Heart failure
Heart failure is an acute or chronic condition caused by a weakening of myocardial contractility and congestion in the pulmonary or systemic circulation. It manifests itself as shortness of breath at rest or with slight exertion, fatigue, swelling, cyanosis (blueness) of the nails and nasolabial triangle. Acute heart failure is dangerous due to the development of pulmonary edema and cardiogenic shock, while chronic heart failure leads to the development of organ hypoxia. Heart failure is one of the most common causes of human death.
Classification of heart failure
According to the nature of the course, the classification of heart failure involves division into:
- spicy;
- chronic.
Acute heart failure
According to ICD-10, the code corresponds to I50.9 Heart failure, unspecified. Acute circulatory failure often leads to death (death) in the absence of timely, competent therapy.
Acute heart failure occurs suddenly, minutes or hours after a heart attack, when the body can no longer compensate. Some symptoms include:
- severe difficulty breathing and/or coughing;
- Gurgling sound when breathing;
- Heart rhythm disturbances;
- Pallor;
- Cold sweat.
The development of acute heart failure can occur in two types:
- left type (acute left ventricular or left atrial failure);
- acute right ventricular failure.
Chronic heart failure
Chronic heart failure is a consequence of cardiovascular diseases. It develops gradually and progresses slowly. The wall of the heart thickens due to the growth of the muscle layer. The formation of capillaries that supply nutrition to the heart lags behind the growth of muscle mass. The nutrition of the heart muscle is disrupted, and it becomes stiff and less elastic. The heart cannot cope with pumping blood.
Short description
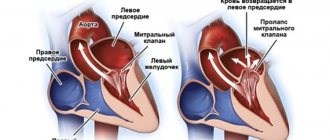
Mitral regurgitation is the inability of the left atrioventricular valve to prevent the reverse flow of blood from the left ventricle into the left atrium during ventricular systole.
Code according to the international classification of diseases ICD-10:
- I05.1 Rheumatic mitral valve insufficiency
- I05.2 Mitral stenosis with insufficiency
- I34.0 Mitral (valve) insufficiency
- Q23.3 Congenital mitral regurgitation
Frequency. Mitral insufficiency is recorded in 50% of patients with various heart defects. In its pure form, mitral regurgitation is a rare disease. It is observed much more often in children than in adults. Often combined with mitral stenosis or aortic valve defects. Congenital mitral valve insufficiency accounts for 0.6% of all congenital heart diseases. In 65% of cases it is combined with septal defects, coarctation of the aorta or patent ductus arteriosus. About 5–6% of healthy women have some degree of mitral regurgitation detected by echocardiography.
How is chronic heart failure classified?
In all cases when heart failure (symptoms and organ disorders) develops slowly, it is said to be chronic. As symptoms increase, this option is divided into stages. So, according to Vasilenko-Strazhesko there are three of them.
I (initial) stage - hidden signs of circulatory failure, manifested only during physical activity by shortness of breath, palpitations, excessive fatigue; at rest there are no hemodynamic disturbances.
Stage II (severe) – signs of prolonged circulatory failure and hemodynamic disorders (congestion of the pulmonary and systemic circulation) are expressed at rest; severe limitation of working capacity:
- Period II A – moderate hemodynamic disturbances in one part of the heart (left or right ventricular failure). Shortness of breath develops during normal physical activity, and performance is sharply reduced. Objective signs are cyanosis, swelling of the legs, initial signs of hepatomegaly, hard breathing.
- Period II B – deep hemodynamic disorders involving the entire cardiovascular system (large and small circle). Objective signs – shortness of breath at rest, severe edema, cyanosis, ascites; complete disability.
III (dystrophic, final) stage – persistent circulatory and metabolic failure, morphologically irreversible damage to the structure of organs (liver, lungs, kidneys), exhaustion.
