Carotid arteries
Diseases of the carotid arteries occur when developing atherosclerotic plaques partially or completely block their lumen. The carotid arteries are paired vessels that supply blood to the head and brain.
The carotid arteries are paired vessels that are located in the neck and provide blood flow to the brain.
Narrowing of the lumen of the carotid arteries due to the formation and growth of atherosclerotic plaques reduces the volume of blood flowing to the brain and increases the risk of stroke.
Symptoms
Since atherosclerotic lesions of the carotid arteries develop slowly and are often asymptomatic, the first clinical manifestations of this disease may be a stroke (acute cerebrovascular accident - stroke) or transient ischemic attack (TIA), sometimes called a microstroke.
Treatment of atherosclerotic lesions of the carotid arteries usually includes a set of measures, such as lifestyle changes, drug therapy and, in some cases, surgical treatment (open surgery or stenting).
In the early stages, atherosclerotic lesions of the carotid arteries are usually asymptomatic. You and your doctor may not be aware that you have a narrowing of the carotid artery until an acute disruption of cerebral blood supply develops as the first and very serious manifestation of the disease.
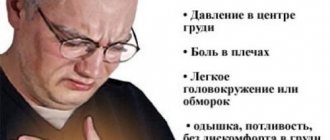
Clinical manifestations of stroke or transient ischemic attack may include:
- a sudden feeling of numbness or weakness in the face or limbs, usually on one side.
- Impaired speech or understanding
- sudden loss of vision in one or both eyes
- dizziness or loss of balance
- sudden, causeless severe headache
If you have risk factors for developing atherosclerotic lesions of the carotid arteries, you should consult your doctor. Your doctor may order an examination to determine the condition of these vessels. Even if you do not have clinical manifestations of the disease, your doctor may recommend a number of measures aimed at reducing the severity of risk factors and reducing the likelihood of developing a stroke.
Seek immediate medical attention when you experience symptoms of a transient ischemic attack or stroke.
Even if the duration of symptoms is short, usually less than an hour, but possibly longer, tell your doctor right away. The appearance of these symptoms indicates that you have suffered a transient ischemic attack - a short-term decrease in blood flow to the brain. The presence of transient ischemic attacks is the most important sign that you are at high risk of developing a stroke if preventive measures are not taken in time. A timely visit to the doctor increases your chances that atherosclerotic lesions of the carotid arteries will be identified and eliminated before an acute cerebrovascular accident develops.
A transient ischemic attack may also indicate a decrease in blood flow through other blood vessels in the brain. To clarify the diagnosis, your attending physician will prescribe the necessary examination.
Make sure your family and close friends are aware of the clinical manifestations of a stroke and that it is important to act quickly if they occur.
About symptoms that may indicate a tumor on the carotid artery - angiosurgeon of the Scientific Research Center
The earlier a disease is detected, the greater the chance of curing it. This applies to all diseases, but especially to cancer. In addition to fairly common types of cancer (breast cancer, cervical cancer, stomach cancer, and so on), there are also more rare and poorly understood tumors. One of them is carotid paraganglioma, which is also called carotid body tumor, or carotid chemodectoma. This is a tumor that forms inside the neck, at the site of the bifurcation of the human carotid arteries.
Targeted drugs have not been developed for these tumors, they respond poorly to radiation and chemotherapy, and the main treatment method is surgery. The editors of zakon.kz decided to find out what type of neoplasm this is and how it can be avoided.
Despite the fact that it becomes malignant in rare cases (5-20%), this type of neoplasm can grow rapidly, reaching large sizes, and cause a number of severe complications: from cerebrovascular insufficiency to compression of the upper respiratory tract. For this reason, the best treatment is often surgery to completely remove the tumor.
At the initial stage, the patient cannot detect the tumor due to its small size. However, he begins to notice it at a stage and size where it is easy to remove. However, at this stage, patients, as a rule, do not come to us, ignoring the problem and thinking that the seal will “resolve” on its own. Unfortunately, they come to specialists when the tumor begins to envelop the surrounding vessels and grow into the walls of the carotid artery. At this stage, various serious symptoms may appear: the patient has difficulty breathing, fainting, and so on. That is, a person turns to doctors when the tumor begins to cause discomfort,” said angiosurgeon at the National Scientific Oncology Center Abay Tulemisov.
The tumor is located in the area where the carotid artery bifurcates, and it is technically difficult to operate. Such operations can be accompanied by large blood loss, there is a risk of damaging the nerves responsible for speech and swallowing function, there is a high risk of stroke, and artery plastic surgery is often required, the doctor added.
