What are cardiovascular diseases?
Cardiovascular diseases (CVD) are the leading cause of mortality in many economically developed countries, including Russia, accounting for 55% of total mortality.
According to statistics from recent years, in the structure of mortality from CVD, 85.5% are due to ischemic heart disease (46.8%) and cerebral stroke (38.7%). In the Russian Federation in 2000, the mortality rate from diseases of the circulatory system was 800.9 per 100,000 thousand population. The main cause of cardiovascular disease is atherosclerosis. And although it is impossible to eliminate many risk factors for the development of atherosclerosis, we can change, for example, our lifestyle and diet.
Natural age-related “wear and tear” of blood vessels creates conditions for cholesterol deposition inside and on the walls of arteries. This leads to a gradual narrowing of the lumen of the blood vessels and reduces the ability of the heart to pump blood through them to the body. The moment the vessel is completely blocked, a heart attack (myocardial infarction) or stroke occurs if the blockage occurs in a vessel in the brain. It is important to note that high blood cholesterol does not always have an unfavorable prognosis. The fact is that cholesterol is associated with proteins - proteins, together they make up lipoproteins. So, cholesterol can be in high (HDL-CHOL.) and low (LDL-CHOL.) density lipoproteins. Cholesterol in HDL-CHOL. prevents the progression of atherosclerosis - “beneficial lipoproteins”, and cholesterol in LDL-CHOL. promotes the progression of atherosclerosis.
What diseases can electrocardiography (ECG) tell about?
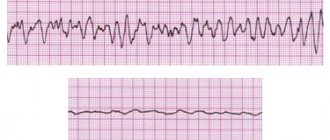
An electrocardiogram (ECG) is considered the main diagnostic method for identifying various diseases of the cardiovascular system. Our heart works in the body under the control of its own pacemaker, which produces electrical impulses and directs them to the conduction system, and they are recorded on the ECG. It turns out that using an electrocardiogram, we can record a peculiar language of our myocardium. Based on the deviations of the main teeth: P, Q, R, S and T, it is possible to determine which disease is the basis of cardiovascular pathology.
Hypertrophy of the heart
Hypertrophy of the heart chambers occurs as a result of hemodynamic disturbances in the bloodstream, which provoke overload of the ventricles or atria. On the ECG you can see seven main signs of cardiac muscle hypertrophy:
- An increase in the time of internal deviation, since in the hypertrophied myocardium the excitation spreads longer in the area from the endocardium to the epicardium.
- An increase in the amplitude of the R wave, while the excitation vector is larger in magnitude.
- Ischemia of the subendocardial layers of the heart, due to the fact that they lack blood flowing through the coronary arteries.
- Conduction disturbance.
- Deviation of the electrical axis of the heart towards the hypertrophied section, as its mass increases due to the growth of cardiomyocytes.
- Changes in the electrical position of the heart.
- Displacement of the transition zone (V3), manifested by a change in the ratio of the R and S waves in the third chest lead.
Angina pectoris
The disease is characterized by attacks of anginal pain lasting from a few seconds to twenty minutes. This disease is one of the formischemic heart diseases. In the classic form of angina pectoris, electrocardiographic signs are manifested by changes in the final part of the ventricular QRS complex:
- Depression of the S-T segment.
- Various changes in the T wave, such as decreased amplitude, biphasicity, isoelectricity, or negativity.
- The focal nature of these changes: they are recorded in one or two leads, since the observed hypoxia is local in nature, developing in the basin of a separate branch of the coronary artery.
During the periods between attacks, the ECG often shows no pathological changes at all. In addition, the above-described deviations are possible in many other heart diseases and pathological conditions. That is why in some cases the diagnosis of angina pectoris can be difficult.
Arrhythmia
Pathology of the cardiovascular system associated with a violation of the formation of an excitation impulse or its spread throughout the myocardium. In most cases, it manifests itself as an interruption in the rhythm of heart contractions, with periods of acceleration and gradual deceleration. Typically, your heart rate increases as you inhale and decreases as you exhale. The features of the ECG are as follows:
- The frequency of changes in the R - R intervals is more than 0.1 seconds.
- Unlike other rhythm disturbances, there is a gradual change in the duration of the R – R interval, usually due to the T – P segment.
- Small fluctuations of P – Q and Q – T are characteristic.
The most reliable electrocardiographic sign of sinus arrhythmia is considered to be a gradual periodic shortening of the R - R section against the background of an increased rhythm and, conversely, a lengthening of the R - R intervals when the rhythm slows down.
Tachycardia
An increase in heart rate is called tachycardia. In this case, the heart rate accelerates to 100-150 beats per minute. A similar disorder can develop due to increased automatism of the sinus node. The pathology is also inherent in healthy individuals during physical exertion or emotional stress. The cause is often ischemia, dystrophic changes, various infections and toxic effects. Main ECG signs:
- There is a decrease in the R–R interval as the T–P interval shortens.