Depending on the symptoms that appear at different stages of the disease, the severity of the patient, functional classes (types) of heart failure are distinguished:
I – the disease does not have any effect on the patient’s quality of life. Heart failure is stage 1 and does not limit the patient’s physical activity in any way. Stage 1 deficiency responds well to therapy.
II – the patient is not bothered by anything at rest; mild restrictions are recorded during physical activity.
III – there are no symptoms at rest, but there is a noticeable decrease in performance.
IV – chest pain and signs of heart failure are recorded at rest, the patient is partially or completely incapacitated.
Symptoms of heart failure
In the initial stages, symptoms of heart failure occur only during physical activity. Shortness of breath appears - breathing becomes too frequent and deep, and does not correspond to the severity of work or physical exercise. If the pressure in the vessels of the lungs increases, the patient is bothered by a cough, sometimes with blood.
After physical exertion, heavy meals and in a lying position, increased heart rate occurs. The patient complains of increased fatigue and weakness.
Over time, these symptoms intensify and begin to bother you not only during physical work, but also at rest.
Many patients with heart failure have decreased urine output and go to the toilet mostly at night. In the evenings, swelling appears on the legs, at first only on the feet, and over time it “rises” higher. The skin of the feet, hands, earlobes and tip of the nose takes on a bluish tint. If heart failure is accompanied by stagnation of blood in the liver vessels, a feeling of heaviness and pain occurs under the right rib.
Over time, heart failure leads to poor circulation in the brain. The patient becomes irritable, quickly gets tired during mental stress, and often becomes depressed. He sleeps poorly at night and is constantly sleepy during the day.
Symptoms of right ventricular acute heart failure are caused by stagnation of blood in the veins of the systemic circulation:
- Increased heartbeat is the result of deterioration of blood circulation in the coronary vessels of the heart. Patients experience increasing tachycardia, which is accompanied by dizziness, shortness of breath and heaviness in the chest.
- Swelling of the neck veins, which increases with inspiration, is explained by an increase in intrathoracic pressure and difficulty in blood flow to the heart.
- Edema. A number of factors contribute to their appearance: slower blood circulation, increased permeability of capillary walls, interstitial fluid retention, and impaired water-salt metabolism. As a result, fluid accumulates in cavities and limbs.
- A decrease in blood pressure is associated with a decrease in cardiac output. Manifestations: weakness, pallor, increased sweating.
- There is no congestion in the lungs.
Chronic heart failure develops in the right and left atrial, right and left ventricular types. Chronic heart failure, according to various authors, is observed in 0.5–2% of the population. The incidence increases with age; after 75 years, the pathology occurs in 10% of people. Chronic left ventricular failure develops as a complication of coronary heart disease, arterial hypertension, mitral valve insufficiency, aortic disease and is associated with stagnation of blood in the pulmonary circulation. It is characterized by gas and vascular changes in the lungs.
Clinically manifested:
- increased fatigue;
- dry cough (rarely with hemoptysis);
- attacks of palpitations;
- cyanosis;
- attacks of suffocation, which often occur at night;
- shortness of breath.
In chronic left atrial insufficiency in patients with mitral valve stenosis, congestion in the pulmonary circulation system is even more pronounced. The initial signs of heart failure in this case are cough with hemoptysis, severe shortness of breath and cyanosis. Gradually, sclerotic processes begin in the vessels of the small circle and in the lungs. This leads to the creation of an additional obstacle to blood flow in the pulmonary circle and further increases the pressure in the pulmonary artery basin. As a result, the load on the right ventricle increases, causing the gradual formation of its failure.
Chronic right ventricular failure usually accompanies emphysema, pneumosclerosis, mitral heart defects and is characterized by the appearance of signs of blood stagnation in the systemic circulatory system. Patients complain of shortness of breath during exercise, enlargement and distension of the abdomen, a decrease in the amount of urine discharge, the appearance of edema of the lower extremities, heaviness and pain in the right hypochondrium.
