Gangrene is one of the most severe surgical pathologies. This is tissue necrosis, which is impossible not to notice: the fact is that most often the skin in the affected area changes its color to dark gray or black. In the absence of timely treatment, gangrene can cause disability and even death for the patient.
The most common type of this pathology is gangrene of the leg: a finger or the entire foot of the lower limb. Most often, this is a complication of diabetic foot – one of the consequences of diabetes mellitus (the so-called “Sugar gangrene”). However, in some cases, tissue necrosis can occur on the torso or in the face, and also spread to some internal organs - for example, a fragment of the intestine, appendix, etc.
For dry gangrene
the boundary between dead black skin and living skin of normal color is clearly defined (line of demarcation). Dry gangrene is more favorable than wet gangrene. This is due to the fact that dead tissue is well separated from living tissue and practically no decay products enter the bloodstream, causing intoxication. Dry gangrene usually develops against the background of prolonged ischemia, when collateral small vessels have time to form, feeding damaged tissues, and as ischemia worsens, the body “manages” to limit the necrotic process.
Classification of diabetic foot forms
Diabetic foot syndrome is classified according to the severity of the disease. There are 6 stages, starting from zero (the foot is deformed, hyperkeratosis occurs, and calluses form) and ending with stage five (extensive spread of gangrene).
The traditional classification includes 3 forms of the disease.
1. The most common neuropathic form (about 70% of all cases). Diabetes mellitus primarily affects the nervous system of the legs, which significantly reduces the sensitivity of tissues to heat, pain, and touch. The skin becomes dry, hyperkeratosis occurs (the skin is excessively flaky), anhidrosis (sweating is impaired), and flat feet develop. The bones of the foot can become deformed (a common symptom is the formation of a Charcot joint) and become excessively fragile, which increases the risk of unexpected fractures.
2. The ischemic form accounts for up to 10% of cases. It is characterized by atherosclerotic disruption of the blood supply to the foot due to the destruction of large and small vessels under the influence of excess sugar and glucose. As a result, the leg swells noticeably, and the swelling practically does not subside. Walking causes discomfort or pain in the patient, he limps, gets tired quickly and is unable to walk long distances. Visually you can notice how the pigmentation of the skin changes.
3. Approximately 20% of cases of diabetic foot syndrome occur in the mixed form , which is also called neuroischemic. This is the most complex disease, since the symptoms and signs of previous forms are clearly expressed.
Most often, individual forms (neuropathic or ischemic) are diagnosed in the early stages. Their occurrence depends on what problems the patient faces - whether he is worried about neuropathy or ischemia. Over time, the manifestations of the disease become more complex, and both forms flow into one another.
The most severe form is considered diabetic gangrene . In this case, the blood supply is disrupted over a large area of the leg - right up to the top of the lower leg. This provokes the development of an anaerobic infection, since the cells on the affected limb do not resist its penetration. This is the most advanced form of the disease, when only amputation can help. That is why treatment for diabetic foot symptoms should be started as early as possible.
Symptoms of gangrene
Typically, gangrene is preceded by prolonged pain in the distal (most distant) parts of the limb - fingers, heel. This is observed with gradual blockage of blood vessels, for example, with obliterating atherosclerosis. In acute arterial thrombosis, pain occurs suddenly, and if left untreated, gangrene begins to form within a few hours (days).
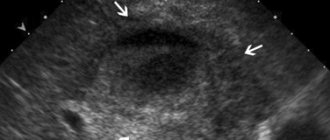
Gangrene begins with the appearance of a bluish spot on the skin of the toes or heel, which gradually increases in size, turns from bluish to dark, then turns black. If gangrene is dry , then it manifests itself as a black area of skin (or a finger, sometimes part of the foot with fingers) with a clear demarcation from intact tissue. The patient's general condition usually does not suffer, the temperature and health are normal. The severity of the pain syndrome varies. Wet gangrene manifests itself as blackening of the skin of a finger or several fingers and part of the foot without demarcation, i.e. next to the black areas of the skin there are purple-bluish ones, higher up there is redness and swelling. There is no clear boundary between areas of different colors. The general condition can be severe (not always), body temperature usually rises. Wet gangrene tends to spread to the upper parts of the limb.
What is diabetic foot?