Unfortunately, at the moment, scientists have not yet been able to determine how this tumor develops and whether it is the result of hereditary mutations, so that a hereditary predisposition to it can be detected in time. Moreover, at present, there are no other effective treatments for carotid paraganglioma other than surgery.
Doctors point to the following symptoms that signal the development of a carotid body tumor.
First, the tumor begins to attract attention when it becomes possible to palpate it at the angle of the lower jaw, even independently. Sometimes such patients experience discomfort when swallowing or turning the head, pain when pressing on a tumor-like formation, pain radiating to the head, face and ear, headaches and dizziness resulting from a decrease in the lumen of the carotid artery. Intensive enlargement of carotid chemodectoma is accompanied by the development of progressive neurological disorders caused by compression of nearby nerves. Some patients experience episodes of decreased blood pressure and short-term fainting states when pressing on the tumor. Sometimes patients may experience hoarseness, sudden attacks of weakness, decreased heart rate, and unstable blood pressure. In rare cases, such patients may develop mental disorders of the oncophobia type (fear of cancer). Due to the close connection with the carotid artery, there may be a feeling that the tumor is pulsating, the doctor noted.
Approximately 5-20% of such tumors turn from potentially benign to malignant. In this case, the tumor grows faster and grows into neighboring vessels and nerves. From there, the disease quickly metastasizes to the lymph nodes, liver, and bones.
— What surgical treatment methods are available for tumors of the carotid artery?
In collaboration with x-ray endovascular surgeons, the National Cancer Research Center's vascular surgery team offers patients a multidisciplinary approach to the treatment of carotid artery tumors. As a rule, a team of doctors is able to perform procedures such as transcatheter embolization of vessels feeding a carotid chemodectoma and reconstruction of the carotid arteries, said Abay Tulemisov.
Most often, operations on blood vessels, including the carotid artery, are performed in our center. Why? Because our center employs doctors with extensive experience in performing operations on the arteries of the neck, in particular, my colleague performed about 500 such operations. And this is a good experience. Every year, the department performs about 120 operations on the carotid arteries, 5 of which are for carotid chemodectoma, so our doctors successfully remove such a tumor,” the doctor added.
The technology of surgical intervention and anesthesia for lesions of the carotid arteries was introduced in the clinic in 2010, when the doctors of the department received the appropriate qualifications and specialization in foreign clinics: Assuta Medical Center (Tel Aviv, Israel), Russian Scientific Center of Surgery named after. Petrovsky (Moscow, Russia), National Medical Research Center named after. Meshalkin (Novosibirsk, Russia), after which master classes were held within the walls of the National Scientific Oncology Center with the participation of specialists from the above clinics.
Tumors of the carotid body are extremely rare. According to statistics, this is 5-6 cases per year. It is difficult to perform such an operation in regional clinics. Therefore, it is important to contact specialized centers, where such operations are carried out.
— What is transcatheter embolization of carotid chemodectoma?
With the development of interventional technologies at the present stage, this procedure is widely introduced into the practice of vascular surgery. The purpose of the technique is to reduce the blood supply to the tumor. It is performed in advance of open surgery. During the procedure, a very thin tube called a catheter is inserted through the femoral artery to reach the blood vessels feeding the tumor. Then, using various special means, the nutrition of the tumor is blocked. Thus, during the upcoming operation, the risk of massive blood loss is reduced. This significantly reduces the level of complications during surgery and in the postoperative period,” the doctor answered.
— How is surgical removal of a tumor performed?
— Surgical removal of carotid chemodectoma is a radical treatment method. The operation is difficult due to the tight connection of the tumor with the branches of the carotid artery and the close location, and sometimes involvement, of the vagus and hypoglossal nerves. Therefore, during the diagnostic stage, it is very important to determine the exact topographic anatomy of the tumor using CTA data. In most cases (60–70%) the tumor can be removed without the need to remove part of the carotid artery. If the artery wall still needs reconstruction, this can be done by applying a vascular suture, the doctor noted.
- Sometimes more complex repairs are required, such as patching the hole made when the tumor was removed, or completely replacing a section of the artery with a bypass graft (using another blood vessel to create a new path for blood flow). Removal of the tumor may be accompanied by the removal of part of the carotid artery with its replacement with the great saphenous vein or a synthetic prosthesis, added Abay Tulemisov.
The team of vascular surgeons at the National Cancer Research Center has extensive clinical and practical experience in working with the carotid arteries and their tumors, and takes special precautions to reduce the risk of complications. The clinic’s doctors will tell patients about all possible risks in each specific case.