- With severe tachycardia, the P–Q segment shortens.
- The degree of increase in heart rate is directly proportional to the decrease in Q – T.
- An upward displacement of the RS – T segment downward from the isoelectric line.
- The amplitude and direction of the teeth correspond to the norm.
Bradycardia
A deviation that is manifested by a reduced heart rate (less than 60 per minute). It occurs with reduced automatism of the sinus node; it can occur even in healthy people, for example in athletes, when exposed to various factors. A common cause is considered to be an increase in the tone of the vagus nerve. The electrocardiographic picture, in principle, differs little from the norm, only the rhythm is slowed down. The following changes are noted on the ECG:
- The R interval increases due to the T – P shift.
- Q – T increases according to the decrease in rhythm frequency.
- The amplitude and vector of the teeth change slightly.
Heart aneurysm
A cardiac aneurysm is an enlargement of the myocardial cavity due to pathological changes in the muscle layers or abnormalities in the development of the organ at the stage of embryogenesis. The main signs of a cardiac aneurysm include protrusions in its area due to thinning of the wall, which can rupture. This is what can lead to irreparable consequences, which ECG research helps prevent. There are two leading signs that allow you to diagnose an aneurysm:
- The QS wave is present in leads where high R is usually recorded.
- A “frozen” ECG curve: instead of Q, a dome-shaped RS-T segment appears, shifted upward from the isoline, and sometimes a negative coronary T-wave appears.
Extrasystole
Extrasystole is the most common heart rhythm disorder. The pathology develops due to the appearance of an active heterotopic focus capable of generating an electrical impulse that interrupts the work of the sinus node. Manifested by extraordinary excitation and subsequent contraction of parts of the heart or its entirety:
- On an ECG, extrasystoles differ in shape, relation to the isoline, location of the P wave or width, direction of the QRST complex teeth.
- The presence of an increased pause (compensatory) after the extrasystole.
- Atrial extrasystole is characterized by: interval R(c)-R(e) <interval R(c)-R(c), there is a wave P(e), different from the wave P(c), an incomplete compensatory pause.
- The signs of ventricular extrasystole are as follows: interval R(s)—R(e) <interval R(s)—R(s), the P(e) wave is absent, the QRS complex is deformed, a complete compensatory pause.
Pulmonary embolism
Pulmonary embolism is accompanied by the development of pulmonary heart syndrome, since the resulting hypertension of the pulmonary circulation leads to acute overload of the right ventricle. In this case, the myocardium is in a state of hypoxia, and its hypertrophy develops. All of the above determines several ECG options for pulmonary embolism:
- SI-QIII-TIII syndrome: deep S waves in standard I and Q waves in leads III, while T waves in lead III become negative.
- acute hypertrophy of the right parts of the heart muscle, which is manifested by a high pointed P wave in standard lead II.
- acute supraventricular tachyarrhythmias.
In some cases, with acutely developing cor pulmonale, metabolic changes in the area of the right ventricle provoke the occurrence of complete or partial blockade of the right bundle branch.
Pericarditis
The dynamic picture of the ECG during pericarditis depends on its etiology. However, there are also common characteristics, for example: inflammation of the pericardial tissue changes its electrical status, which leads to the emergence of so-called “inflammatory currents” coming from the heart. It is these “currents” that are recorded by the electrode located above the myocardial area:
- This is graphically displayed on the ECG by the rise of the S-T segment in all leads (concordant rise of the S-T segment).
- There is no displacement of the RS segment – Tbelow the isoline level.
- Pathological Q-waves do not appear dynamically.
The above differences form and disappear in the case of acute pericarditis much more slowly than in the case of myocardial infarction. The appearance of effusion in the pericardial cavity is accompanied by a noticeable decrease in the voltage of all electrocardiographic waves, especially in the leads from the limbs of the subject.
Myocarditis
In all cases of myocarditis, parenchymal inflammation occurs and progresses in the wall of the ventricles, which is focal or diffuse in nature, affecting a certain area of the heart muscle:
- The total T vector tilts in the direction opposite to the affected area, and a low or negative T wave is displayed on the ECG.
- The S–T vector is directed towards the lesion.
- The RST segment is displaced up and down from the isoelectric line.
- Negative T can become symmetrical in acute myocarditis, it becomes pointed, as in coronary insufficiency. The localization of all noted disorders depends on the location of the inflammatory reaction.
These electrocardiographic shifts are best determined in the chest leads. A concomitant pathology is rhythm and conduction disturbances.
Myocardial dystrophy
Myocardial dystrophy is part of the complex of pathological clinical symptoms of menopausal hormonal changes in older people. The pathology is described by pain in the heart area, different from angina pectoris, and a disturbance in heart rhythm. There are cases when these symptoms occur before the onset of menopause. The most common electrocardiographic signs are the following:
- A negative but not deep “coronal” T wave or it may be biphasic with a negative second phase.