Medical practice shows that many people with symptoms of diabetes ignore the problem of metabolic disorders in the body and seek treatment from a doctor only when serious complications occur. Only in 50% of cases are requests recorded at an early stage.
A number of patients really pay attention and begin treatment for this disease when they begin to show signs and symptoms of developing diabetic foot syndrome:
- tissues become overgrown with ulcers;
- necrosis develops under the influence of infections;
- the skin on the sole is cracking;
- in some vessels, blood flow is disrupted or stops altogether;
- the limb itself loses its functions.
A person cannot step on his foot due to pain, and then completely loses the ability to move independently. The tissues of the foot gradually die - this includes nerves, joints, bones and blood vessels. The patient inevitably becomes disabled.
Meanwhile, the symptoms of diabetic foot are a severe and advanced stage of diabetes mellitus (in 90% we are talking about type II diabetes), which requires immediate and qualified treatment. Ulcers will not “heal” on their own, and a gradual decrease in physical activity will lead to a worsening of the disease. Most often, signs and symptoms appear 10-15 years after the first manifestations of diabetes. However, in most cases this concerns patients who do not pay due attention to diabetic treatment and prevention.
Of course, not all patients with diabetes develop diabetic foot syndrome. However, about half of them are at risk, and statistics show that this complication occurs in 10% of diabetics.
Treatment of gangrene
The main treatment method is amputation. Those tissues that are dead cannot be brought back to life, so they must be removed. The question is usually about the level of amputation. The approach here is ambiguous. It would seem that if one finger is affected by gangrene, why not limit it to amputation? But if all the arteries of the leg, the popliteal artery, are affected, then after amputation of the finger the wound will not heal, the sutures will “fall apart”, the necrotic process will progress further, which will require a higher amputation already at the level of the foot. Then the wound does not heal again - amputation at the level of the lower leg, then at the level of the thigh, where the wound almost always heals, because In the thigh, blood circulation is usually good, which is associated with the flow of blood from the deep femoral artery and from the internal iliac artery. Each operation is stressful for the body and increases the danger to life. Therefore, amputation must be done once and at a level that ensures good wound healing.
“Minor” amputations (fingers, part of the foot) can be limited to diabetic gangrene, because general blood circulation in the limb is usually preserved (if diabetes is not combined with atherosclerosis of the arteries). With obliterating atherosclerosis, amputations usually have to be done “high”, at the level of the hip. In some cases, it is possible to perform reconstructive surgery on blood vessels (bypass surgery, stenting) - then blood circulation in the limb improves, which makes “low” (at the level of a finger, foot) amputation possible.
Patients also receive therapy aimed at improving microcirculation in the limb (angioprotectors, antiplatelet agents), antibacterial therapy, and pain relief.
Causes
Often, diabetic foot syndrome is a consequence of diabetes mellitus, which is accompanied by atherosclerosis, coronary heart disease, arterial hypertension, smoking, and alcohol abuse.
However, a diabetic leg ulcer can also be caused by a seemingly harmless cause. People suffering from diabetes may not pay attention to calluses, corns, cracked heels, or ingrown toenails that appear due to tight shoes. Meanwhile, these small injuries provoke the disease.
Diabetes mellitus negatively affects the functioning of the entire body, but the lower extremities suffer the most (especially since they bear a serious daily load). Saturation of the blood with excess sugar and glucose destroys blood vessels - large and small (a distinction is made between macro- and microangiopathy in diabetes), bones and muscles. Due to anatomical features, blood circulates in the legs of any person worse than in other parts of the body, so it is the feet that are the first to suffer from total circulatory problems in diabetes.
Lesions of the lower extremities in patients with diabetes mellitus
About the article
31698
0
Regular issues of "RMZh" No. 13 dated June 15, 2006 p. 972
Category: General articles
Authors: Volkova A.K. , Komelyagina E.Yu. , Antsiferov M.B.
For quotation:
Volkova A.K., Komelyagina E.Yu., Antsiferov M.B. Lesions of the lower extremities in patients with diabetes mellitus. RMJ. 2006;13:972.
Diabetes mellitus (DM) is one of the most common chronic diseases and is a non-infectious epidemic. Currently, about 200 million people in the world suffer from diabetes, while the number of patients increases annually by 5–7% and doubles every 15 years. According to WHO experts, their number will reach 325 million people by 2025, and 410 million people will have impaired glucose tolerance (IGT). DM is characterized by early disability and high mortality of patients due to the development of late vascular complications. This circumstance places diabetes among a number of socially significant diseases.
