Short description
Atrial septal defect (ASD) is a congenital heart defect with communication between the atria. Statistical data: 7.8% of all congenital heart disease detected in infancy, and 30% in adults; VSD of the ostium secundum type - 70%, ostium primum - 15%, sinus venosus - 15%; Lutembashe syndrome accounts for 0.4% of all cases of ASD, the combination of ASD with mitral valve prolapse - 10–20%; the predominant gender is female (2:1–3:1).
Code according to the international classification of diseases ICD-10:
- Q21.1 Atrial septal defect
Causes
Etiology: factors that form congenital heart disease (see Tetralogy of Fallot).
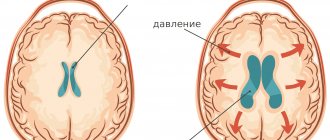
Pathogenesis • The magnitude and direction of shunt depend on the size of the defect and the relative compliance of the ventricles • In adults, the right ventricle is more compliant than the left, as a result of which shunt occurs from the left atrium to the right • A small shunt leads to a moderate volume overload of the right heart, and pressure in the pulmonary artery remains normal • The severity of pulmonary hypertension may be insignificant even with a large shunt • Only in rare cases does severe pulmonary hypertension develop, leading to right ventricular failure and right-to-left shunt • Unlike VSD, with ASD the shunt is smaller and affects only the right side of the heart.
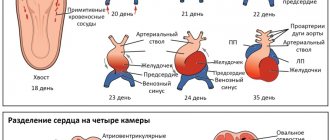
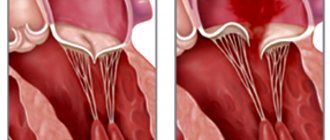
Variants of ASD • Ostium secundum (secondary defects) are localized in the area of the oval fossa, are often multiple, accompany many syndromes: Holt-Oram syndrome (ASD of the ostium secundum type in combination with digital hypoplasia), Lutembashe syndrome (combination of ASD with mitral valve stenosis), combination of ASD with mitral valve prolapse, etc. • Ostium primum (primary defects) are usually large in size, localized in the lower part of the septum, at the attachment point of the mitral and tricuspid valves, interatrial and interventricular septa. They are part of an open AV canal and are often combined with abnormal drainage of the pulmonary veins, splitting of the anterior mitral valve leaflet, mitral regurgitation and Down syndrome • Defects of the sinus venosus type are localized near the mouth of the superior vena cava and the sinus node, often combined with sick sinus syndrome, AV - nodal rhythm and abnormal drainage of the pulmonary veins.
Symptoms (signs)
Clinical picture
Complaints: shortness of breath, palpitations, fatigue during physical activity, retarded physical development, frequent infections, paradoxical embolisms.
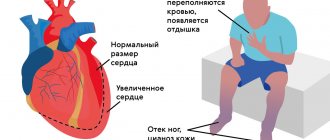
Objectively • Pallor of the skin • Harrison's furrows - displacement of areas of the chest as a result of chronic shortness of breath • Splitting of the first tone with a pronounced component of the tricuspid valve • Pronounced fixed splitting of the second tone (pronounced - due to - due to prolongation of the time of blood ejection from the right ventricle; fixed - due to - due to the fact that the dependence of venous return on the phases of breathing is leveled by discharge from the left atrium) • An ejection click and a soft systolic murmur of relative stenosis of the pulmonary artery in the second intercostal space to the left of the sternum • Due to an increase in blood flow through the tricuspid valve, a low-frequency diastolic murmur sometimes occurs above the xiphoid process of the sternum.
Let's try to figure it out. Let's start in order
Worry? No, let's first go to a pediatric cardiologist. The pediatrician will give you a referral, and in it there will be a number of completely incomprehensible terms and abbreviations. Let's try to decipher them.
- Functional cardiopathy (FCP) or FIS – functional changes of the heart – is one of the most common diagnoses in pediatric cardiology. The use of this term is not always justified. In fact, FIS refers to any set of minimal deviations from the norm (based on the results of a clinical examination, ECG, EchoCG, etc.) that cannot be combined into any other, more serious diagnosis.