- Dynamic changes in electrocardiographic data.
- A slight shift of the RS – T segment downward from the position of the isoelectric line.
- More pronounced changes in the middle chest and right leads.
The main problem of ECG diagnostics is that many deviations and changes in the electrocardiographic picture are similar for a number of diseases. For example, coronary insufficiency, some forms of myocarditis and myocardial dystrophy are characterized by similar electrocardiograms. As practice shows, clinical symptoms need to coincide with the dynamics of ECG abnormalities. In this regard, it is important to note the development of the promising direction presented in the Kardi.ru project. The technique of monitoring the state of your heart allows you to register micro changes in the work of the heart muscle even before the appearance of serious disorders, which is displayed graphically by the CardiRu device and facilitates timely decision-making on appropriate therapeutic measures.
Risk factors for cardiovascular disease
Some risk factors for cardiovascular disease are potentially reversible or can be changed. They include:
- Smoking cigarettes
- Elevated LDL (low density) cholesterol levels
- High triglyceride levels in the blood
- Low HDL (high density) cholesterol
- Overweight
- Large waist circumference (“apple shape”)
- High blood pressure
- Sedentary lifestyle
- Diabetes
Diet and cardiovascular disease
Making small changes to your diet is one of the easiest and most effective ways to reduce your risk of heart disease. You can do it like this:
- Reducing fat in your diet, especially saturated fat and trans fat
- More fruits and vegetables, whole grains and soluble fiber
- Drinking alcohol in moderation
- Reducing salt to maintain lower blood pressure
Cholesterol and cardiovascular disease
Because there is a proven direct link between high blood cholesterol and your risk of heart disease, reducing the amount of fat in your diet, especially saturated fat, can help lower your blood cholesterol. According to the official recommendations of the European Society of Atherosclerosis, “normal” levels of fatty fractions in the blood are: 1. Total cholesterol - less than 5.2 mmol/l. 2. Low-density lipoprotein cholesterol (LDL) - less than 3-3.5 mmol/l. 3. High-density lipoprotein cholesterol (HDL) - more than 1.0 mmol/l. 4. Triglycerides - less than 2.0 mmol/l. People with average energy expenditure should consume no more than 70g of fat per day and less than 20g of saturated fat.
The most common diseases of the cardiovascular system
Diseases of the cardiovascular system are widespread among the adult population of many countries around the world and occupy a leading place in overall mortality statistics. A person who does not have a medical education should at least understand in general terms what a particular heart or vascular disease is, so that if one suspects its development, he does not waste precious time, but immediately seeks medical help. That is why we bring to your attention this article, which reflects the signs of the most common diseases of the cardiovascular system.
Atherosclerosis
Atherosclerosis is a chronic, steadily progressing disease of arteries of predominantly large or medium caliber, which is the main cause of the development of various diseases of the heart and blood vessels.
This disease has now become an epidemic, causing about 50% of all deaths. Atherosclerosis begins at a young age and constantly progresses. In persons over 60 years of age, changes in the vascular wall, characteristic of one or another stage of atherosclerosis, are present in 100% of cases.
The cause of atherosclerosis is a violation of lipid metabolism in the body.
Risk factors for developing this disease are as follows:
- Non-modifiable (that is, those that the patient cannot influence): age (women over 55 years of age or younger during early menopause, men over 45 years of age); male gender; hereditary predisposition (early development of atherosclerosis in close relatives).
- Modifiable (those that the patient can, if desired, eliminate): smoking - regardless of the number of cigarettes smoked per day; high blood pressure – above 140/90 mm Hg. Art.; diabetes; body mass index more than 30 – obesity; especially - abdominal type of obesity - waist circumference in women is more than 88 cm, in men - more than 102 cm.
- Partially reversible: Changes in the biochemical blood test (the level of total cholesterol in the blood is more than 5.2 mmol/l, low-density lipoprotein (LDL in the analysis form) is more than 4.1 mmol/l or less than 0.9 mmol/l.
- Other factors: alcohol abuse; physical inactivity (low physical activity); taking oral contraceptives; unfavorable psychosocial environment – social isolation, depression, stress; drinking soft water.
Disorders of lipid metabolism, expressed in increased levels of cholesterol and triglycerides in the blood, trigger a number of pathophysiological mechanisms, which result in damage to the inner lining of the arteries and endothelium. This leads to platelets sticking to the damaged area, forming an atherosclerotic plaque. This plaque gradually increases in size, increasingly clogging the lumen of the vessel, and the organs that this vessel supplies with blood experience a lack of oxygen. The plaque can rupture, leading to thrombosis (blockage by a blood clot) - this mechanism underlies unstable angina, myocardial infarction and sudden death.
