The child's organ system is formed after conception has occurred, but sometimes a hole forms between the cavities of the heart valves and the process is disrupted. In a newborn with a VSD, blood from the left ventricle ends up in the right ventricle, rather than moving into the aorta, which interferes with the normal functioning of the heart; constant overload of the ventricle provokes the appearance of pulmonary hypertension.
What it is
Normally, the heart ventricles are separated by a muscular barrier already at the time of birth. It not only makes up a third of their total area, but also takes an active part in every contraction and relaxation of the heart. The fetal organs receive only mixed blood. Both ventricles of the newborn are “busy with work” approximately equally, this explains the lack of difference in the thickness of their muscle walls.
Pathogenesis of circulatory disorders in VSD
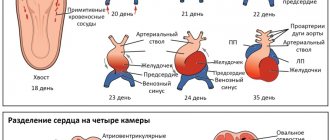
The interventricular septum arises from three different structures, its formation is completed by 4-5 weeks of pregnancy. If fusion does not occur, a hole (defect) remains between the ventricles. It may be the only anomaly in the development of the heart (an isolated defect) or it may be combined with other congenital changes in the anatomy and be part of the structure of a combined defect. Today we are talking only about the first option.
In the first hours of your child’s life, after the baby begins to breathe, his entire blood flow system changes. The inclusion of the systemic and pulmonary circulation “forces” the baby’s heart to restructure its work:
- The pressure in the left ventricle increases significantly.
- With VSD, part of the blood enters not only the aorta, but also the right ventricle, creating additional stress for the latter. Experts call this process the discharge of blood “from left to right” (from the left half of the heart to the right).
- The right ventricle is “forced” to function more intensely in order to pump “extra” blood.
Changes in hemodynamics directly depend on the size and location of the defect. A small hole can close on its own (spontaneously) in a child by the age of 4-5 years. This usually happens in 65-75% of cases. With extensive defects, not only the right ventricle “suffers”. The pressure in the pulmonary circulation increases, and pulmonary hypertension occurs.
The baby’s body will try to compensate for the load:
- The mass of the ventricles increases.
- The walls of large and small arteries thicken.
- Thanks to these mechanisms, the pressure in both ventricles is equal. Despite the existing hole, blood discharge does not occur for some time.
- Gradually, the body's defenses are depleted, and the pressure in the right ventricle becomes greater than in the left.
- Venous blood will begin to flow through the defect into the systemic circulation - Eisenmenger syndrome. Decompensation of the defect occurs. Clinically, this process is manifested by the fact that the child begins to “turn blue.”
Fortunately, with early diagnosis and timely surgical treatment, this does not happen, even if the VSD is large. Therefore, try to listen to your doctor's advice. Of course, surgeons consider the best operation to be the one that the patient does not need to perform. But a ventricular septal defect in a newborn requires a thorough examination, specialist consultations, and a differentiated approach to patient management.
Classification of ventricular septal defects
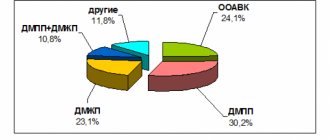
According to the International Classification of Diseases, 10th revision (ICD-10), any VSD is coded with a code – Q 21.0. However, in practical pediatrics, doctors distinguish four anatomical types of this anomaly, according to the “Clinical Guidelines for the Management of Children with Congenital Heart Defects,” approved by the Association of Cardiovascular Surgeons in 2013:
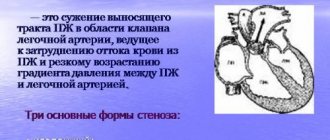
- Subarterial ventricular septal defect. Located directly below the pulmonary valve. The aortic leaf can “bend” or “wedge” into the existing hole, which causes aortic regurgitation (reverse discharge of blood).
- Perimembranous ventricular septal defect - the hole is located in the membranous part adjacent to the tricuspid valve. The membranous septum can fuse with the defect, partially covering it.
- Inflow ventricular septal defect is localized in the inflow portion of the right ventricle.
- A muscular defect of the interventricular septum can be located in the center of the muscle, in the upper part, or at the border between the wall of the right ventricle and the septum itself. Sometimes several small holes are detected at once (multiple type of muscular VSD - Tolochinov-Roget disease).
So that you are not frightened by medical terms, and it becomes clear where exactly the hole in the interventricular septum is in your child, I will try to explain further. Anatomists divide this structure into three parts - upper (membranous), middle (muscular), lower (trabecular). Consequently, the trabecular defect is located in the lower part, the muscular defect is located in the middle part, and the membranous defect of the interventricular septum is located in the upper part.
Classification of the disease
VSD in a newborn (can occur in older children) is defined as an independent disease or as part of a cardiovascular disease. The defect is classified primarily by size, which correlates with the aortic opening, thus there are the following:
- small vices. Their size does not exceed one centimeter, for example, this could be Tolochinov-Roger disease;
- great vices. Defined by sizes greater than one centimeter.
If we classify according to the location of the aortic opening, then there are several types of VSD.