- FSS - functional systolic murmur - in this case, the word “functional” means “not caused by any serious disease,” which is most often found in pediatric practice.
A “heart doctor” – a specialist in heart and vascular diseases – will examine your baby.
He will ask if there are any specific complaints - how the child eats, if he gets tired when sucking, if he turns blue, if he has attacks of shortness of breath, how he gains weight. If the child has grown up and can already speak, is there any pain in the heart area, palpitations, or dizziness? Was there any fainting? He will look carefully to see if there is cyanosis (blueness), shortness of breath, deformation of the chest, fingertips and nails, swelling, or pathological pulsation of blood vessels. He will percuss (knock) to see if the boundaries of the heart are expanded. Palpates (feels) peripheral vessels, the heart area, liver and spleen. He will listen carefully to the heart - how and where it makes noise, what the heart sounds are, where the noise is directed, whether there are any accompanying sounds, and count the frequency of breathing and pulse. And, most likely, he will say that your baby has no signs of circulatory failure (or hemodynamic disorders, or heart failure, which, in general, is almost the same thing). This means that at the moment the child’s heart is doing its job well. Hooray? Hooray. But it’s too early to part with the doctor. Most likely, he will recommend conducting the necessary additional research. For what? And in order to determine where this noise comes from, how to monitor the child, what to fear and in what case to begin treatment.
Diagnostics
Instrumental diagnostics
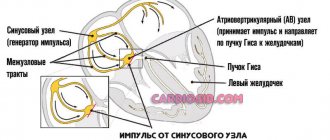
• ECG. Signs of hypertrophy and overload of the left sections, and with pulmonary hypertension - also of the right. With ostium primum, there is a sharp deviation of the EOS to the left due to the displacement of the hypoplastic branch of the left leg of the His bundle forward. Various variants of sick sinus syndrome, AV block. With a defect such as sinus venosus - lower atrial rhythm or AV rhythm - junction.
• Jugular venography: equal amplitude of A and V waves.
• X-ray examination of the chest organs. Strengthening the pulmonary pattern. Expansion and lack of structure of the roots of the lungs, bulging of the right atrium arch and upward displacement of the right cardiovasal angle. Fluoroscopy reveals increased pulsation of the roots of the lungs (a rather specific sign). The “Turkish saber” symptom with concomitant anomalous drainage of the right pulmonary veins into the superior vena cava.
• EchoCG. Hypertrophy and dilatation of the left sections, and with pulmonary hypertension - also of the right. Visualization of ASD in Doppler and B-mode. Differentiation from an open foramen ovale (the anatomical closure of the latter occurs no later than 2 years of life) is the inconsistency of visualization of the discharge in color Doppler mapping and the presence of a leaflet in the cavity of the left atrium. Diagnosis of associated anomalies (abnormal drainage of the pulmonary veins, valvular defects, etc.). The degree of discharge and the ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) are determined. Adults undergo transesophageal echocardiography. With intravenous contrasting of the right parts of the heart, there is a negative contrast effect (displacement of the contrast agent by a stream of blood from the left atrium).
• Radionuclide angiocardiography (first pass method or equilibrium): registration of pathological discharge and its quantitative assessment, diagnosis of concomitant abnormal drainage of the pulmonary veins and ventricular dysfunction.
• Probing of the cardiac cavities •• Indicated for suspected pulmonary hypertension, before open-heart surgery and with conflicting clinical data •• If the catheter can be passed from the right atrium to the left, then this in itself cannot be a sign of an atrial septal defect: sometimes the catheter it is possible to carry out through the open foramen ovale •• Tests are carried out with aminophylline and oxygen inhalation to determine the prognosis regarding the reversibility of pulmonary hypertension •• The ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) is calculated - a reference indicator of the amount of discharge.