Coronary heart disease (CHD)
IHD is an extremely important medical problem because it is characterized by extremely high prevalence and mortality.
More than half of deaths from cardiovascular diseases are due to ischemic heart disease. Every fifth man aged 50-59 years suffers from this pathology, and morbidity and mortality rates are becoming higher every year.
Coronary heart disease is a disease caused by atherosclerotic damage to the heart vessels - the coronary arteries, leading to an imbalance between the supply and demand of the heart muscle for oxygen - the development of myocardial ischemia.
Factors that increase the risk of developing coronary heart disease are:
- Main factors: imbalance of lipids in the blood; high blood pressure; smoking; diabetes; complicated heredity (sudden death or myocardial infarction in close relatives under the age of 55 years for men and 65 years for women).
- Minor factors: excess body weight; hormone replacement therapy after early menopause; taking oral contraceptives; psychosocial factors; infectious factors (cytomegalovirus, chlamydia, Helicobacter pylori); alcohol abuse; left ventricular hypertrophy; changes in the biochemical blood test (increased levels of triglycerides, lipoprotein, fibrinogen, homocysteine, procoagulants, the presence of inflammatory markers).
There are 6 forms of coronary heart disease, differing in the mechanism of development and features of the clinical course:
- Sudden coronary death. This form is defined as death that occurs in the presence of witnesses, instantly or within 60 minutes from the onset of acute symptoms, preceded by a sudden loss of consciousness, in a healthy person or a sick person, but in satisfactory condition. The main risk factor for this form of coronary artery disease is dysfunction of the left ventricle of the heart.
- Angina pectoris. A form of ischemic heart disease characterized by attacks of chest pain in response to myocardial ischemia, which occurs due to exposure to factors that provoke it. The main provoking factor is physical activity (both industrial work and everyday stress - lifting weights, walking down the street, climbing stairs). An angina attack can also be triggered by psycho-emotional stress, caused not only by negative, but also by positive emotions. Less commonly, the causes of an attack include sexual intercourse, excess food intake, exposure to cold (both general and local), overexertion during bowel movements - if the patient is constipated. If medical attention is not provided, angina will progress and lead to unstable angina.
- Unstable angina. This form of coronary artery disease includes new-onset, progressive and post-infarction angina. This is a period of exacerbation of coronary heart disease, characterized by an increase in the severity of painful attacks and is a leading risk factor for the development of large-focal myocardial infarction.
- Acute myocardial infarction (MI). One of the most dangerous cardiovascular diseases and diseases of internal organs in general. It is characterized by extremely high mortality - the frequency of acute MI among men over 40 years of age ranges from 2-6 cases per 1000 people. Every year about 500,000 people die from this pathology. Myocardial infarction is a condition that occurs as a result of a sudden cessation of coronary blood flow due to thrombosis of a coronary vessel and the development of foci of necrosis (death) in the heart muscle. If emergency care is not provided in a timely manner, and in some cases even when it is provided, the disease ends in the death of the patient.
- Cardiosclerosis. Morphologically, it represents small areas of replacement of cardiac muscle tissue with connective tissue. Essentially these are scars. Cardiosclerosis develops after acute diseases of the heart muscle (for example, after a heart attack) or against the background of chronic heart pathology (for example, with myocardial dystrophy). Areas replaced by scar tissue are unable to perform their function and can cause arrhythmias, heart valve defects, and chronic heart failure.
- Painless form of ischemic heart disease. Temporary disruption of the blood supply to the myocardium in the absence of signs of angina. At moments of ischemia, in some cases it is possible to register changes on the ECG characteristic of ischemic heart disease. The risk of acute myocardial infarction or sudden death in people suffering from silent myocardial ischemia is very high, since they are unaware of their disease, and therefore do not attempt to treat it.
Arterial hypertension
Persistently high blood pressure is one of the most common cardiovascular diseases; it has acquired the proportions of a non-infectious epidemic.
Every third adult in the world has high blood pressure, that is, suffers from one of the forms of arterial hypertension.
According to the WHO (World Health Organization), arterial hypertension is constantly elevated blood pressure: systolic - above 140 mm Hg. Art., diastolic – above 90 mm Hg. Art. The blood pressure level at diagnosis should be determined as the average of two or more measurements during at least two examinations by a specialist on different days. Essential hypertension, or essential hypertension, is high blood pressure in the absence of an obvious reason for its increase. Accounts for about 95% of all cases of arterial hypertension.
The main risk factors for this disease are the same factors that contribute to the development of ischemic heart disease and atherosclerosis, and the course of hypertension is aggravated by the following accompanying pathology: diabetes mellitus; cerebrovascular diseases - ischemic or hemorrhagic strokes, transient ischemic attack (TIA); heart diseases – myocardial infarction, angina pectoris, heart failure; kidney diseases - diabetic nephropathy, chronic renal failure; peripheral arterial disease; retinal pathology – papilledema, hemorrhages, exudates.