Iron is necessary for the human body. It is an integral component of all cells and is also involved in many cellular processes. For example, iron (as part of the protein hemoglobin) transports oxygen from the lungs to all organs. Read more in the article: “iron supplements for anemia list.”
| Type of defect | a brief description of |
| Muscular | The hole is located directly in the muscle area. If small sizes are diagnosed, the pathology will resolve on its own |
| Membranous | The localization of the defect is in the upper part of the septum. Most often, the pathology is small in size, which spontaneously stops with the age of the child. |
| Nadgrebny | It is defined as the most serious heart defect, since the hole is localized at the border of the efferent vessels of the cardiac ventricles. It rarely resolves on its own |
It is necessary to diagnose the pathology in a timely manner in order to apply treatment if necessary and avoid possible consequences.
Doctor's advice
Repeatedly, parents tormented themselves and me, trying to find out the exact etiology of the child’s congenital defect. When such a diagnosis is discovered in your own child, you definitely want to find the culprit. Grandmother on my father’s side sometimes blames my daughter-in-law for “bad genetics,” and my mother’s relatives blame her son-in-law for smoking and drinking alcohol.
I strongly advise you not to do this. Of course, it is important to find out the reason in order to predict the birth of healthy or sick children from the parents and the child himself. A baby with a VSD will someday become a father or mother himself. But a little person’s illness is not a reason to sort things out. Forget family quarrels. Focus on taking care of the baby.
How to suspect a defect: symptoms and signs in a child
If the hole size is small, your baby will be no different from his peers. Probably, even in the maternity ward, the neonatologist will report that your baby has a systolic heart murmur. Parents usually ask with alarm at each auscultation: “Has the noise decreased or become stronger?” The paradox of VSD is that the intensity of the noise is inversely proportional to the size of the hole. The weaker the noise, the larger the size of the defect.
The situation is more serious if the baby was born “without noise”, but:
- from three to four weeks of age, he suddenly stopped gaining weight when the mother had enough milk;
- he developed shortness of breath during feeding;
- respiratory infections “pursue” him more often than other children;
- sometimes the child begins to “turn blue”;
- upon examination, the doctor suddenly discovers an expansion of the borders of the heart and an enlargement of the liver.
Subsequently, the clinical picture is characterized by a diffuse, intensified apical impulse, the appearance of systolic tremors on the left in the third and fourth intercostal spaces, expansion of the borders of the heart, especially to the left, and the formation of a cardiac hump (Davis chest).
When should you see a doctor?
Advertising:
VSD, despite the fact that it may not bother a small patient and may not manifest itself symptomatically, still requires mandatory monitoring by a specialist. A heart defect is a pathology in which a deterioration in the clinical picture can occur at any moment.
In order not to miss the moment when alarming symptoms arise, parents should constantly monitor the baby’s behavior and record atypical signs. It is worth going for a consultation with a cardiologist if:
- the child sleeps a lot of time;
- very capricious, without good reason;
- problems with weight gain are noted;
- lags behind in development.
The above signs are a reason to visit a pediatrician, and then, if necessary, a cardiologist.
Diagnostic methods
Auscultatory data and other symptoms will allow the pediatrician to suspect a congenital malformation in the child. Most likely, to clarify the diagnosis, the pediatric cardiologist will write a referral to:
- X-ray of the chest organs - if the defect is small, no changes will be detected. If the hole is of a significant size, hypertrophy of the left atrium and ventricle and an increase in the pattern of the lungs may be detected. In case of complication of VSD with pulmonary hypertension, bulging of the pulmonary artery arch with a weakening of the lung pattern and a non-hypertrophied left ventricle.
- Electrocardiography - in the differentiation of heart disease is not of particular importance, but will reveal a deviation of the electrical axis, as well as signs of overload of both or only the left ventricle.
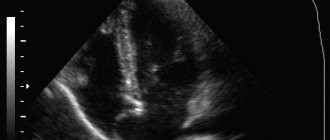
- Echocardiography is considered the main diagnostic technology for heart defects. The ultrasound examination method makes it possible to clarify the exact location of the hole, its size, the number of defects, and also evaluate changes in hemodynamics. The main purpose of ultrasound is to directly visualize the defect and exclude other cardiac anomalies. Doppler mapping will help determine the magnitude of the discharge, the presence of blood regurgitation, and assess the systolic pressure in the right ventricle.
If the defects are not clearly visible on echocardiography, or the doctor suspects a combined heart defect, you may need to undergo magnetic resonance or computed tomography.
Cardiac catheterization and angiography
Typically, these diagnostic techniques are rarely prescribed to children, but if non-invasive methods do not provide complete information about the condition, they are performed to assess hemodynamics in the pulmonary circulation and pulmonary hypertension. During this procedure, pressure in the aorta and pulmonary artery is measured, and the gas composition of the blood inside the heart chambers and large vessels is determined. Conducted by experienced specialists in regional centers.
Treatment of ventricular septal defect
The approach to the management of patients with VSD is strictly individual, depending on the size and location of the defect, clinical presentation (the occurrence of pulmonary hypertension, the development of circulatory failure), and the presence of concomitant pathology.
If the hole is small, there are no hemodynamic disturbances, the child only needs regular examinations by a cardiologist and periodic echocardiography. If there is the slightest doubt about the favorable course of the disease, surgical treatment is indicated.