Lesions of the lower extremities in patients with diabetes are one of the main causes of disability, since the risk of non-traumatic amputations of the lower extremities in a patient with diabetes is 22 times higher compared to the same probability in the absence of diabetes [1]. The above fact was one of the main reasons why the St. Vincent Declaration (1989) proclaimed a 50% reduction in the number of high amputations among patients with diabetes mellitus in the world by 2000 [2]. Lesions of the lower extremities in patients with diabetes include: diabetic neuropathy (DN), lesions of the main bloodstream of the lower extremities (macroangiopathy), diabetic foot syndrome (DFS). Diabetic neuropathy Diabetic neuropathy is the presence of symptoms and/or objective signs of neuronal dysfunction in a patient with diabetes, subject to the exclusion of other causes [3]. The prevalence of the complication is quite high, depending on various examination methods, varying between 30–50% [4]. And if we add patients with subclinical forms to the number of patients with obvious clinical signs of diabetic neuropathy, then the incidence of neuropathy can reach 90% [5]. There are different classifications of diabetic polyneuropathy, one of which is given below. Classification of diabetic polyneuropathy [6]: • Hyperglycemic neuropathy • Generalized neuropathies: – sensorimotor – acute pain – autonomic – acute motor • Focal and multifocal neuropathies • Hypoglycemic neuropathy. In terms of damage to the lower extremities, sensorimotor neuropathy is most often encountered in clinical practice, which will be discussed below. Chronic hyperglycemia plays a key role in the pathogenesis of diabetic neuropathy [7]. Long-term elevated blood sugar levels lead to activation of the polyol pathway of glucose metabolism, causes oxidative stress, reduces the formation of nitric oxide, reduces blood flow in the nerve fiber, and disrupts the formation of growth factors. All of the above mechanisms cause the death of a nerve cell and lead to a slowdown in the conduction of impulses along the nerve fiber. Clinical manifestations of DN significantly reduce the quality of life of patients and are the most important pathogenetic and prognostically significant risk factor for the development of a number of complications of diabetes mellitus, in particular, diabetic foot syndrome. The clinical symptoms of DN can be positive (productive) when the patient presents certain complaints, and negative when there are no active complaints, but there are already sensory disturbances. Basically, painful and painless variants of lesions are distinguished [8]. In the absence of active complaints from the patient, the diagnosis of neuropathy can be made only on the basis of the results of examination and diagnostic testing. Among the painful forms of neuropathies, acute and chronic are distinguished [9]. The duration of the acute painful form is 6 months. Stitching, shooting, aching pains appear in the feet and legs; feeling of burning, numbness, tightening of the feet. The intensity of the pain syndrome may increase in the evening and at night. Chronic neuropathy is characterized by the presence of pain symptoms for more than six months. The clinical picture of pain varies in intensity and frequency. Compensation for diabetes can lead to regression of subjective symptoms, while inadequate control of blood glucose levels, on the contrary, worsens sensitivity and increases the feeling of numbness, burning, tingling, and paresthesia. Table 1 shows the main clinical manifestations of neuropathy depending on the stage of development of the pathological process [10]. The diagnosis of DN is established on the basis of characteristic complaints, anamnesis (duration of symptoms, presence of concomitant pathology), and objective examination data. In clinical practice, with the help of special instruments, disorders of various types of sensitivity are determined. To assess the presence of changes in tactile sensitivity, a monofilament weighing 10 g (5.07 Semmens–Weinstein) is used, pain is a prick of the back surface of the thumb with a special needle with a blunt end, temperature is by determining the difference in the sensations of heat and cold with a “tip therm” instrument, vibration - using a tuning fork or biothesiometer. Achilles and knee reflexes are used to assess motor dysfunction. For the purpose of early detection and in-depth study of DN, electromyography is performed to determine the speed of impulse transmission along the nerve fiber. The most accurate diagnostic methods include nerve biopsy followed by morphological examination. For a differential diagnosis of disturbances in the main blood flow of the lower extremities, Doppler ultrasound (USDG) of the arteries of the legs and