Publications in the media
Mitral regurgitation is the inability of the left atrioventricular valve to prevent the reverse flow of blood from the left ventricle into the left atrium during ventricular systole.
Frequency. Mitral insufficiency is recorded in 50% of patients with various heart defects. In its pure form, mitral regurgitation is a rare disease. It is observed much more often in children than in adults. Often combined with mitral stenosis or aortic valve defects. Congenital mitral valve insufficiency accounts for 0.6% of all congenital heart diseases. In 65% of cases it is combined with septal defects, coarctation of the aorta or patent ductus arteriosus. About 5–6% of healthy women have some degree of mitral regurgitation detected by echocardiography.
Etiology • Rheumatism • Isolated mitral valve prolapse (myxomatous degeneration, Barlow's disease) • Idiopathic rupture of chordae (14–23% of cases of severe insufficiency, of which degenerative changes of the chordae are detected in 73–93% of cases) • Ischemic dysfunction or rupture of papillary muscles (5 % cases of transmural MI, more often with lower MI) • Infective endocarditis • Annular calcification of the elderly • Connective tissue diseases (Marfan and Ehlers-Danlos syndrome) • Complication of mitral valvuloplasty • Relative failure due to dilatation or submitral aneurysm of the left ventricle • Congenital forms of failure (e.g. due to splitting of the anterior leaflet of the mitral valve with a fully open AV canal).
Pathophysiology • Hemodynamics in acute regurgitation are significantly different from those in the chronic course of the disease, when compensatory hypertrophy and dilatation of the left ventricle, the degree of which depends on the severity of mitral regurgitation, maintain cardiac output, sometimes for many years • In acute mitral regurgitation (for example, due to rupture of the papillary muscle or chordae) the left ventricle does not have time to adapt to a sharp increase in preload. As a result of this, and also due to the low compliance of the normal left atrium, acute left ventricular failure occurs, leading to pulmonary edema and arterial hypotension • With chronically existing regurgitation, due to an increase in the volume load of the left atrium, its hypertrophy and dilation occurs, more pronounced than with mitral stenosis, leading to chronic stagnation in the pulmonary circulation • Often, with dilatation of the left atrium, paroxysmal or permanent form of atrial fibrillation occurs, as well as thrombosis of the left atrium.
Clinical picture and diagnosis . • During chronic mitral regurgitation, three periods are conventionally distinguished: compensation, pulmonary venous hypertension and right ventricular failure. • Complaints •• During the compensation period, an asymptomatic course can be observed for several years •• When clinical symptoms appear in patients, the most common complaints are shortness of breath (98%), fatigue (87%), hemoptysis (15%) •• With severe regurgitation there are symptoms of compression of the recurrent laryngeal nerve by the enlarged left atrium (the most common of them is Ortner's syndrome - hoarseness of voice), and during the period of right ventricular failure - by the pulmonary trunk •• In patients in the third stage - symptoms of stagnation in the systemic circulation (edema, enlarged liver, Plesch's sign, swelling of the jugular veins).
• Peripheral symptoms are due to small output syndrome - see Aortic valve insufficiency. • Valve symptoms •• Mesosystolic click occurs with mitral valve prolapse, separation of chords or papillary muscle •• Weakening of the first tone •• Systolic murmur over the apex of various timbres, carried out to Botkin’s point and the left axillary region; its intensity depends on the volume of regurgitation •• The most specific sign of a mitral regurgitation murmur is intensification or appearance during tests that reduce the volume of the left ventricle (Valsalva maneuver, orthostatic test), or in a clinostatic position when turning to the left side due to the closer location of the apex of the heart to the chest •• Systolic flutter over the apical region - with high velocity (usually fine jet) regurgitation •• Coombs murmur occurs due to relative stenosis of the mitral valve due to the increased volume of blood expelled from the left atrium.