• Right atriography, angiopulmonography: flow of contrast from the right atrium to the left; identification of concomitant abnormal pulmonary venous drainage.
Drug therapy. In uncomplicated ASDs of the ostium secundum type, infective endocarditis prophylaxis is usually not carried out. For ASDs of the ostium primum type, large defects of the sinus venosus type, and a combination of ASDs with mitral valve defects, antibiotics are prescribed before and for 6 months after uncomplicated surgical correction. For right ventricular failure, diuretics are prescribed.
Publications in the media
Atrial septal defect (ASD) is a congenital heart defect with communication between the atria. Statistical data: 7.8% of all congenital heart disease detected in infancy, and 30% in adults; VSD of the ostium secundum type - 70%, ostium primum - 15%, sinus venosus - 15%; Lutembashe syndrome accounts for 0.4% of all cases of ASD, the combination of ASD with mitral valve prolapse - 10–20%; the predominant gender is female (2:1–3:1).
Etiology: factors that form congenital heart disease (see Tetralogy of Fallot).
Pathogenesis • The magnitude and direction of shunt depend on the size of the defect and the relative compliance of the ventricles • In adults, the right ventricle is more compliant than the left, as a result of which shunt occurs from the left atrium to the right • A small shunt leads to a moderate volume overload of the right heart, and pressure in the pulmonary artery remains normal • The severity of pulmonary hypertension may be insignificant even with a large shunt • Only in rare cases does severe pulmonary hypertension develop, leading to right ventricular failure and right-to-left shunt • Unlike VSD, with ASD the shunt is smaller and affects only the right side of the heart.
Variants of ASD • Ostium secundum (secondary defects) are localized in the area of the oval fossa, are often multiple, accompany many syndromes: Holt-Oram syndrome (ASD of the ostium secundum type in combination with digital hypoplasia), Lutembashe syndrome (combination of ASD with mitral valve stenosis), combination of ASD with mitral valve prolapse, etc. • Ostium primum (primary defects) are usually large in size, localized in the lower part of the septum, at the attachment point of the mitral and tricuspid valves, interatrial and interventricular septa. They are an integral part of the open AV canal and are often combined with abnormal drainage of the pulmonary veins, splitting of the anterior mitral valve leaflet, mitral regurgitation and Down syndrome • Defects of the sinus venosus type are localized near the mouth of the superior vena cava and the sinus node, often combined with sick sinus syndrome, AV nodal rhythm and abnormal pulmonary venous drainage.
Clinical picture
Complaints: shortness of breath, palpitations, fatigue during physical activity, retarded physical development, frequent infections, paradoxical embolisms.
Objectively • Pallor of the skin • Harrison's furrows - displacement of areas of the chest as a result of chronic shortness of breath • Splitting of the first tone with a pronounced component of the tricuspid valve • Pronounced fixed splitting of the second tone (pronounced - due to prolongation of the time of blood ejection from the right ventricle; fixed - due to - due to the fact that the dependence of venous return on the phases of breathing is leveled by discharge from the left atrium) • Ejection click and soft systolic murmur of relative pulmonary artery stenosis in the second intercostal space to the left of the sternum • Due to increased blood flow through the tricuspid valve, low-frequency diastolic murmur sometimes occurs above the xiphoid process of the sternum.
Instrumental diagnostics
• ECG. Signs of hypertrophy and overload of the left sections, and with pulmonary hypertension - also of the right. With ostium primum, there is a sharp deviation of the EOS to the left due to the displacement of the hypoplastic branch of the left leg of the His bundle forward. Various variants of sick sinus syndrome, AV block. With a sinus venosus type defect, there is an inferior atrial rhythm or an AV junction rhythm.
• Jugular venography: equal amplitude of A and V waves.
• X-ray examination of the chest organs. Strengthening the pulmonary pattern. Expansion and lack of structure of the roots of the lungs, bulging of the right atrium arch and upward displacement of the right cardiovasal angle. Fluoroscopy reveals increased pulsation of the roots of the lungs (a rather specific sign). The “Turkish saber” symptom with concomitant anomalous drainage of the right pulmonary veins into the superior vena cava.