feet is performed. Treatment of diabetic polyneuropathy Treatment of DN is characterized by an integrated approach and largely depends on the stage of development of the pathological process. Table 2 shows the principles of management of patients with diabetes mellitus and the presence of diabetic polyneuropathy. As you can see, at the initial stage of treatment, achieving compensation for carbohydrate metabolism is a prerequisite. In addition, normalization of glycemia often leads to the elimination of neuropathic pain, while drug therapy against the background of decompensation of carbohydrate metabolism may be ineffective. The prescription of symptomatic therapy is aimed primarily at eliminating the symptoms of peripheral neuropathy (pain, cramps, burning, paresthesia). The following may be prescribed: • tricyclic antidepressants (imipramine, amitriptyline) • anticonvulsants (gabapentin, carbamazepine) • analgesics • local irritants Pathogenetic drugs include: • aldose reductase inhibitors • g-linolenic acid • inhibitors of advanced glycation end products of structural proteins • drugs a- lipoic acid • nerve growth factors • myoinositol Currently, of all the above methods of pathogenetic influence, based on a number of international placebo-controlled studies, a-lipoic acid preparations have proven their effectiveness. It should be noted that one of the main objectives of managing patients with diabetic peripheral neuropathy is to prevent the development of foot ulcers. In this aspect, the main role belongs to teaching patients the rules of foot care and the selection of orthopedic shoes. Diabetic angiopathy of the lower extremities Diabetic angiopathy of the lower extremities is understood as “the presence of clinical signs such as absence of pulse in the arteries of the feet, a history of intermittent claudication, the presence of rest pain and/or changes detected during non-invasive vascular examination, indicating circulatory disorders” [3] . Reduced blood flow is the leading factor that disrupts tissue repair processes and, in combination with infection, is the main factor in lower extremity amputations [11]. The development of diabetic macroangiopathy is promoted by: smoking, arterial hypertension, chronic hyperglycemia, hyperlipidemia, age, genetic predisposition, duration of diabetes [12]. Manifestations of macroangiopathy in diabetes mellitus include: mediacalcinosis (Mönckeberg sclerosis) and atherosclerosis. Mönckeberg's sclerosis is calcification of the tunica media of the arterial wall. As a rule, mediacalcinosis in isolated form is not a cause of limb ischemia, since it is not accompanied by a decrease in the lumen of the vessel. It is believed that Mönckeberg's sclerosis is associated with autonomic polyneuropathy [13]. The course of atherosclerosis in diabetes mellitus has some differences compared to atherosclerosis in its absence [14]. Morphologically, atherosclerotic vascular lesions are characterized by a circular arrangement of plaques, systemicity, a tendency to complicated lesions with caseous decay, the formation of aneurysms, and clinically - by lesions in younger patients, the same frequency of occurrence in men and women, more rapid progression, frequent damage to the popliteal and tibial arteries. Clinically, angiopathy of the lower extremities is manifested by pain in the lower legs when walking - “intermittent claudication syndrome”, coldness of the feet. On examination - weakening or absence of pulsation of the great vessels of the lower extremities; marbled skin coloring, alopecia in the lower legs, hypothermia of the feet. In advanced cases, critical limb ischemia develops. It is characterized by the presence of ischemic pain at rest for more than 2 weeks, and/or the presence of ulcers or gangrene in the area of the foot or toes with systolic pressure in the area of the tibial arteries. To identify a decrease in the main blood flow in the arteries of the lower extremities, palpation determination is performed as a screening pulsations in the arteries of the feet. Weakening or absence of pulsation in at least one of them is an indication to refer the patient for a consultation with an angiosurgeon. The most common non-invasive method for studying the main course of the lower extremities is Doppler ultrasound (USDG) with calculation of the ankle-brachial index (ABI). ABI is the ratio of systolic blood pressure in the tibial arteries at the level of the middle third of the leg to systolic blood pressure in the brachial artery. Normally, the ABI is greater than 0.9 but less than 1.15. The degree of disturbance of the blood supply to the lower extremities is determined according to the Pokrovsky-Fontaine classification of chronic arterial insufficiency, based on the clinical manifestations of the