This information explains how to relieve shortness of breath.
Sometimes you may find it difficult to breathe and feel like you are out of breath. This condition is called shortness of breath or dyspnea. Shortness of breath may be caused by:
- damage to the lungs due to cancer or its treatment;
- blood clots in the lungs (pulmonary embolism);
- fluid around the heart or lungs;
- pneumonia (pneumonia);
- asthma or emphysema;
- heart damage (chronic heart failure);
- anemia (low levels of red blood cells in the body).
Depending on the cause, shortness of breath may be transient or permanent.
to come back to the beginning
Relief of shortness of breath
The best way to relieve shortness of breath is to treat the cause. But this is not always possible. Your doctor and nurse will work with you to determine the best ways to improve your breathing. Below are other ways to relieve symptoms.
General Tips
- Try using a small hand-held fan to blow air on your face when you feel out of breath. This is a way to provide immediate relief from shortness of breath.
- When carrying out daily activities, limit your activity so as not to cause discomfort. If you are out of breath, stop and rest until your breathing is the same as when you started your activity. After that, get back to what you're doing if you can.
Oxygen
Every cell in your body needs oxygen. If your blood oxygen levels are low, you may experience shortness of breath. Your doctor or nurse can measure the oxygen levels in your blood using a small finger-worn device called an oximeter.
If you don't have enough oxygen in your blood, breathing in extra oxygen can help make you feel better. You can get extra oxygen in two ways:
- Using a hub. A concentrator is a small machine that takes oxygen from the air and delivers it to you through a thin, flexible tube placed under your nose.
- From a portable oxygen cylinder. You can take this cylinder with you anywhere. If the oxygen in the cylinder runs out, it can be refilled. Companies that provide breathing machines or home care services can deliver oxygen to your home if needed.
Medicines
Your doctor may also prescribe medications for shortness of breath, depending on the cause. You may take these medications by inhalation, orally (by mouth), or intravenously (through a vein).
- If you have asthma, emphysema, or chronic bronchitis, your doctor may prescribe a nebulizer or inhaler. Both devices spray the medication into tiny droplets that you inhale. Your nurse will teach you how to use a nebulizer or inhaler.
- If you have a blood clot in your lung, your doctor may prescribe a blood thinner (anticoagulant). This medicine may be taken as a tablet or as an injection (shot). Your doctor will order blood tests and tell you what precautions you need to take while taking these medications.
- If you have pneumonia, your doctor may prescribe antibiotics to treat it.
- If you have too much fluid around your heart or in your lungs, your doctor may prescribe medications such as diuretics (water pills) or diuretic injections to get rid of the fluid.
Other medications that may help make breathing easier include:
- corticosteroids, such as prednisone (Deltasone®) or methylprednisolone (Medrol®);
- pain medications such as morphine sulfate (Avinza® or Kadian®).
Your doctor will discuss with you which of these medications is best for you.
to come back to the beginning
Drugs
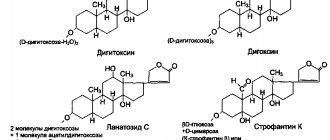
Digoxin belongs to the group of cardiac glycosides. It reduces the heart rate caused by arrhythmia, thus making the heart work easier and increasing its tolerance to exercise. However, the drug tends to accumulate in the body, so it is not prescribed for a long time.
Carvedilol is a drug from the group of beta blockers. It, like the glycoside described above, helps reduce the heart rate, in addition, reduces oxygen starvation of the muscle, blood pressure, and removes excess fluid from the body.
"Monopril" is an inhibitor. It dilates the arteries, promotes easy passage of blood through them, as well as immediate delivery of oxygen to all organs.
Lasix is one of the diuretic drugs. Removes excess fluid from the body, which becomes one of the causes of shortness of breath. Along with it, the body actively leaves potassium. Therefore, you need to carefully monitor its constant replenishment in the form of products (baked potatoes, bananas). Read more about how to get rid of the manifestations of heart failure here https://cardiograf.com/bolezni/dekompensatsiya/serdechnaya-nedostatochnost-lekarstva.html
Breathing exercises
Your nurse can show you how to take slow, deep breaths to help relieve shortness of breath. You can do them with the diaphragm, the muscle that separates the chest cavity from the abdominal cavity (see Figure 1). This type of breathing is called diaphragmatic breathing.
Figure 1. Aperture
Try to relax while doing breathing exercises. Relieve muscle tension. This will allow the abdominal cavity (belly), chest, and lungs to expand.
Here are some breathing exercises that can help relieve shortness of breath.
Deep breathing 4-8-8
This exercise improves the movement of air in the lungs. This helps increase oxygen levels throughout the body.
- Inhale through your nose, counting to 4.
- Hold your breath and count to 8.
- Exhale through pursed lips (as if you were whistling) for a count of 8.
- Repeat 4 times.
Chest wall stretch
This exercise will help the chest muscles become more elastic.
- Inhale through your nose, counting to 4. As you inhale, extend your arms in front of you and raise them above your head.
- Exhale through pursed lips. As you exhale, open your palms and lower your arms down to your sides.
- Repeat 4 times.
Rapid breathing through the nose
This exercise can help strengthen your diaphragm.
- Shut your mouth.
- Inhale and exhale quickly through your nose for 15 to 30 seconds.
- Practice this exercise several times until you can do it for 60 seconds.
Walking and breathing
These tips will help you breathe easier when walking.
- When walking on a level surface, inhale and exhale through your nose without opening your mouth.