• EchoCG. Hypertrophy and dilatation of the left sections, and with pulmonary hypertension - also of the right. Visualization of ASD in Doppler and B-mode. Differentiation from an open foramen ovale (the anatomical closure of the latter occurs no later than 2 years of life) is the inconsistency of visualization of the discharge in color Doppler mapping and the presence of a leaflet in the cavity of the left atrium. Diagnosis of associated anomalies (abnormal drainage of the pulmonary veins, valvular defects, etc.). The degree of discharge and the ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) are determined. Adults undergo transesophageal echocardiography. With intravenous contrasting of the right parts of the heart, there is a negative contrast effect (displacement of the contrast agent by a stream of blood from the left atrium).
• Radionuclide angiocardiography (first pass method or equilibrium): registration of pathological discharge and its quantitative assessment, diagnosis of concomitant abnormal drainage of the pulmonary veins and ventricular dysfunction.
• Probing of the cardiac cavities •• Indicated for suspected pulmonary hypertension, before open-heart surgery and with conflicting clinical data •• If the catheter can be passed from the right atrium to the left, then this in itself cannot be a sign of an atrial septal defect: sometimes the catheter it is possible to carry out through the open foramen ovale •• Tests are carried out with aminophylline and oxygen inhalation to determine the prognosis regarding the reversibility of pulmonary hypertension •• The ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) is calculated - a reference indicator of the amount of discharge.
• Right atriography, angiopulmonography: flow of contrast from the right atrium to the left; identification of concomitant abnormal pulmonary venous drainage.
Drug therapy. In uncomplicated ASDs of the ostium secundum type, infective endocarditis prophylaxis is usually not carried out. For ASDs of the ostium primum type, large defects of the sinus venosus type, and a combination of ASDs with mitral valve defects, antibiotics are prescribed before and for 6 months after uncomplicated surgical correction. For right ventricular failure, diuretics are prescribed.
Surgery
Indications: Qp/Qs ratio is 1.5 or more, defects of the ostium primum type, large defects of the ostium secundum type, concomitant hemodynamically significant anomalies (abnormal drainage of the pulmonary veins, mitral stenosis, etc.).
Contraindications: severe concomitant pathology that threatens the patient’s life; end-stage circulatory failure, irreversible pulmonary hypertension, the ratio of total pulmonary vascular resistance to peripheral vascular resistance is 0.9 or more.
Methods of surgical treatment. Endovascular correction with a button or two-patch Sideris device or an Amplatz device is feasible for central defects no larger than 2 cm in size. In the absence of experience in endovascular treatment, small defects are sutured under artificial circulation. In other cases, ASD repair with a synthetic or autopericardial patch under artificial circulation is recommended.
Specific postoperative complications • Sick sinus syndrome (after correction of sinus venosus defects) • AV block (after correction of ostium primum defects) • If mitral regurgitation existed before surgery, symptoms may worsen after correction of ASD • Atrial fibrillation that occurred before surgery , as a rule, persists after it.
Forecast. In early childhood the course is benign. In rare cases, severe circulatory disorders can lead to death in the first months of life. Spontaneous closure of the defect is possible before the age of 5. The average life expectancy without treatment is 40 years. 5–15% of patients die before age 30. 10-year survival rate - 90%, 20-year - 88%, 30-year - 67%; 40-year-old - 44%, 50-year-old - 25%, 60-year-old - 13%, 70-year-old - 7%. More than 75% of patients with large defects die from other causes. For uncomplicated defects of the ostium secundum type, perioperative mortality is less than 1%, it is slightly higher for defects of the ostium primum type, the latter also require mitral valve replacement or repair.
Abbreviations. Qp/Qs is the ratio of the pulmonary minute volume of blood flow to the systemic one.
ICD-10 • Q21.1 Atrial septal defect