Experts agree that isolating cyanosis into separate disorders is incorrect. Rather, it is a group of signs, visually expressed, combined for diagnostic purposes into a single group. Cyanosis is manifested by skin coloration that is different from normal. This is due to an increase in the amount of reduced (reduced) hemoglobin, which has a darker color.
Depending on the affected area, this may be:
- diffuse (generalized, extensive) cyanosis, when color changes throughout the body;
- local (peripheral) cyanosis or acrocyanosis.
If we can talk about this kind of phenomenon, cyanosis has its advantages. Firstly, it often becomes the only signal for urgent treatment of a critical pathology. Secondly, despite the severity of its symptoms, it is not accompanied by acute discomfort.
SYMPTOMATICS OF CUTANEOUS PHENOMENON AND ITS PROVOCATORS
There can be many provocateurs of cyanosis, but most often the color of the skin and membranes is observed with:
- diseases of the pulmonary-bronchial system (pleurisy, pneumothorax, pneumonia, asphyxia, emphysema, COPD, edema);
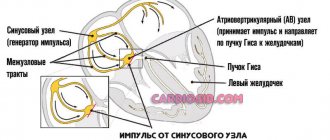
- critical pathologies of the heart and circulatory systems (embolism, myocarditis, endocarditis, tamponade).
By the way cyanosis spreads, one can judge its causative agent. Thus, gradual staining of the skin, starting from the membranes of the tongue, ears, face, indicates pathologies of the lungs or heart. Instantly developing cyanosis indicates toxic shock or anaphylaxis. With tamponade or thrombolism, cyanosis develops within 1-3 hours.
Color and distribution area
The color of the coat can indicate the need for urgent treatment.
- Red cyanosis is a sign of progressive diabetes. May indicate the need for treatment for polycythemia (a surplus of red blood cells) or cancer. Bright scarlet cyanosis of the face is a threat of developing oncology of the pituitary gland or adrenal glands.
- Dark purple color (ears, fingers, nose) is a sign of microthrombosis.
- Dark purple cyanosis accompanies pancreatitis.
- The orange color of the limbs (soles, palms) indicates cyanosis due to bleeding in the peritoneum.
The practice of treating diseases that are accompanied by cyanosis indicates that the proximity of the color to black-blue and violet more often indicates heart pathologies. The symptoms of the so-called blue disease – pulmonary artery stenosis – are separated into a separate block. There is also the concept of spotted cyanosis; it can signal vascular embolism, brain pathologies or hemorrhagic fever.
When blueness is concentrated in the extremities, the likelihood of treating thromboembolism increases. Or thrombosis of the main canals (with cyanosis with swelling of the limbs).
What is the cause of cyanosis
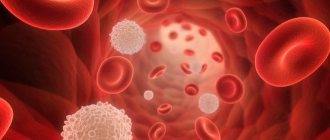
The term comes from the Greek word "kuaneos", meaning dark blue. That is, cyanosis is a change in the color of the nails, skin or mucous membranes of the mouth to a bluish tint due to an increased amount of reduced hemoglobin (Hb). For these symptoms to manifest, the content of reduced hemoglobin in capillary blood must be more than 5 g%. Reduced hemoglobin is the form of hemoglobin in red blood cells after oxygen is released in the tissues and the red blood cells combine with carbon dioxide. It is also called deoxygenated hemoglobin. High levels of deoxygenated hemoglobin in the superficial vessels, skin capillaries and venous plexuses cause this bluish tint. The thickness of the dermis, skin pigmentation and the condition of the skin capillaries determine whether cyanosis will be visible or not. Therefore, cyanosis is best seen where the overlying layer of the epidermis is thin and there is an extensive network of blood vessels in this area. The lips, tip of the nose, cheeks, ears, and oral mucous membranes are the areas where cyanosis will be most noticeable.
METHODOLOGY FOR STUDYING PATHOLOGICAL SKIN COLORING
Recognition of cyanosis comes down to differential analysis and verification of the provocateur (the disease against which cyanosis occurred, requiring treatment). At the first level, cyanotic pigmentation is distinguished from related pathologies - methemoglobinemia and carboxyhemoglobinemia.
To do this, blood is taken (it may contain toxins that cause one of three pathologies). For verification and “targeted” treatment, the following can be carried out:
- capillaroscopy;
- UAC;
- spectrophotometry;
- study of blood gases (arterial);
- pulse oximetry;
- measurements of PaO2 and SaO2;
- refined assay for the identification of hemoglobin derivatives.
To exclude (confirm for the purpose of treatment) OD pathologies, X-rays, chest CT and spirometry are performed. To exclude (or clarify and begin treatment) heart disease, you need an ECG / EchoCG, sometimes an MRI or scintigraphy.