If a patient suffering from hypertension does not receive therapy that helps lower blood pressure, the disease progresses, hypertensive crises occur more and more often, which sooner or later can cause all sorts of complications: acute hypertensive encephalopathy; pulmonary edema; myocardial infarction or unstable angina; stroke or transient ischemic attack; arrhythmias; aortic dissection; acute renal failure; eclampsia - in pregnant women.
Secondary, or symptomatic, hypertension is a persistent increase in blood pressure, the cause of which can be determined. It accounts for only 5% of cases of arterial hypertension.
Of the diseases that lead to increased blood pressure, the most frequently diagnosed are: damage to kidney tissue; adrenal tumors; diseases of the renal arteries and aorta (coarctation); pathology of the central nervous system (brain tumors, encephalitis, polyneuritis); blood diseases (polycythemia); pathology of the thyroid gland (hypo-, hyper-, hyperparathyroidism) and other diseases. Complications of this type of arterial hypertension are the same as with hypertension, plus complications of the underlying disease that provoked hypertension.
Heart failure
A frequently occurring pathological condition, which is not an independent disease, but is a consequence, outcome of other acute and chronic heart diseases.
In this condition, due to changes in the heart, its pumping function is disrupted - the heart is unable to supply all organs and tissues with blood. Complications of heart failure are: arrhythmias; congestive pneumonia; thromboembolism; liver cirrhosis and liver failure; chronic renal failure (the so-called “stagnant kidney”); cardiac cachexia (exhaustion); cerebrovascular accidents.
Acquired heart defects
Acquired heart defects occur in approximately 1-10 people per 1000 population, depending on the region of residence, and account for about 20% of all heart lesions of an organic nature.
The main reason for the development of acquired heart defects is rheumatic damage to the valves: 70-80% of all defects are pathology of the mitral valve, the second place in the frequency of damage belongs to the aortic valve, stenosis and/or insufficiency of the tricuspid valve and pulmonary valve are relatively rarely diagnosed. This pathology affects people of different age groups. Every 2nd patient with heart disease requires surgical treatment.
The essence of the disease is that, under the influence of etiological factors, the heart valves lose the ability to function normally: stenosis is a narrowing of the valve, as a result of which it does not allow enough blood to pass through, and the organs experience a lack of oxygen, or hypoxia; insufficiency - the valve leaflets do not close completely, as a result of which blood is thrown from the part of the heart located below to the part located above; the result is the same - the organs and tissues of the body do not receive the vital oxygen they need, and their function is impaired.
Complications of heart defects include many conditions, among which the most common are acute pulmonary edema, infectious bronchopulmonary complications, chronic circulatory failure, atrial fibrillation, thromboembolism and others.
Myocarditis
Myocarditis is an inflammatory disease of the heart muscle caused by infection, infestation of parasites or protozoa, physical or chemical factors, or occurring in autoimmune, allergic diseases, as well as after heart transplantation.
The prevalence of myocarditis is 4-11% of diseases of the cardiovascular system. Myocarditis is especially often diagnosed during a control ECG after a viral infection.
Clinically, myocarditis is manifested by attacks of chest pain, signs of valve pathology, symptoms of arrhythmias, and circulatory disorders. May be asymptomatic. The prognosis for this disease depends on the severity of its course: mild and moderate forms, as a rule, result in complete recovery of the patient within 12 months after the onset of the disease, while severe forms can lead to sudden death, refractory circulatory failure and thromboembolic complications.
Cardiomyopathies
Cardiomyopathies are independent, steadily progressing forms of damage to the heart muscle of unclear or controversial etiology.
Within 2 years, about 15% of patients die from some forms of this disease in the absence of symptoms, and up to 50% in the presence of symptoms corresponding to the disease. They are the cause of death in 2-4% of adults, and are also the leading cause of sudden death in young athletes.
The probable causes of cardiomyopathies are: heredity; infection; metabolic diseases, in particular glycogenosis; lack of certain substances in the diet, in particular selenium, thiamine; pathology of the endocrine system (diabetes mellitus, thyrotoxicosis, acromegaly); neuromuscular pathology (muscular dystrophy); exposure to toxic substances - alcohol, drugs (cocaine), certain medications (cyclophosphamide, doxorubicin); diseases of the blood system (some types of anemia, thrombocytopenia).
Clinically, cardiomyopathies are manifested by all sorts of symptoms of cardiac dysfunction: angina attacks, fainting, palpitations, shortness of breath, cardiac arrhythmias. Cardiomyopathy is especially dangerous due to the increased risk of sudden death.
Pericarditis
Pericarditis is an inflammation of the layers of the lining of the heart - the pericardium - of infectious or non-infectious etiology. Areas of the pericardium are replaced by fibrous tissue, and exudate accumulates in its cavity. Pericarditis is divided into dry and exudative, acute and chronic.