• Symptoms associated with enlargement of the chambers of the heart • Increase in the boundaries of relative dullness to the left, up and to the right (with dilatation of the right sections) • Popov's symptom - different degrees of filling of the pulse in the radial arteries. • Symptoms of the underlying disease (rheumatism, Marfan syndrome, cardiomyopathy).
Special studies • ECG •• Signs of hypertrophy and overload of the left parts of the heart, primarily the left atrium, and in the third stage of the disease and the right parts of the heart •• Supraventricular tachyarrhythmias (atrial fibrillation and flutter, supraventricular extrasystole and tachycardia).
• X-ray of the chest organs •• Pronounced signs of pulmonary venous hypertension • Bulging of the arch of the left atrium and deviation of the contrasted esophagus along an arc of a large radius •• Bulging of the arch of the left ventricle •• In the third stage of the disease - signs of pulmonary hypertension and bulging of the arches of the right parts of the heart •• With compression of the pulmonary trunk by the dilated left atrium - weakening of the pulmonary pattern on the left •• With fluoroscopy in direct projection - a symptom of a “rocker arm” between the arches of the left ventricle and the left atrium.
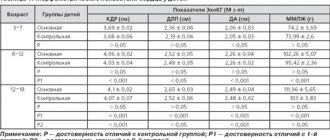
• Echocardiography •• Hypertrophy and dilatation of the left heart, especially the left atrium •• Visualization of a flapping leaflet when the chordae or papillary muscle is avulsed •• Increased end-diastolic index (EDI = [end-diastolic volume of the left ventricle] / [body surface area]), degree which has prognostic significance: an increase in CDI above 30 ml/m2 is associated with postoperative left ventricular failure, above 90 ml/m2 - with high postoperative mortality •• In Doppler mode - the flow of mitral regurgitation, the volume of which (estimated in the color mapping mode) corresponds to the degree severity of the defect •• In the third stage of the disease - hypertrophy and dilation of the right heart, increased systolic pressure in the right ventricle •• Transesophageal echocardiography is performed to detect thrombosis of the left atrium in the presence of atrial fibrillation.
• Catheterization of the left and right ventricles •• Increase in end-diastolic pressure of the left ventricle, pressure in the left atrium, systolic pressure in the right atrium, pulmonary artery wedge pressure •• “Ventriculization” of the pulmonary capillary pressure curve (increase in wave V more than 15 mm Hg. ).
• Left ventriculography •• The presence and degree of regurgitation is determined by the degree of filling of the left atrium in one contraction with contrast injected into the left ventricle •• Combined valvular lesions are also diagnosed.
TREATMENT • Drug therapy •• Chronic mitral regurgitation ••• Asymptomatic mild and moderate mitral regurgitation does not require treatment, and the advisability of taking vasodilators is controversial ••• Asymptomatic severe compensated regurgitation (CDI less than 50 ml/m2, absence of pulmonary hypertension and normal left ventricular systolic function , negative stress tests): invasive studies of hemodynamics at rest and during stress tests are indicated, as well as continuous use of ACE inhibitors •• Acute mitral regurgitation ••• Vasodilators (sodium nitroprusside or ACE inhibitors) and IV diuretics ••• Intra-aortic balloon counterpulsation ••• In case of infective endocarditis, absence of progression of sepsis or severe refractory heart failure, preoperative antibiotic therapy is permissible for no longer than 3 days ••• In case of severe failure due to MI without rupture of the papillary muscles - intra-aortic balloon counterpulsation, vasodilators.