Types of cyanosis
Various causes of cyanosis provoke disruption of gas exchange in tissues. An adult contains on average 15 g% hemoglobin, 95% of which is saturated with oxygen. When the amount of reduced hemoglobin in the capillaries exceeds 5 g%, the blood appears dark, which gives the tissues a bluish tint. Experts highlight:
- central;
- peripheral;
- mixed;
- cyanosis due to abnormal pigment.
Central cyanosis refers to a generalized blue discoloration of the lips, tongue and sublingual tissues, as well as the hands and feet. There is always a systemic cause for its development, causing hypoxemia (low oxygen levels). This is the most dangerous type of cyanosis. Peripheral cyanosis causes a bluish discoloration of the arms and legs and is accompanied by vasoconstriction and decreased peripheral blood flow. It is believed that mixed cyanosis occurs in the presence of both central and peripheral causes. Cyanosis due to abnormal pigmentation occurs when abnormal pigment appears in the blood due to medication or another reason, which gives the tissues a dark color. Peripheral cyanosis is almost always caused by decreased blood circulation in the affected limbs, causing the tissues to lack oxygen. Oxygen-rich blood is bright red, while oxygen-poor blood is dark red, reflecting a bluish cherry color through the skin.
Why do symptoms of cyanosis occur?
Any activity or serious illness that prevents blood from returning to the heart through the veins or interferes with its flow to tissues and organs can lead to peripheral cyanosis. Some of the main factors leading to blue hands and feet include:
- Tight clothing or tight jewelry.
- Deep vein thrombosis (DVT).
- Venous insufficiency, caused by conditions that slow blood flow through the veins.
- Raynaud's phenomenon.
- Lymphedema.
- Heart failure.
- Arterial insufficiency caused by diseases that slow blood flow through the arteries.
- Severe hypotension or extremely low blood pressure.
Characteristic symptoms of peripheral cyanosis are as follows:
- The skin on the tips of your fingers, toes, palms, or soles becomes bluish-cherry.
- The affected part of the body feels cold to the touch.
- The color returns to normal after the body part is warmed up.
However, if a person develops any serious complications, such as shortness of breath, chest pain, or severe dizziness, emergency medical attention must be sought immediately to prevent any serious consequences.
Diagnosis of the causes of bluish skin
Bluish skin is not usually a sign of serious illness. However, if your skin color does not return to normal, it is important to find out the reason. A doctor can determine the underlying cause through a physical examination, listening to the heart and lungs, and blood tests. CT scans and x-rays can determine if there are abnormalities in the lungs and heart. A non-invasive pulse oximeter is a useful tool for measuring oxygen saturation in the blood, although it cannot help determine oxygen metabolism or the amount of oxygen a person uses. Peripheral cyanosis can also be diagnosed using arterial blood gas analysis. This test measures the levels of acidity, carbon dioxide and oxygen in the blood.
What to do with cyanosis
Treatment for peripheral cyanosis depends on the underlying cause.
Doctors may prescribe certain medications to treat heart and lung conditions. These medications help improve blood flow and oxygen supply to organs and tissues. Some people may require oxygen therapy to restore normal oxygen levels. Doctors may tell a person with peripheral cyanosis to stop taking any medications that restrict blood flow. Medications include beta blockers, birth control pills, and some allergy medications. The doctor may also recommend that the patient make radical lifestyle changes, such as quitting smoking or drinking caffeine. Text: Alena Paretskaya.
HOW TO GET RID OF CYANOSIS?
The treatment tactics for cyanosis always come down to three levels of exposure.
- Urgent identification of the provocateur and treatment of critical illness.
- Oxygen treatment (cocktails, tents, procedures).
- Maintenance treatment. This includes exercises, aqua physiotherapy, massage.
Actually, the treatment of cyanosis is based on the elimination of hypoxia - oxygen deficiency in the blood transport system. Treatment should be carried out with mandatory procedural oxygen support and LOP. The patient himself must comply with a number of conditions for treatment of both the related and the underlying disease.
The first is giving up dangerous habits (alcohol, smoking) - treatment of cardiac and respiratory mechanisms without this is ineffective. The second is building a rest schedule (here – treatment through auto-training and self-massage). Third, a strict treatment regimen for the underlying disease (antibacterial, anti-inflammatory therapy).
Risk group
People most often affected by cyanosis are:
- abuse alcohol;
- smoke a lot;
- do not eat properly, eat a lot of fatty foods (cholesterol levels increase);
- experience severe emotional shocks and are in a state of stress for a long time;
- suffered leg injuries;
- suffer from hypertension, diabetes mellitus;
- frostbitten limbs;
- suffer from varicose veins;
- little rest.