Factors that cause pericarditis are: viral or bacterial infection; mushrooms; parasites; metabolic disorders (renal failure, uremia); heart diseases – myocardial infarction, myocarditis; trauma – with damage directly to the pericardium; autoimmune diseases - acute rheumatic fever, rheumatoid arthritis and others.
Clinically manifested by chest pain, shortness of breath, fever, muscle pain, combined with signs of the underlying disease. The most serious complication of pericarditis is cardiac tamponade - the accumulation of fluid (inflammatory or blood) between the layers of the pericardium, preventing normal contractions of the heart.
Infective endocarditis
It is an inflammatory lesion of valve structures with subsequent spread to other organs and systems, resulting from the introduction of a bacterial infection into the structures of the heart.
This disease is the 4th leading cause of death in patients from infectious pathology. In recent years, the incidence of infective endocarditis has increased significantly, which is associated with the wider spread of surgical interventions on the heart. It can occur at any age, but it most often affects people between 20 and 50 years of age. The ratio of incidence between men and women is approximately 2:1.
Infective endocarditis is a potentially life-threatening disease, so timely diagnosis, adequate, effective treatment and rapid identification of complications are extremely important to improve the prognosis.
Arrhythmias
Heart rhythm disturbances are not separate diseases, but are manifestations or complications of any pathological conditions associated with heart disease or non-cardiac pathology.
They can be asymptomatic for a long time, and can pose a danger to the patient’s life.
There are many types of arrhythmias, but 80% of them are due to extrasystole and atrial fibrillation.
Clinically, arrhythmias are manifested by a feeling of interruptions in the functioning of the heart, dizziness, shortness of breath, weakness, a feeling of fear and other unpleasant symptoms. Their severe forms can provoke the development of cardiac asthma, pulmonary edema, arrhythmogenic cardiomyopathy or arrhythmic shock, and also cause sudden death of the patient.
Which doctor should I contact if I feel unwell? If you have pathology of the cardiovascular system, you need to consult a cardiologist.
Proper nutrition and lifestyle
Trans fats are fats containing trans isomers of unsaturated fatty acids. They are naturally present in small quantities in the meat and milk of ruminants. They are produced from vegetable oils using a special treatment method - hydrogenation: hydrogen is passed through liquid vegetable oil heated to high temperatures. The result is a solid fat mass that is resistant to oxidation. It is used to make margarines, confectionery and cooking fats, which are used to improve the taste and extend the shelf life of food products. Because these fats are cheap and easy to use, they are found in almost all industrially produced foods. Trans fats can also be formed during deep frying. Hydrogenated vegetable fats have recently been frequently introduced into many food products and are completely unjustifiably advertised as dietary fats. These fats behave in the human body like real fats of animal origin - they increase cholesterol levels and accelerate the aging process of the arteries. This type of fat is used to prepare products such as corn flakes, potato chips, and they are used in semi-finished products - pizzas, battered products, muffins, cookies, and candies.
When reducing the fat content in food, it is important not to exclude from the diet “heart-healthy” fats (mono- and polyunsaturated fats), mainly found in vegetable fats and seafood (fish oil).
How to change the ratio of fats in your diet:
- Use butter and spreads (butter substitutes) sparingly
- Choose lean meat
- Use grilling, steaming or baking meats. Avoid frying.
- Replace saturated fats such as butter with unsaturated oils such as sunflower, canola or olive oil
- Limit consumption of trans fats (such as margarine) for cooking
- Eat fatty fish (eg sardines, mackerel, fresh tuna, salmon)
Essential fatty acids (Omega-3, Omega-6). Previously known as vitamin F. Vitamin F is important for the cardiovascular system: it prevents the development of atherosclerosis, improves blood circulation, and has cardioprotective and antiarrhythmic effects. Polyunsaturated fatty acids reduce inflammatory processes in the body and improve tissue nutrition. Essential fatty acids are found in fatty fish. For heart health, you need to eat two servings of fish per week, one of which should be fatty.
Stanols and sterols
Plant sterols and stanols are the so-called phytoesterols - insignificant in content, but very important elements of the cell wall of plants. They are found in small amounts in some vegetable oils, nuts, grains, beans, fruits and vegetables. Plant sterols and stanols help lower blood cholesterol levels. Phytoesterols are added to foods - margarines, mayonnaise, yoghurts, orange juice, breakfast cereals, and much more. These fortified foods may be beneficial for people with high blood cholesterol. Clinical trials have shown that with regular use, they can reduce high blood cholesterol levels.
Fruits and vegetables
Fruits and vegetables are rich in many important nutrients, including vitamins C, E, and carotenoids (antioxidants). They may help protect the heart by limiting the harmful effects of cholesterol on body tissue. This confirms the need for daily inclusion of vegetables and fruits in the diet.