pathology: I - functional: there are no clinical manifestations, intermittent claudication occurs during prolonged (more than 1 km) or fast walking. A decrease in ABI is detected when performing an ultrasound scan of the lower extremities. IIA – intermittent claudication when walking 500–200 m. IIB – intermittent claudication when walking less than 200 m. III – pain appears at rest. IV – presence of ulcerative-necrotic lesions of the lower extremities. However, it should be remembered that in patients with severe polyneuropathy, accompanied by decreased sensitivity, this classification does not always objectively reflect the severity of ischemia. The patient may not feel pain, which leads to underestimation of the severity of the condition. It is also necessary to know that the determination of ABI in the presence of mediacalcinosis is accompanied by falsely high ABI values (>1.15). Advanced methods for diagnosing lesions of the main blood flow of the lower extremities include duplex scanning of the arteries. Angiography is considered the “gold standard” for studying the vascular bed. The indication for performing angiography or aorto-arteriography is the identification of stenosis or occlusion by ultrasound to determine the possibility of performing reconstructive surgery. To assess the severity of tissue ischemia, the method of determining transcutaneous oxygen tension in the lower extremities is becoming increasingly widespread. Through transcutaneous gas analysis, it is possible to measure local oxygenation (TspO2) of the skin and, thus, assess the prognosis of healing of the wound defect. The level of TcpO2 is considered a critical indicator. Comprehensive management of patients with diabetes mellitus with impaired main blood flow involves addressing the following issues [16]: 1) improving the main blood flow; 2) normalization of carbohydrate metabolism (HbA1c 3) correction of blood pressure (target parameters should be considered blood pressure 4) prescription of drugs that reduce the increased thrombogenic potential of the blood (taking acetylsalicylic acid in a dosage of 50–325 mg is mandatory); 5) correction of the blood lipid spectrum (total cholesterol 1.2 mmol/l, triglycerides 6) adherence to a dosed walking regimen; 7) quitting smoking. To resolve issues of improving the main blood flow, patients with diabetes mellitus must be managed together with an angiosurgeon. The most effective method is reconstructive surgical interventions on blood vessels: bypass surgery (aorto-femoral, femoral-popliteal, femoral-tibial), percutaneous transluminal balloon angioplasty (alone or in combination with the installation of an endovascular stent). To improve the rheological properties of blood, vasoactive drugs are prescribed. In addition to platelet disaggregants (acetylsalicylic acid), the use of which is currently considered mandatory in this category of patients, drugs with complex effects are prescribed (pentoxifylline 1200 mg per day). Recently, reports on the beneficial effect of Tanakan (EGb 761) at 120 mg/day have been published quite often. at least 3 months. The effectiveness and safety of Tanakan for obliterating atherosclerosis of the lower extremities has been proven in a number of international double-blind placebo-controlled studies, which recorded a significant increase in walking distance before the onset of pain [17–19]. The beneficial vasoactive effect of Tanakan was objectified using Doppler ultrasound of the lower extremities [20]. We must not forget that uncontrolled use of vasoactive drugs can lead to the progression of retinopathy (hemorrhage into the vitreous body and retina). Therefore, throughout the prescription of vasoactive drugs, dynamic observation by an ophthalmologist is necessary. It should be noted that due to the presence of hemorheological, metabolic, neuroprotective and antioxidant effects in Tanakan’s mechanism of action, the drug has a protective effect on the retina. The safety and effectiveness of Tanakan in the treatment of patients with diabetic retinopathy was also confirmed by both foreign and Russian specialists during experimental and clinical studies [21]. The absence of contraindications, drug-drug interactions and the favorable side effect profile of Tanakan identified in these studies allows us to recommend its wider use in elderly patients with diabetes mellitus when they have a combination of polyneuropathy, angiopathy and retinopathy. Diabetic foot Diabetic foot (diabetic foot syndrome - DFS) is an infection, ulcer and/or destruction of deep tissues associated with neurological disorders and/or a decrease in the main blood flow in the arteries of the lower extremities of varying severity [11]. Manifestations of DFS include “painless progressive destruction of one or more joints of