Elderly or, conversely, childhood and pregnancy are also risk factors for the development of cyanosis.
Blue discoloration of the nasolabial triangle
Blue discoloration of the nasolabial triangle.
Very often, parents turn to the pediatrician with complaints about blue discoloration around the lips, or, as it would be more correct to say, cyanosis of the nasolabial triangle. What is this and is it worth worrying about this issue, we will now consider.
The nasolabial triangle is an area on the face limited by the nasolabial folds on the sides, the nose above and the lips below. Cyanosis can be caused by physiological (i.e., occurs in absolutely healthy babies) and pathological (various diseases) conditions of the body.
Physiological conditions.
In the area of the nasolabial triangle, the blood supply is highly developed: both arterial and venous vessels are present. And the skin of infants and young children is very thin and delicate, so the vascular plexuses seem to “shine through” through it and it appears bluish.
Baby crying . Sometimes mothers note that cyanosis appears when crying or prolonged screaming. This is due to the peculiarity of the pulmonary system in newborns. At this time, the level of oxygen in the body decreases (its amount can decrease by up to 92%), and the capillaries expand from tension and are therefore clearly visible through thin skin. In medicine, this phenomenon is called pulmonary cyanosis, and does not pose any threat to health. It disappears when the baby calms down. As the child grows up and lung function improves, this symptom goes away.
Feeding. Sucking at the breast is a big burden for the baby, during which capillaries appear and become visible near the surface of the skin. After feeding, the blueness goes away immediately.
Low air temperature . When your baby is cold, some parts of the body, including the nasolabial triangle, may turn blue. This is due to the imperfect heat exchange system of the child’s body. As soon as the baby warms up, the skin will take on a natural color. The same thing happens while walking. If you notice a blue nasolabial triangle, it’s time to leave the street, because this may be the first sign of hypothermia in a child.
We have reviewed with you the physiological conditions of cyanosis of the nasolabial triangle in children, which are not associated with the manifestation of any diseases. What pathological conditions can lead to the appearance of this symptom?
Pathological conditions.
Respiratory diseases. Respiratory diseases that can lead to cyanosis of the nasolabial triangle include ARVI, pneumonia, bronchial asthma, obstructive or allergic bronchitis, that is, those that lead to impaired air exchange. Of course, along with cyanosis, other symptoms of these diseases should be present (fever, nasal discharge, prolonged dry cough). In this case, you cannot do without consulting a pediatrician, who in turn can refer you to other specialized specialists.
Foreign objects. This is another common cause of cyanosis of the nasolabial triangle. Little children are very curious. Their taste buds are best developed, and therefore they experience the whole world through their mouth. Everything that interests them ends up in the mouth - one careless breath and a tiny object ends up in the respiratory tract. The child begins to cough heavily and gasp for air. It is necessary to provide first aid and call an ambulance.
First aid for a foreign body in the respiratory tract : Turn the child face down and tap the back with force, but not excessively. It is better to carry out manipulations over a sofa or armchair so that the baby does not fall on the floor and accidentally slip out of your hands.
Second option. Sit in a chair or chair. Place your baby face down on your left knee. Your left palm should be on his chest and support his neck. With your right hand, make strong pushes with the edge of your palm between the shoulder blades towards the mouth. Additionally, induce vomiting in the child by pressing your fingers on the root of the tongue. Follow all steps until the ambulance arrives.
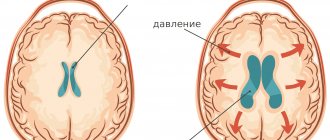
Neurological pathology. Very often, cyanosis can be observed in children who experienced hypoxia or asphyxia during birth (for example, when entwined with the umbilical cord), and were also born premature. We see a blue nasolabial triangle in children with increased intracranial pressure and immature brain structures. In any case, consultation with a neurologist is necessary.
Congenital heart defects . Cyanosis of the nasolabial triangle in a child is one of the first signs of congenital heart disease and heart failure. To clarify the diagnosis and timely treatment, it is necessary to conduct an echocardiogram (ultrasound of the heart), an ECG and consult a cardiologist.
Problems with the development of the respiratory system. Malformations of the bronchopulmonary system (tracheal stenosis, bronchial hypoplasia, etc.) can also lead to cyanosis of the nasolabial triangle. Such conditions require urgent treatment.
Poisoning with drugs or chemicals. Poisoning causes tissue hypoxia, which is manifested by impaired absorption of oxygen by cells, hence cyanosis of the nasolabial triangle. Cyanosis will also be observed in children in whose presence their parents smoke, as a consequence of nicotine intoxication.
