective resuscitation measures, every adult should know the symptoms, since a few seconds are allotted for reflection:
- Complete loss of consciousness - the victim does not respond to shouting or braking. It is believed that the brain dies 7 minutes after cardiac arrest. This is an average figure, but the time can vary from two to eleven minutes. The brain is the first to suffer from oxygen deficiency; the cessation of metabolism causes cell death. Therefore, there is no time to speculate on how long the victim’s brain will live. The earlier resuscitation is started, the greater the chance of survival.
- Inability to detect pulsation in the carotid artery - this diagnostic sign depends on the practical experience of others. If it is absent, you can try to listen to heartbeats by placing your ear to your bare chest.
- Impaired breathing - accompanied by rare noisy breaths and intervals of up to two minutes.
- “Before our eyes” there is an increase in the change in skin color from pallor to blueness.
- The pupils dilate after 2 minutes of cessation of blood flow, there is no reaction to light (constriction from a bright beam).
- Manifestation of cramps in individual muscle groups.
If an ambulance arrives at the scene of the incident, then asystole can be confirmed by an electrocardiogram.
All probiotics are the same
Probiotics are live microorganisms that are very beneficial to the body if taken in reasonable quantities. By probiotics, many people mean bacteria, but this effect can be exerted not only by bacteria, but by different microorganisms.
Probiotics are available in different forms - fermented foods, dietary supplements, pharmaceutical preparations. Some supplements contain one strain of bacteria, others contain several. Moreover, each drug has its own functions and mechanism of action. It is important not to confuse probiotics with prebiotics.
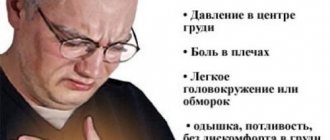
Signs of imminent sudden cardiac arrest
Danish scientists analyzed cases of sudden death from cardiac arrest. And it turned out that even before it stopped, the heart made it known that something was wrong with it.
35% of patients with sudden arrhythmia death syndrome had at least one symptom suggestive of heart disease:
- fainting or near-fainting - in 17% of cases, and this was the most common symptom; chest pain;
- dyspnea;
- The patient had already undergone successful resuscitation of cardiac arrest. Likewise, 55% of people who died from hypertrophic cardiomyopathy, more than 1 hour before their sudden death, experienced: fainting (34%);
- chest pain (34%);
- shortness of breath (29%).
American researchers also point out that every second person who suffered sudden cardiac arrest experienced manifestations of cardiac dysfunction - and not an hour or two, but in some cases several weeks before the critical moment. Thus, chest pain and difficulty breathing 4 weeks before the attack were noted by 50% of men and 53% of women, and in almost all (93%) both symptoms occurred 1 day before sudden cardiac arrest.
Only one in five of these people consulted doctors. Of these, only a third (32%) managed to survive. But from the group that did not seek help at all, even fewer survived - only 6% of patients. The difficulty of predicting sudden death syndrome also lies in the fact that not all of these symptoms appear at the same time, so it is impossible to accurately track a critical deterioration in health.
74% of people had one symptom, 24% had two, and only 21% had all three.
So, we can talk about the following main signs that may precede sudden cardiac arrest:
- Chest pain: from an hour to 4 weeks before the attack.
- Difficulty breathing, shortness of breath: from an hour to 4 weeks before the attack.
- Fainting: shortly before the attack.
If these signs are present, you should contact a cardiologist and undergo an examination.
Classification
Cardiac arrest is distinguished by:
- cause of heart disease (sudden cardiac death), among which, depending on the time interval between the onset of a heart attack and the onset of death, instantaneous (almost instantly) and rapid cardiac death (within 1 hour) are distinguished.
- non-cardiac causes (rupture of an aneurysm of large vessels, drowning, thromboembolism of the pulmonary artery or cerebral vessels, airway obstruction, electric shock , shock of various etiologies, embolism, drug overdose, exogenous poisoning, etc.).
What are the consequences of cardiac arrest?
The consequences of circulatory arrest depend on the speed and correctness of emergency care. Long-term oxygen deficiency of organs causes:
- irreversible foci of ischemia in the brain;
- affects the kidneys and liver;
- With vigorous massage in elderly people and children, fractures of the ribs, sternum, and the development of pneumothorax are possible.
The mass of the brain and spinal cord together constitutes only about 3% of the total body mass. And for their full functioning, up to 15% of the total cardiac output is required. Good compensatory capabilities make it possible to preserve the functions of nerve centers when the level of blood circulation decreases to 25% of normal. However, even chest compressions can only maintain 5% of normal blood flow.
Consequences from the brain can be:
- partial or complete memory impairment (the patient forgets about the injury itself, but remembers what happened before it);
- blindness is accompanied by irreversible changes in the visual nuclei, vision is rarely restored;
- paroxysmal spasms in the arms and legs, chewing movements;
- different types of hallucinations (auditory, visual).
Why does the brain need oxygen?
Gray matter makes up only 2% of body weight, but it uses about 20% of oxygen. Without it, the brain cannot perform even the most basic functions. The brain relies on glucose to stimulate neurons that control everything from conscious functions like planning and thinking to automatic, unconscious processes like heart rate and digestion.
Without oxygen, the cells of this organ cannot metabolize glucose and therefore cannot convert glucose into energy. When your brain is deprived of oxygen, the ultimate cause of brain death is insufficient energy to fuel the cells.