the foot against the background of neuropathy - diabetic osteoarthropathy (Charcot foot) [22].” DBS is one of the leading disabling chronic complications of diabetes mellitus. From 40 to 60% (in some regions up to 90%) of all non-traumatic amputations are performed in patients with diabetes mellitus. In 85% of cases, all amputations associated with diabetes mellitus are preceded by infected foot ulcers, the prevalence of which is 4–10% among diabetic patients over 50 years of age. In most cases, amputations are performed due to a combination of deep tissue infection and ischemia: in 50-70% of cases, the cause of amputations is gangrene, in 20-50% - infection. It is necessary to distinguish between risk factors for diabetic foot syndrome and risk factors for amputation. As a rule, a peptic ulcer occurs as a result of a combined interaction of several risk factors. Risk factors for the development of diabetic foot syndrome, according to leading experts, can be presented as follows: peripheral neuropathy; peripheral vascular pathology; previous ulcers and/or amputations; foot deformities; poorly chosen shoes; injury; socio-economic factors; race [23,24]. Risk factors for amputation include: infected foot ulcers; infected foot ulcers in combination with ischemia. Currently, there is no single classification that takes into account all the features of the etiopathogenesis of diabetic foot syndrome. The following classifications have been proposed, taking into account various factors in the formation of this complication, such as: 1) the form of the lesion. Depending on the predominance of peripheral neuropathy or macroangiopathy, the following are distinguished: – neuropathic, – ischemic (in isolated form it is extremely rare), – neuro-ischemic forms of diabetic foot syndrome [11]. 2) depth of spread of the ulcer (Wagner classification) [25]. Depending on the depth of the lesion, the ulcerative defect is assigned a grade from 0 to V: Art. 0 – intact undamaged skin st. I – superficial ulcer (the process involves the epidermis, dermis) st. II – the process involves the skin, subcutaneous tissue, soft tissues. III – deep ulcer, abscess, osteomyelitis, septic arthritis Art. IV – dry/wet gangrene: necrosis of all layers of skin in individual areas of the foot, Art. V - dry/wet gangrene of part of the foot/all foot 3) the severity of the infectious process: • the infection that does not threaten limbs, characterized by the presence of signs of inflammation. Soft tissue edema, hyperemia and hyperthermia spread to less than 2 cm. As a rule, it is superficially located ulcerative defects that do not require hospitalization. • The infection threatening limbs. Soft tissue edema, hyperemia, hyperthermia spread by more than 2 cm, capturing deeply lying structures (subcutaneously fatty fiber, fascia, joints, bones) with the presence of necrotic and purulent discharge (plantar abscess, septic arthritis, feet of the foot, osteomyelitis). In this case, hospitalization is required for the relevant therapeutic measures. The main manifestation of the SDS is trophic ulcers or other purulent -destructive lesions of the foot. It should be noted that the ulcer of the lower leg, developing against the background of chronic venous failure, do not belong to the definition of SDS. Table 3 shows differential diagnosis of neuropathic and neuroichemic ulcers for SDS. The basic principles for the treatment of ulcerative defects in patients with diabetes in patients with diabetes strategy of comprehensive treatment of neuropathic infected ulcers consists of the following basic provisions: 1) surgical treatment of the purulent focus (the volume of intervention is determined by the severity of the existing infectious process); 2) the appointment of systemic rational antibacterial therapy; 3) local treatment of wounds using multicomponent ointments on a hyperosmolar basis, antiseptics and dressings that contribute to the purification of the wound; 4) execution of the unloading mode (fasting heel, use when walking crutches/ seats - strollers, etc.); 5) plastic and reconstructive organ -preserving operations. With the neuroichemic version of the lesion, the principles of therapeutic measures are as follows: 1) correction of arterial blood flow in the lower extremities (surgical and conservative); 2) surgical treatment of a purulent -non -chorotic focus (the volume of intervention is determined by the severity of the existing infectious process and compensation for arterial blood flow); 3) the appointment of systemic rational antibacterial therapy; 4) local treatment of wounds using solutions of iodophores, antiseptics and dressings that contribute to the purification of the wound; 5) if necessary, performing the unloading mode (unloading heel, use of crutches/seats - inks