If the doctor, after examining the baby, did not find any pathologies and recognized cyanosis of the nasolabial triangle as normal, the following measures should be taken so that the blue discoloration disappears as soon as possible.
Be sure to take your child for a walk in the fresh air every day. Long walks will not only strengthen the baby’s body, but also saturate it with oxygen. And if there is no deficiency, then the nasolabial triangle will not turn blue.
Don't let your baby cry for too long. This is harmful not only to the physical health, but also to the emotional comfort of the child. Crying is a form of communication accessible to the baby to the mother. By crying, the child tries to draw her attention to some factors that cause him discomfort (wet diaper, hunger, loneliness and others). Provide him with everything he needs.
Monitor the air temperature in your baby's room. It should not be too hot or cold. Ideally - 21-25 degrees. If your child starts to feel cold, just dress him warmly (in clothes made from natural fabrics so that the skin can breathe).
Prevention
Doctors include preventive measures to avoid the development of local/diffuse cyanosis:
- giving up alcoholic drinks and smoking;
- maintaining an active lifestyle (swimming, long walks, running, trips to nature, exercise therapy, outdoor games are useful);
- balanced diet (you need to eat more plant foods);
- regular preventive medical examinations;
- avoiding hypothermia;
- competent treatment of existing chronic diseases.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Diagnostics
To identify the cause of cyanosis, the doctor determines the area of its localization, listens to the patient’s complaints and analyzes his medical history. The following points must be clarified:
- when and under what circumstances did cyanosis occur;
- how the bluish tint changes during the day or under the influence of some factors;
- cyanosis appears constantly or periodically.
After this, the specialist listens to the lungs and heart. To obtain more detailed data, the following types of laboratory and instrumental diagnostics may be prescribed:
- blood gas analysis;
- clinical blood test;
- pulse oximetry;
- spirography;
- ECG;
- chest x-ray;
- Echo-CG;
- CT scan of the chest.
After diagnosis, the patient may be recommended other types of examinations to create a more effective treatment plan for the underlying disease.
Treatment
The main goal of treatment when cyanosis is detected is aimed at eliminating the underlying disease. And to eliminate oxygen starvation, the patient may be prescribed oxygen therapy and certain medications.
Oxygen therapy
A person with acute cyanosis is indicated for oxygen therapy, possibly in a pressure chamber.
Additional oxygen supply to the patient’s body allows the blood to be saturated with oxygen and reduces the bluishness of the skin. However, this method of treatment is effective only for acute cyanosis. In the chronic presence of cyanosis (for example, with heart disease or anemia), eliminating tissue hypoxia in this way will be a temporary measure, and to treat the underlying disease, the patient must undergo a course of conservative or surgical treatment.
Oxygen therapy can be carried out using:
- oxygen mask (simple, non-reversible or Venturi);
- nasal catheters;
- oxygen tent;
- artificial lung ventilation device;
- barotherapy.
The method of supplying the oxygen mixture to the body is determined individually and depends on the clinical case. Oxygen therapy can be carried out both in a hospital setting and at home (using portable oxygen cylinders or concentrators).
For health purposes, the patient may be recommended oxygen therapy techniques such as taking oxygen cocktails or baths.
Drug therapy
To eliminate cyanosis and oxygen starvation of tissues, patients may be prescribed medications that normalize blood flow, enhance erythropoiesis, the activity of the heart and lungs, or improve blood flow. The goal of such drug therapy is to improve the supply of oxygen and its delivery to tissues suffering from hypoxia.
To reduce the manifestations of cyanosis, the following may be prescribed:
- respiratory analeptics - Cititon, Etimizol, etc.;
- bronchodilators - Berodual, Salmbutamol, etc.;
- cardiac glycosides – Korglykon, Strophanthin;
- neuroprotectors – Piracetam, Nootropil, Phezam, etc.;
- anticoagulants – Fragmin, Warfarin, etc.;
- vitamin preparations.
If cyanosis is caused by a chronic disease, then after treatment the patient is recommended to undergo clinical observation. Such constant monitoring of the course of the disease allows timely adjustment of therapy and prevent the development of more severe cases of tissue hypoxia.
Cyanosis of the skin and mucous membranes is a symptom of many diseases, but is more often detected in pathologies of the respiratory organs, heart or blood vessels. Its appearance should always be a reason to consult a doctor. To eliminate the causes of its occurrence, the patient should undergo a comprehensive diagnosis, the data of which will allow the doctor to draw up the most productive treatment plan. In some cases, with the sudden appearance and rapid increase of cyanosis, cyanosis indicates the development of a critical condition and requires emergency assistance and calling an ambulance.