• Surgical treatment •• Indications ••• Severe mitral regurgitation, asymptomatic or functional class II, if the end-diastolic size of the left ventricle is more than 40 mm or the CDI is more than 40 ml/m2, or the left ventricular ejection fraction is less than 55–60% (with mitral insufficiency, if the contractile function of the left ventricle is not impaired, the left ventricular ejection fraction should not be lower than 65%) ••• Severe mitral regurgitation, functional class III–IV ••• Severe asymptomatic mitral regurgitation in combination with severe pulmonary hypertension ••• Symptomatic moderate failure with preserved systolic function of the left ventricle in case of positive results of an invasive hemodynamic study •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life ••• End-stage circulatory failure ••• Negative test result with aminophylline and oxygen •• Methods of surgical treatment ••• In the absence of calcification and preserved mobility of the leaflets and valve apparatus, it is permissible to perform valve-sparing interventions (annuloplasty with the Alain Carpentier ring or using the “double hole” technique, excision of the flapping portion of the posterior leaflet, shortening of the chordae) ••• Despite the greater physiology of valve-sparing operations and relatively low incidence of thrombosis and infective endocarditis, due to the high frequency of relapses of the defect and the need for repeated operations, plastic interventions on the valves are actually performed only in cases of prolapse, ruptures of valve structures, relative valve insufficiency during dilatation of its ring and before a planned pregnancy ••• Mitral valve replacement valves under conditions of artificial circulation using biological prostheses are performed on children or before a planned pregnancy ••• In other cases, the affected valve is replaced with a mechanical prosthesis.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Atrioventricular block • Dystrophic changes in biological prostheses and the need for repeated prosthetics. Prognosis • Only 5–10% of patients with mitral valve prolapse progress to mitral regurgitation • 5-year survival rate is more than 80%, 10-year survival rate is more than 60% • With ischemic genesis of the defect, 5-year survival rate does not exceed 30% • Surgical treatment improves survival and exercise tolerance if the initial left ventricular ejection fraction is more than 35%, cardiac index is more than 1.5 ml/min/m2 • Surgical treatment is ineffective for secondary mitral regurgitation due to dilated cardiomyopathy and primary - for left ventricular ejection fraction less than 30% • Surgical treatment is often effective for ischemic cardiomyopathy when coronary artery bypass grafting and annuloplasty are performed simultaneously • Mortality with mitral valve replacement is 2-7%, with annuloplasty - 1-4% • 5-year survival rate averages 90%.
Synonyms • Left atrioventricular valve insufficiency • Mitral valve insufficiency
Abbreviations. EDI - end diastolic index.
ICD-10 • I05.1 Rheumatic mitral valve insufficiency • I05.2 Mitral stenosis with insufficiency • I34.0 Mitral (valve) insufficiency • Q23.3 Congenital mitral insufficiency
Causes of heart failure
The main causes of heart failure are:
- coronary heart disease and myocardial infarction;
- dilated cardiomyopathy;
- rheumatic heart defects.
In elderly patients, the causes of heart failure are often type II diabetes mellitus and arterial hypertension. Type 2 diabetes mellitus can lead to the development of heart failure.
There are a number of factors that can reduce the compensatory mechanisms of the myocardium and provoke the development of heart failure. These include:
- pulmonary embolism (PE);
- severe arrhythmia;
- psycho-emotional or physical stress;
- progressive coronary heart disease;
- hypertensive crises; acute and chronic renal failure;
- severe anemia;
- pneumonia; severe ARVI;
- hyperthyroidism;
- long-term use of certain medications (adrenaline, ephedrine, corticosteroids, estrogens, non-steroidal anti-inflammatory drugs);
- infective endocarditis;
- rheumatism; myocarditis;
- a sharp increase in the volume of circulating blood due to incorrect calculation of the volume of intravenously administered fluid;
- alcoholism;
- rapid and significant weight gain.
Eliminating risk factors can prevent the development of heart failure or slow its progression.
How is heart failure diagnosed?
Diagnosis begins with a comprehensive assessment of a person's medical history, paying particular attention to symptoms (onset, duration, manifestation). This helps classify the severity of the symptom. The heart and lungs are examined. If a heart attack or rhythm disorder is suspected, a 12-lead resting ECG is performed. In addition, echocardiography and complete blood count. The need for catheterization is determined individually.
In diagnosis, you need to start with analyzing complaints and identifying symptoms. Patients complain of shortness of breath, fatigue, and palpitations.