In the scientific literature, doctors note the absence of relapses of the disease after surgery, with a follow-up period of up to 15 years. But for successful surgical treatment, in their opinion, “a high degree of clinical suspicion and early diagnosis” are important. The second important factor for successful treatment is that the operation must be performed by an experienced surgeon.
— How to prevent complications, where to go if a person suspects he has this disease at the initial stage? What examinations need to be completed?
- As soon as a person discovers a lump in his neck, this should alert him. In this case, he needs to go to the clinic at his place of residence and see a general practitioner. To establish a preliminary diagnosis, the doctor will prescribe the necessary instrumental studies, including ultrasound examination of the soft tissues of the neck and Doppler ultrasound of the great vessels. Next, the patient is sent for consultation to the appropriate specialists in order to decide on further treatment tactics, the doctor answered.
In general, problems with blood vessels in a person arise in connection with his lifestyle. The key to vascular health is a proper diet low in fat and salt, and maintaining physical activity. It has been proven that smoking significantly increases vascular damage, as it causes their persistent narrowing. This contributes to an increase in blood pressure in the vessels, which also leads to their damage.
Causes
Over time, the walls of the carotid arteries can become thickened, their lumen narrows due to the formation of atherosclerotic plaques, which leads to a decrease in the volume of blood flowing through them. Atherosclerotic plaques consist of accumulations of cholesterol, calcium, fibrous tissue elements and cell debris that penetrate the artery wall through microscopic damage to the inner lining and form an atherosclerotic plaque in the area of which a blood clot (thrombus) can form.
Normal, healthy carotid arteries, like other normal arteries, are soft and flexible and allow blood to flow freely. If you place your finger on either side of the Adam's apple, you can feel the pulsation of the carotid arteries. The carotid arteries provide oxygen and nutrients to the cortex and other vital structures of the brain.
Risk factors
Factors that affect arteries and increase the risk of damage, plaque formation, and disease include:
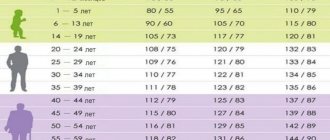
- High blood pressure.
High blood pressure is the most important factor in the development of atherosclerotic lesions of the carotid arteries. Exposing the artery wall to high pressure weakens it and makes it more susceptible to damage. - Smoking.
Nicotine irritates the inner lining of blood vessels, and also increases heart rate and increases blood pressure. - Age.
With age, the arterial wall loses elasticity and becomes more susceptible to damage. - Violation of the blood lipid ratio.
Elevated levels of low-density lipoprotein cholesterol ("bad cholesterol") and high levels of triglycerides contribute to the formation of atherosclerotic plaques. - Diabetes.
Diabetes not only affects the ability to control blood sugar levels, but also lipid metabolism, increasing the risk of hypertension and the development of atherosclerosis. - Obesity.
Excess body weight increases the risk of arterial hypertension, atherosclerosis and diabetes. - Heredity.
The presence of atherosclerosis or coronary heart disease in relatives significantly increases the risk of developing atherosclerotic lesions. - Sedentary lifestyle.
Lack of physical activity contributes to the development of hypertension, obesity and diabetes.
Often, the listed risk factors are present in combination, thereby increasing the degree of risk.
Complications
Atherosclerotic plaque
The most dangerous complication of atherosclerotic lesions of the carotid arteries is stroke. There are various mechanisms that increase the risk of stroke:
- Decreased blood flow.
The carotid arteries may become so narrowed by atherosclerotic lesions that they are unable to provide adequate blood supply to the brain. - Rupture of an atherosclerotic plaque.
Particles of atherosclerotic plaque can break off and travel with the bloodstream into smaller vessels of the brain, blocking the lumen of these arteries and blocking the blood supply to the area of the brain that is fed by this vessel. - Blood clot formation.
The surface of some atherosclerotic plaques may rupture to form an uneven, ulcerated surface. When this happens, the body's response is to attract platelets to the site of the break and form a blood clot (thrombus). Large blood clots can partially or completely block the lumen of an artery, thereby impeding blood flow and causing a stroke.
The consequences of a stroke can be the formation of a focus of brain damage and dysfunction of organs, in particular paralysis of the limbs. In severe cases, a stroke can be fatal.
Stroke or transient ischemic attack are often the first manifestations of atherosclerotic lesions of the carotid arteries and are considered medical emergencies. If you or your loved ones have symptoms of impaired blood supply to the brain, you should urgently seek medical help. Do not try to get to the hospital on your own.