when walking, etc.); 6) plastic and reconstructive organ -preserving operations. Due to the fact that with diabetes, the risk of gangrene of the foot and, as a result, amputation of the limb, each patient should be familiar with the complex of preventive measures that allow us to sufficiently reduce this risk. Patients cannot be: trim the nails on their feet with scissors or use nippers; use corn -layers; walk barefoot; wear high -heeled shoes and a narrow nose; wear "slaps"; Heat your legs next to the heat source (next to the fireplace or on the battery). At the same time, patients need to: regularly file nails with a file; every day wash your legs in warm water, thoroughly wiping interdigital spaces after washing; Buy new shoes in the afternoon, when the legs were already slightly swollen; wear only cotton socks (warm your legs in socks from wool); wear only comfortable low -heeled shoes; With any wound on the legs, immediately contact the office of a diabetic foot. Compliance with these simple rules will significantly reduce the likelihood of amputation of the limb. Literature 1. Trautner C., Haastert B., et al. Amputations and diabetes: a case - comol Study // Diabet Med. - 2002. - Vol. 19. - P. 35–40. 2. Diabetes Care and Research in Europe: The St.vinsent Declaration. Geneva: World Health Organization. ICP/CLR 034 // - 1989. 3. International agreement on the diabetic foot, 2000. 4. Kempler P. Neuropathies - Springer - Budapest - 2002; Dyck Pj, Litchy Wj The Rochester Diabetic Neuropathy Study of Health Subjects. // Neurology, 1995, 45: 1115–1121. 5. Vinik AI, Liuzze Fi, ETS. Diabetes Neuropathy. Diabetes Care, 1992, 15: 1926–1975. 6. Thomas PK “Nextbook of Diabetic Neuropathy”, 2002. 7. The Diabetes Control and Complications Trial Research Group. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long - Term Complication in -Depness Diabetes Mellitus n.engl. J.Med. 1993; 70: 1009–1018. 8. International guidelines on the out -Patient Management of Diabetic Peripheral Neuropathy. Abingdon: The Medicine Group (Education) Ltd., 1998. 9. Kempler P. Neuropathies. Springer. Budapest. 2002. BULTON AJM “Nextbook of Diabetic Neuropathy”, 2002. 11. International agreement on diabetichek stop. - M., 1999. 12. Grandfather I.I., Antsiferov M.B. and co -authors. Diabetic foot syndrome. - M., 1998. 13. Young M. et al., Medial Arterial Calcification in the Feet of Diabetic Patients and Matched Non -Diabetic Control Subjects // Diabetologia. - 1993. –VOL.36. - P. 615–621. 14. Jude E., et al., Peripheral Arterial Disease in Diabetic and Nondiabetic Patients // Diabetes Care. - 2001. - Vol. 24. - P. 1433–1437. 15. Luther M. Critical Limb Ischemia in Diabetes // VASA. - 2001. - SUPPL. 58. - P. 21–27. 16. ADA: Clinical Practice Recommentations 2004 // Diabetes Care 2004; 27: S19 - S75. 17. Bauer U. etude clinicue d i/ egb 761 dans 1'artertedes Mambers inferieurs. Essai a duble Insu Face au Placebosur 6 Mois. // Arzneim Forsh Drug Res. –1984. –V.34. –N.6. –P.716–720. 18. Koshkin V.M. Conservative therapy of chronic obliterating diseases of the arteries of the limbs. // Russian Medzinsky Journal. –1997. –T.6. - No. 13. —s.820. 19. Pokrovsky A.V., Chupin A.V., Gryaznov O.G. The clinical test of the drug Tanakan in patents with atherosclerotic damage to the arteries of the lower extremities. // International Symposium “Consecious therapy in angology. Experience in the use of Tanakan and Gingko Fort preparations. ” - M. –1997. - Abstracts. - S.37. 20. Aliyev M.A., Dzhakupov V.A., Sekerbaev O.A. Conservative treatment of diabetic angiopathies. // in Sat: Surgical treatment of diabetic angiopathies. - Almaty. –1998. —P.29–32. 21. Moshetova L.K., Arzhimatova G.Sh., Strokov I.A., Yarovaya G.A. "Modern antioxidant therapy of diabetic retinopathy." Russian medical journal, 2006, v. 7, No. 1, 26–38. 22. Frykberg RG “Charcot Foot: An Update on Pathogenesis and Management” in the Foot in Diabetes, 2000, P.236. 23. Peter - Riesch b et al.: Pivotal Events: A Neglected Field of Factors Leading to Major Diabetic Foot Complications. // Diabetologia. 1996; 39, SUPPL. 1, A.265. 24. Veves A., et all: Comparison of Risk Factors for Foot Problems in Diabetic Ptions Attending Teaching Hospital Outpatient Clinics in Four Different European States. // Diabetic medicine. 1994; 11: 709–711. 25. Wagner FM a classification and Treatment Program for Diabetic, Neuropatic and Dysvascular Foot Problems. In the American Acaemy of Ortopaedic Surgeons Instructions Lectures. - St. Louis: Mosby, 1979. - P. 143–165.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Signs of diabetic foot
- An ingrown toenail occurs if the corners are not trimmed correctly. They can grow into tissues, and in these places inflammation occurs and pus forms, which is fraught with more serious consequences.