The doctor asks the patient:
- How does he sleep?
- Has the number of pillows changed over the past week?
- Did the person begin to sleep sitting instead of lying down?
The second stage of diagnosis is a physical examination, including:
- Skin examination;
- Assessment of the severity of fat and muscle mass;
- Checking for edema;
- Pulse palpation;
- Palpation of the liver;
- Auscultation of the lungs;
- Auscultation of the heart (1st sound, systolic murmur at the 1st point of auscultation, analysis of the 2nd tone, “gallop rhythm”);
- Weighing (a 1% decrease in body weight over 30 days indicates the onset of cachexia).
If heart failure is suspected, the electrolyte and gas composition of the blood, acid-base balance, urea, creatinine, cardio-specific enzymes, and indicators of protein-carbohydrate metabolism are determined.
Based on specific changes, an ECG helps to identify hypertrophy and insufficiency of blood supply (ischemia) of the myocardium, as well as arrhythmias. Based on electrocardiography, various stress tests using an exercise bike (veloergometry) and a treadmill (treadmill test) are widely used. Such tests with a gradually increasing level of load make it possible to judge the reserve capabilities of heart function.
Using ultrasound echocardiography, it is possible to determine the cause of heart failure, as well as evaluate the pumping function of the myocardium. Using cardiac MRI, coronary heart disease, congenital or acquired heart defects, arterial hypertension and other diseases are successfully diagnosed. X-ray of the lungs and chest organs in heart failure determines congestive processes in the pulmonary circulation, cardiomegaly.
Diagnostics
Special studies • ECG •• Signs of hypertrophy and overload of the left parts of the heart, primarily the left atrium, and in the third stage of the disease and the right parts of the heart •• Supraventricular tachyarrhythmias (atrial fibrillation and flutter, supraventricular extrasystole and tachycardia).
• X-ray of the chest organs •• Pronounced signs of pulmonary venous hypertension • Bulging of the arch of the left atrium and deviation of the contrasted esophagus along an arc of a large radius •• Bulging of the arch of the left ventricle •• In the third stage of the disease - signs of pulmonary hypertension and bulging of the arches of the right parts of the heart •• With compression of the pulmonary trunk by the dilated left atrium - weakening of the pulmonary pattern on the left •• With fluoroscopy in direct projection - a symptom of a “rocker arm” between the arches of the left ventricle and the left atrium.
• Echocardiography •• Hypertrophy and dilatation of the left heart, especially the left atrium •• Visualization of a flapping leaflet when the chordae or papillary muscle is avulsed •• Increased end-diastolic index (EDI = [end-diastolic volume of the left ventricle] / [body surface area]), degree which has prognostic significance: an increase in CDI above 30 ml/m2 is associated with postoperative left ventricular failure, above 90 ml/m2 - with high postoperative mortality •• In Doppler mode - the flow of mitral regurgitation, the volume of which (estimated in the color mapping mode) corresponds to the degree severity of the defect •• In the third stage of the disease - hypertrophy and dilation of the right heart, increased systolic pressure in the right ventricle •• Transesophageal echocardiography is performed to detect thrombosis of the left atrium in the presence of atrial fibrillation.
• Catheterization of the left and right ventricles •• Increase in end-diastolic pressure of the left ventricle, pressure in the left atrium, systolic pressure in the right atrium, pulmonary artery wedge pressure •• “Ventriculization” of the pulmonary capillary pressure curve (increase in wave V more than 15 mm Hg. ).
• Left ventriculography •• The presence and degree of regurgitation is determined by the degree of filling of the left atrium in one contraction with contrast injected into the left ventricle •• Combined valvular lesions are also diagnosed.
How is heart failure treated?
For chronic heart failure, medications (such as ACE inhibitors, beta blockers and diuretics) are used. Medicines are used to prevent complications and improve quality of life. ACE inhibitors and beta blockers can prolong life, but they must be taken regularly to achieve a beneficial effect.