Whole grains and fiber
Research has shown that diets rich in whole grains can reduce the risk of heart disease by 30 percent. It is important to include whole grains at every meal, choosing wholemeal bread and using appropriate types of pasta and rice. Soluble dietary fiber found in oats and legumes can help lower LDL (low-density lipoprotein) cholesterol levels. These foods should be included as part of an overall healthy, balanced diet at least two to three times a week. Soy protein. Recommending a diet that includes at least 25 grams of soy per day has been associated with a reduction in cholesterol and cardiovascular disease. Soy isoflavones, in particular, reduce the risk of cardiovascular disease because they inhibit the growth of cells that form when arteries become clogged with atherosclerosis. Soy protein is also an excellent meat substitute and is available in a convenient and tasty form in many ready-made meals. Another good source of protein is soy milk and yogurt.
Rest and relaxation
While exercise can help lower blood pressure and strengthen the heart, rest and relaxation can reduce anxiety and improve your stress response. We all have to deal with situations such as divorce, bereavement, job loss or financial problems from time to time. There are also everyday events (traffic on the way to work, an argument with your partner, or a disagreement with someone at work) that can lead to stress—these everyday annoyances have an even greater impact because they are constant. Ways to cope with stress - Keep a journal - take note of stressful situations and how you responded to them. This will help you change how you react to stress in the future - Stay positive: Be in control of your feelings. Listen to your emotions. Replacing negative thoughts with positive ones will help you cope with stressful situations more calmly. — Learn to relax, pay attention to your posture, master yoga techniques, massage, meditation, etc. — Restore and regulate your sleep. Each person requires a different number of hours of sleep to feel rested. Try to get enough sleep every night.
Smoking
One of the most important steps you can take to reduce your risk of heart disease is to quit smoking. Smokers under 50 are five times more likely than non-smokers to die from coronary heart disease. Quitting smoking will reduce the risk of not only cardiovascular disease, but also lung diseases such as cancer and chronic obstructive pulmonary disease (COPD). Your doctor may prescribe nicotine replacement therapy or, for example, acupuncture to help you.
Infectious heart diseases
Gilmanshina Diana Ralifovna
Cardiologist, general practitioner
Infectious lesions of the heart
are a category of diseases whose existence many do not even think about, however, the clinical manifestations of such conditions force them to consult a doctor immediately.
Depending on the level of damage, infectious heart diseases are classified as follows:
• Endocarditis
– damage to the inner lining of the heart, epithelial, as well as the valvular apparatus of the heart.
• Myocarditis
– damage to the middle, muscular layer of the heart.
• Pericarditis
- damage to the outer, serous membrane of the heart, that is, the pericardial sac.
• Pancarditis
– damage to all layers of the heart, an extremely serious and rare condition, which most often acts as a complication of endocarditis, myocarditis or pericarditis.
The main causative agents of infectious heart diseases:
•
Adenovirus.
It is one of the most common viral respiratory tract infections leading to myocarditis in both children and adults.
• Cytomegalovirus (CMV).
It is a virus from the same group as the herpes simplex, chickenpox and Epstein-Barr viruses. CMV can be detected in 50-80% of people over 40 years of age. Cytomegalovirus can live in the human body for years without causing harm. But under a certain set of circumstances it becomes active and poses a danger to the tissues of the heart too.
• Coxsackievirus group B
- an enterovirus and the cause of half of the cases of myocarditis. It occurs with flu-like symptoms for 2-10 days. And after a couple of weeks, heart complications may appear in the form of fever, chronic fatigue and chest pain.
• ECHO viruses
- another group of microorganisms that cause intestinal infections. They may appear as a skin rash and most often affect children. The most common complication of echoviruses is myocarditis.
• Parvovirus B19
- an infection that causes anemia and, as a complication, heart damage. According to statistics, 2-15% of children and 85% of older people have encountered parvovirus. But in people with a healthy body, the infection is often asymptomatic and may go unnoticed altogether.
• Rubella
- a viral infection, especially dangerous for pregnant women if they do not have developed immunity to it. When the rubella virus enters the heart tissue, myocarditis develops.
Any foci of chronic inflammation of a bacterial nature can become a source of infection that is dangerous to the heart. For example, there are known cases of the development of endocarditis due to bacteria living in the mouth and throat of a person. Through damage to the oral mucosa, they enter the bloodstream and thus penetrate the tissues of the heart. Streptococci are especially dangerous in this regard.
Bacteria that attack heart tissue:
•
Streptococcus pneumonia
;
• Staphylococcus aureus
- causes infective endocarditis in almost 100% of cases;
• Enterococcus
;
• Escherichia coli
and etc.