Signs of concern:
- sudden feeling of numbness or weakness in the face or limbs, usually on one side;
- impaired speech or understanding;
- sudden loss of vision in one or both eyes;
- dizziness or loss of balance;
- sudden causeless severe headache;
Diagnostics
Depending on the preliminary diagnosis, the specialist prescribes a proper diagnostic regimen.
The process of diagnosing pathologies takes place in several stages:
- Face-to-face consultation with a survey of the patient regarding current complaints, duration and severity of symptoms, the presence of direct provoking factors;
- Study of anamnesis (personal and family);
- Laboratory tests for the presence of atherosclerosis (lipid profile with calculation of the atherogenic coefficient, biochemical blood test, determination of proteins in blood serum, etc., at the discretion of the specialist);
- Magnetic resonance or classical angiography;
- Ultrasound Dopplerography (Doppler ultrasound).
The latest study is considered the most informative. It allows you to determine:
- The speed and intensity of blood flow in the vessels;
- Places that prevent the movement of arterial blood to the brain;
- The presence of atherosclerotic lesions;
- The presence of detachments, dilations, occlusions, stenosis of the vessel;
- The presence of blood clots and atherosclerotic plaques, their size and shape;
- Deformations of the vessel (tortuosity, loops, protrusions, bends);
- Dimensions of the lumen of the affected vessel;
- Condition of the vascular walls (elasticity, mobility, firmness);
- Modifications of the arterial wall.
When a pathology is detected, the specialist prescribes comprehensive treatment to the patient.
Diagnostic methods
After collecting anamnesis, identifying risk factors and characteristic symptoms, the doctor may conduct an additional examination, including:
- A physical examination,
during which the doctor, using a phonendoscope, can detect a noise above the carotid artery in the neck, which indicates a narrowing of the artery. The doctor may also conduct a neurological examination to assess your physical and mental status, such as strength in your limbs and ability to remember spoken language. - Ultrasonography.
The most common non-invasive research method to assess the condition of the carotid arteries is Doppler ultrasound. This is a variant of conventional ultrasound examination that evaluates blood flow speed, pressure and can detect narrowing of the lumen of the arteries due to changes in these indicators. - Computed angiography.
This procedure is performed using a contrast agent to highlight the arterial vessels. The drug is administered intravenously. When it reaches your carotid arteries, a series of X-ray images are taken of the neck and brain area in different views. - Magnetic resonance imaging.
Similar to CT scanning, this method can visualize brain tissue and detect early brain lesions or other pathology. - Angiography.
It is a more “sensitive” invasive research method. However, it is now used less and less due to the existing risk of stroke during the procedure. During the study, X-ray images of the arterial vessels supplying the brain are taken, with preliminary intra-arterial administration of a contrast agent.
Treatment methods
Treatment of arteritis in our department is carried out by experienced, highly qualified specialists in the field of phlebology, who use various therapeutic and surgical methods in their practice.
Drug treatment of arterial inflammation involves hormonal therapy using high doses of glucocorticosteroids. As a rule, such treatment continues for a long time, up to one year. If a patient is intolerant to glucocorticosteroids, he is given other drugs that are less effective.
Patients with temporal arteritis with the threat of vision loss are prescribed special treatment, including pulse therapy with prednisone, as well as the use of vasodilators and vasodilators.
Surgical treatment of arteritis is indicated for complicated development of the disease. An operation may be prescribed if the patient has blood clots or vascular aneurysms. Surgical intervention is also required for cancer that causes the development of arteritis.
Timely diagnosed arteritis allows doctors to carry out effective therapy and completely rid the patient of the disease. If the diagnosis was made at an advanced stage with complications, the prognosis may be less favorable.
Treatment
The goal of treatment of atherosclerotic lesions of the carotid arteries is to prevent the development of stroke. The choice of treatment method depends on the degree of narrowing of the artery lumen.
Slightly and moderately expressed narrowing.
In the presence of moderate narrowing of the carotid arteries, the following recommendations may be sufficient to prevent stroke:
- Lifestyle changes. Healthy lifestyle changes can help reduce damage to the carotid artery wall and slow the progression of atherosclerosis. Such changes include quitting smoking, losing weight, eating a healthy diet, reducing salt intake and regular exercise.
- Treatment of concomitant chronic diseases. At the same time, it is necessary to treat such concomitant diseases as arterial hypertension, obesity and diabetes mellitus.
- Prescribing medications. Your doctor may prescribe you to take aspirin or other antiplatelet medications daily to reduce the risk of blood clots. Therapy aimed at correcting blood pressure (ACE inhibitors, beta blockers) and correcting the lipid profile – taking statins – may also be recommended.