In addition, rhythm therapy (to treat cardiac arrhythmias) and implantation of a three-chamber pacemaker are used. The latter ensures timely activation of the atria and both ventricles. A defibrillator is also often implanted as part of a pacemaker to counteract dangerous heart rhythm disturbances in the setting of severe heart failure. This treatment is also known as resynchronization therapy. An important part of successful treatment is physical therapy.
In the treatment of heart failure, a properly organized diet plays an important role. Dishes should be easily digestible. The diet should include fresh fruits and vegetables as a source of vitamins and microelements. The amount of table salt is limited to 1-2 g per day, and liquid intake to 500-600 ml.
Pharmacotherapy, which includes the following groups of drugs, can improve the quality of life and prolong it:
- cardiac glycosides – enhance the contractile and pumping function of the myocardium, stimulate diuresis, and increase the level of exercise tolerance;
- ACE inhibitors (angiotensin-converting enzyme) and vasodilators - reduce vascular tone, expand the lumen of blood vessels, thereby reducing vascular resistance and increasing cardiac output;
- nitrates - dilate the coronary arteries, increase cardiac output and improve blood filling of the ventricles;
- diuretics – remove excess fluid from the body, thereby reducing swelling;
- β-blockers - increase cardiac output, improve the filling of the heart chambers with blood, reduce the heart rate;
- anticoagulants - reduce the risk of blood clots in blood vessels and, accordingly, thromboembolic complications;
- agents that improve metabolic processes in the heart muscle (potassium supplements, vitamins).
If cardiac asthma or pulmonary edema (acute left ventricular failure) develops, the patient requires emergency hospitalization.
Prescribed drugs that increase cardiac output, diuretics, nitrates. Oxygen therapy is mandatory. Removal of fluid from body cavities (abdominal, pleural, pericardial) is carried out by puncture.
Causes
Etiology • Rheumatism • Isolated mitral valve prolapse (myxomatous degeneration, Barlow's disease) • Idiopathic rupture of chordae (14–23% of cases of severe insufficiency, of which degenerative changes of the chordae are detected in 73–93% of cases) • Ischemic dysfunction or rupture of papillary muscles (5 % cases of transmural MI, more often with lower MI) • Infective endocarditis • Annular calcification of the elderly • Connective tissue diseases (Marfan and Ehlers-Danlos syndrome) • Complication of mitral valvuloplasty • Relative failure due to dilatation or submitral aneurysm of the left ventricle • Congenital forms of failure (e.g. due to splitting of the anterior leaflet of the mitral valve with a fully open AV canal).
Pathophysiology • Hemodynamics in acute regurgitation are significantly different from those in the chronic course of the disease, when compensatory hypertrophy and dilatation of the left ventricle, the degree of which depends on the severity of mitral regurgitation, maintain cardiac output, sometimes for many years • In acute mitral regurgitation (for example, due to rupture of the papillary muscle or chordae) the left ventricle does not have time to adapt to a sharp increase in preload. As a result of this, and also due to the low compliance of the normal left atrium, acute left ventricular failure occurs, leading to pulmonary edema and arterial hypotension • With chronically existing regurgitation, due to an increase in the volume load of the left atrium, its hypertrophy and dilation occurs, more pronounced than with mitral stenosis, leading to chronic stagnation in the pulmonary circulation • Often, with dilatation of the left atrium, paroxysmal or permanent form of atrial fibrillation occurs, as well as thrombosis of the left atrium.
Prevention and prognosis
To prevent heart failure, you need proper nutrition, sufficient physical activity, and giving up bad habits. All diseases of the cardiovascular system must be promptly identified and treated.
The prognosis in the absence of treatment for CHF is unfavorable, since most heart diseases lead to its wear and tear and the development of severe complications. When carrying out drug and/or cardiac surgery, the prognosis is favorable, because the progression of the insufficiency slows down or a radical cure for the underlying disease occurs.