It should be added that damage to heart tissue is not always caused directly by microorganisms. For example, in a study of pneumococcal heart infections in streptococcal pneumonia, it turned out that the bacteria produce the toxin pneumolysin. The microorganisms themselves do not need to enter the heart - myocardial cells die under the influence of pneumolysin.
Fungi are another group of microorganisms that can affect the heart.
. Most often, fungal infections of cardiac tissue develop during long-term antibacterial treatment, for example, after surgery or with prolonged use of venous catheters.
Risk factors for heart infections
Most often, infectious heart lesions develop in people who have a predisposition to their occurrence.
The development of the disease is determined by the presence of such aggravating factors
:
• Congenital or acquired heart defects.
• The presence of reduced immunity due to severe stress, HIV/AIDS, congenital pathologies.
• Cardiac surgery performed (heart valve replacement).
• Carrying out dental procedures.
• Frequent sore throats.
• Use of injecting drugs.
Clinical manifestations of infectious lesions of the heart
Clinical manifestations of endocarditis
The phenomena of endocarditis occur, as a rule, 2-3 weeks after an infectious disease. Most often, with endocarditis, the body temperature rises sharply to high numbers (38-40°C), chills occur, but in some cases the temperature can even be reduced (below 36°C). More specific symptoms of endocarditis include:
• Muscle pain, joint pain, weight loss, weakness, headache.
• Change in skin color – it becomes jaundiced.
• Peculiar hemorrhages occur on the skin and conjunctiva of the lower eyelid.
• Purple-purple spots up to 5 mm in diameter may appear on the palms, feet and torso.
• Small bumps of dense consistency appear on the palmar surfaces of the fingers and soles.
• Heart pain and dry cough may occur.
Clinical manifestations of myocarditis
Infectious damage to the myocardium makes itself felt 1-2 weeks after the first symptoms of any previous infection. The first and most characteristic signs of myocarditis:
• Increased heart rate over 90 beats/minute.
• Chest pain.
• Feeling of interruptions in heart function.
• Shortness of breath.
• High temperature (38-39ᴼС).
If a complication such as heart failure occurs, the described symptoms may be accompanied by swelling in the lower extremities. In a chronic course, symptoms may appear and disappear after a while, after which they recur again.
Clinical manifestations of pericarditis
It should be mentioned that pericarditis has two main forms: dry and exudative. Depending on the form of pericarditis, the symptoms will differ.
With dry pericarditis there are three leading symptoms:
• Severe chest pain, localized in the center, becomes more intense when sneezing, coughing, swallowing and even breathing. The pain is not relieved by the use of nitroglycerin, but is slightly reduced by the use of analgesics (nimesulide, analgin, ibuprofen), as well as by bending the torso forward.
• Pericardial friction noise, reminiscent of crunching snow.
• Changes in the electrocardiogram that can only be detected in a hospital or when visiting an ambulance.
With exudative pericarditis, the symptoms are different:
• Increased heart rate occurs (rate over 90 beats/minute).
• Body temperature rises to 37.5-38ᴼC.
• Severe shortness of breath appears.
• There is a desire to press the body to the knees, as this position alleviates the condition.
• Swelling may occur in the legs and fluid may accumulate in the abdominal cavity.
• Blood pressure decreases below 120/80 mmHg.
If you identify the described symptoms or a group of symptoms, you must seek qualified medical help as soon as possible and report your symptoms to a general practitioner or cardiologist in order to avoid complications that are life-threatening. Further diagnostic tactics and treatment are prescribed only by a doctor!
Prevention of infectious heart diseases:
The main goal of prevention is to prevent infection from entering the heart tissue.
To do this, you need to: • If you catch a dangerous infection, consult a doctor in a timely manner, without allowing the disease to develop complications.
• Control the microflora of your body - where possible.
Any foci of chronic infection are risk factors for heart damage. For example, brushing and flossing regularly reduces the chance of oral infection spreading.
Lead a healthy lifestyle.
Not all people who contract an infection are susceptible to infectious heart disease. The healthier a person leads a lifestyle, the better protected he is from the spread of infection throughout the body.
Smoking, weak immunity, alcoholism, and drug addiction reduce protection.
Patients with heart pathologies are at increased risk. If we are talking about a bacterial infection, you should strictly follow the course of antibiotics prescribed by your doctor. Stopping taking medications earlier than prescribed or taking them in smaller doses increases the risk of the emergence of bacteria resistant to these medications, progression of the disease and, as a result, the development of heart complications.
Monitor a patient who has had an infectious disease for some time.
Damages to the cardiovascular system can go undetected for a long time if the body as a whole has enough strength to compensate for damage to the tissues of the heart and blood vessels.
If the doctor believes that medications should be taken to support the functioning of the heart for some time after recovery, these prescriptions must be strictly followed.
Cardiologist, medical therapist, candidate of medical sciences Gilmanshina Diana Ralifovna