- A darkened nail indicates hemorrhage underneath it. Most often the reason is uncomfortable shoes. The consequences are the same - inflammation, pus, ulcer.
- A thickened nail can be the result of a fungal infection. Due to the irregular shape of the nail, the tissue under it is injured, and it can put pressure on neighboring fingers. In general, diabetics need to be careful about preventing fungal diseases.
- Calluses and corns are a common sign of the onset of diabetic foot. It is in them that invisible hemorrhages occur and pus is formed. Most patients “treat” these formations with patches and ointments, only worsening the problem.
- Cuts occur due to various factors, but in any case they should be carefully treated, since the wounds can be attacked by infection.
- Cracked heels are directly related to dry skin in neuropathic diabetic foot. Cracking leads to the formation of ulcers and bleeding.
- Deformation of the joints and bones of the foot provokes the formation of calluses and wounds on the skin.
How to treat diabetic foot?
- If the patient’s condition does not require hospitalization and the disease is not advanced, the doctor makes nutritional adjustments in order to achieve the correct balance of carbohydrates and the release of the required amount of hormones in the body.
- If diagnostics reveals problems with blood pressure, systemic drug therapy with beta blockers, inhibitors, diuretics, etc. is prescribed.
- Treatment of diabetic foot is inextricably linked with therapy for diabetes mellitus. Therefore, the patient takes insulin and medications in strictly adjusted doses to stabilize blood sugar and glucose levels.
- To combat the expansion of ulcers due to the proliferation of microbes, antibiotic therapy is carried out. The patient takes antispasmodics, Actovegin, and a-lipoic acid preparations.
- If there are suppurations or ulcers on the foot, treatment by an orthopedist is necessary. Special orthopedic devices, bandages, insoles, motion restraints, etc. are used.
- Wounds and ulcers are treated with antiseptics and antibacterial agents. If necessary, the surgeon excises necrotic tissue and removes potentially dangerous calluses and corns.
- Severe vascular lesions are treated by a vascular surgeon. Modern medicine offers a wide range of low-traumatic methods: stenting, bypass surgery, angioplasty, thromboembolectomy, etc.
- If the foot is gangrene and cannot be treated, amputation is performed.
Preventing diabetic foot symptoms
- Particular attention to prevention should be paid to people with extensive diabetic experience. In addition to preventive measures for diabetes (monitoring nutrition, blood glucose levels, etc.), there are specific recommendations:
- wearing special shoes without seams, with orthopedic insoles;
- performing foot exercises and self-massage;
- careful foot hygiene, careful pedicure;
- treating the skin with creams recommended by a doctor.
Diagnosis of diabetic foot syndrome
When heading to the diabetic foot office of an endocrinologist-diabetologist, be prepared for the fact that it may be necessary to visit an orthopedist, vascular surgeon, etc. Accordingly, the range of diagnostic procedures in each individual case may vary.
An important role in diagnosis and identifying signs of the disease is given to... the patient himself. If you are at risk, periodically conduct a self-examination of your feet for the signs of the disease described above. If you have the slightest suspicion, visit a diabetic foot clinic.
- The doctor determines the degree of sensitivity of the foot tissues, reflexes and other indicators.
- Laboratory tests that demonstrate characteristic changes in the composition of the blood are extremely important.
- Most often, the presence of ulcers requires bacterial culture of their contents for microflora.
- In the ischemic form, ultrasound examinations of blood vessels are prescribed. The method of duplex scanning of the veins of the lower extremities is extremely informative.
- Depending on the specific case, angiography and CT arteriography may be used.
- To diagnose changes in bones and joints, radiography is performed.
At the CBCP Clinic, we offer the latest methods for studying vascular dysfunction in diabetic feet. Ultrasound of the vessels of the lower extremities, performed on modern expert-class equipment, allows the doctor to obtain maximum information about the pathology.