There are the following types of surgical correction of VSD:
- An operation under artificial circulation, during which the cardiac surgeon sutures the hole or closes it with a valve.
- “Auxiliary” narrowing of the pulmonary artery is a preliminary surgical preparatory operation to prevent decompensation of the defect. Allows you to “buy time” before radical correction.
- Minimally invasive endovascular intervention. It is carried out under ultrasound and fluoroscopy control. Through the femoral artery, the vascular surgeon inserts a special device (spiral or occluder), passing it into the cavity of the heart, closing the defect.
- Hybrid operation. After opening the chest, an occluder is inserted directly through the myocardial puncture. The intervention protocol does not include stopping the heart and connecting it to the artificial circulation system.
A specialist decides which method is most suitable for your child. Without the written consent of the parents for surgical intervention, no doctor will operate on the child. It is important to discuss the progress of the operation with your doctor, choosing the most optimal tactics.
It should be remembered that if you miss precious time and do not close the hole before pulmonary hypertension develops, there is a risk of death from circulatory failure. Drug therapy is prescribed as preparation for surgery, during the rehabilitation period, as well as during the development of decompensation of the defect in order to support the functioning of the heart.
Case from practice
In the maternity ward, the neonatologist suspected congenital heart disease.
Ultrasound examination revealed a muscular defect of the interventricular septum in a newborn. Cardiocenter specialists recommended surgical correction before the age of 6 months, since the size of the hole was too large. The parents were determined to undergo surgical treatment, but according to their faith, the pastor's blessing was required. And he, seeing a seemingly healthy girl, advised to postpone the operation a little. Like, she’s still very little, the vice doesn’t bother her, you’ll always have time to “cut” it.
At the seventh month of life, the baby showed the first signs of pulmonary hypertension, which we tried unsuccessfully to combat by prescribing medications. On the ninth - the parents begged the heart surgeons to save the child, but it was too late to operate - a heart failure clinic developed. The girl died when she was one year old.
And yesterday a young man came to the reception. Eighteen years. He was indignant that the draft board doctors sent him to the hospital for additional examination. He is involved in athletics. He dreams of entering a military school. I open the outpatient card, and there is surgical treatment for VSD. On the chest there is a thin strip of postoperative scar, almost invisible. The guy doesn't remember the operation. He sincerely does not understand what is wrong with him. It’s just that his parents weren’t afraid to “cut” him at one time.
Complications
Advertising:
In extremely rare cases, a patent foramen ovale may be complicated by the development of paradoxical embolism. Emboli can become small gas bubbles, blood clots, or small fragments of fatty tissue. When the foramen ovale is open, they can enter the left atrium, then into the left ventricle. With the blood flow, the embolus can enter the vessels of the brain and cause the development of a cerebral infarction or stroke: conditions that can be fatal. This complication appears suddenly and can be provoked by injury or prolonged bed rest during periods of serious illness.
Complaints of abdominal pain are diagnosed at least once during childhood in every child, and cause great concern among his parents. In each such case, you need to consult a pediatrician, pediatric gastroenterologist, or surgeon as quickly as possible. Read more in the article: “The child’s right side hurts.”
In most cases, an open foramen ovale in newborns and children under two years of age does not cause serious complications and does not bother the child. In most children, it completely heals by the age of five and does not in any way affect further physical and social activities. For patients with a patent foramen ovale without serious hemodynamic disturbances, cardiologists recommend excluding extreme sports and choosing professions that are associated with excessive stress on the respiratory and cardiovascular systems (divers, pilots, astronauts).
Is it possible to diagnose a defect before the birth of a child?
Yes, you can. To do this, it is necessary to undergo a timely ultrasound examination during pregnancy by an experienced specialist using modern equipment. If your unborn baby is suspected of having a VSD, try to choose a maternity hospital closer to the cardiac center.
We often hear reproaches from parents that they followed all the doctors’ recommendations, but the heart defect was discovered only after the birth of the child. Unfortunately, a hole in the interventricular septum with a diameter of up to 4 mm is very difficult to detect without color Doppler mapping. Therefore, if you have a family history, smoked before pregnancy, or had the flu or acute respiratory viral infection when you were expecting a baby, be sure to tell your gynecologist about this. You may need to undergo additional ultrasound using more sensitive equipment.
Risk factors and main causes
It is typical that a heart defect forms in the fetus in the early weeks of pregnancy (from the 3rd to the 10th week of pregnancy). The development of this pathological process is explained by a combination of certain factors and causes:
- Genetic predisposition.
- If the mother suffered from various infectious diseases (measles, flu) during pregnancy.
- The presence of bad habits (the mother's consumption of alcoholic beverages, smoking, ends in the development of defects in the fetus).
- Teratogenic effects due to taking antidepressants and other psychotropic drugs, antibiotics.
- Consequences of exposure to heavy metals and radiation exposure on the female body during pregnancy.
- Regular stressful situations.
If a woman leads an unhealthy lifestyle during pregnancy and takes various potent drugs, then the child may be diagnosed with heart defects after birth, one of the most common being VSD.