- On inclined surfaces (slopes), inhale through your nose and exhale through pursed lips.
- When climbing stairs, exhale at each step through pursed lips.
Recovery from an attack of shortness of breath (from coughing or exercise)
- Tuck your chin to your chest.
- Take 10 short and sharp exhalations through your mouth. If necessary, take short breaths between them.
- When your neck muscles relax a little, inhale through your nose.
- Exhale 3 times through pursed lips. Inhale between exhalations.
- Inhale through your nose, counting to 4.
- Exhale through your open mouth, counting to 8 and making the sound “ah”.
- Repeat 3 times.
to come back to the beginning
How to get rid of shortness of breath?
Over time, the symptoms of a cardiac disorder worsen, and shortness of breath increases. The reason for this is the patient’s reluctance to scrupulously and clearly follow the doctor’s recommendations. You should not take independent measures; drug treatment can only be prescribed by a qualified specialist.
To determine the causes of respiratory disorders, the patient is prescribed an examination:
- R-graphy of the chest;
- biochemical blood test;
- ECG;
- external respiration function analysis;
- Ultrasound of the heart.
People suffering from shortness of breath of cardiac origin are prescribed medications from one or more groups:
| Medicinal group of the drug | Action and direction of the drug |
| Angiotensin-converting enzyme inhibitors | Vasodilation and lowering blood pressure. Facilitate blood pumping. Reducing the severity of heart disorders. |
| Beta blockers | Improved heart function. Slowing contraction frequency, reducing oxygen demand. |
| Diuretics | Improving the removal of excess fluid from the entire body. |
| Aldosterone antagonists | The action is similar to diuretic drugs. Reduces the occurrence of scar tissue of the heart muscle. |
| Nitrates and hydralazine | Dilatation of blood vessels. |
| Digoxin | An increase in the strength of heart contractions and a decrease in their frequency. Prescribed to patients with heart failure and atrial fibrillation. |
To reduce such manifestations, it is important to adhere to some recommendations for a healthy lifestyle:
- Carefully follow all specialist prescriptions aimed at treating the underlying disease.
- Quit smoking. Smoking not only damages the lungs, but also blood vessels, reduces the amount of oxygen in the blood, which leads to increased blood pressure and increased heart rate. Such changes significantly worsen shortness of breath.
- Reduce your weight and maintain it at a healthy level.
- Do moderate physical activity every day. After discussing with a specialist a rehabilitation program for a cardiac disorder, this factor must be taken into account.
- Avoid stressful situations, as they can aggravate the disease. Meditation and yoga classes will help you learn to control your stress levels.
- Do not rise higher than 1500 meters from sea level.
When treating this condition, doctors usually prescribe a Mediterranean diet to their patients. It is rich in vegetables, fruits, whole grains, vegetable oils, low-fat dairy products and moderate amounts of seafood and fish. Foods high in cholesterol and trans fats should be avoided or at least significantly reduced in consumption.
It is necessary to significantly reduce the consumption of table salt, which contributes to fluid retention. Alcohol also has a negative effect on a person’s health, since it leads to weakening of the heart muscle, and when interacting with medications, it provokes the development of arrhythmia. In case of severe deficiency, which is accompanied by a significant excess of fluid, experts recommend limiting water intake.
You need to carefully monitor symptoms and lead a calm, healthy lifestyle during recovery. It is necessary to stop being lazy and start working on yourself, taking manifestations of violations seriously. Since there are many reasons why a person develops shortness of breath, treatment must be comprehensive - only in this way can one count on a speedy recovery.
Also, to improve ventilation of the lungs and better enrich the blood with oxygen, you can perform simple breathing exercises:
- Having exhaled all the air through your mouth, you need to inhale it through your nose, then exhale sharply through your mouth and suck in your stomach for ten seconds. Then inhale the air “with your stomach” through your mouth and, drawing in your stomach, hold your breath for another ten seconds. This exercise is performed in any comfortable position, even while walking or working in an office chair.
If you notice symptoms of difficulty breathing, it is important to understand that this is only a sign of some kind of ailment.
You should immediately call an ambulance if:
- the occurrence of strong wheezing, which can be heard even at a distance;
- cough with pink sputum of foamy consistency;
- bluish skin;
- the occurrence of cold, profuse sweat;
- extremely difficult to feel pulse;
- a strong decrease in pressure to 90/60 mmHg;
- inability to breathe while lying down.
Before the doctor arrives, take the following measures:
- open a window or vent to ensure fresh air enters the room;
- unfasten the buttons of the collar area to supply oxygen to the body and ensure good ventilation of the lungs;
- help a person take a comfortable semi-sitting or sitting position, while the legs must be lowered down in order to free the heart from unnecessary stress, creating an outflow of blood to the lower extremities;
- use an oxygen cushion, if available;
- Place a Nitroglycerin tablet under your tongue.
Relief from anxiety
Shortness of breath can cause feelings of fear. Some people say they feel anxious when they start to feel short of breath. However, anxiety can make breathing even more difficult.
Breathing exercises from this material can help you relax. You may also want to know other ways to help relieve anxiety. Talk to your doctor about any anxiety you have. He may prescribe anti-anxiety medications such as alprazolam (Xanax®) or lorazepam (Ativan®) to help you.
Our Integrative Medicine Service also offers relaxation programs that may be beneficial for you.
to come back to the beginning
1. Treatment of heart failure, medications used for treatment
Today there are many more treatments for heart failure than in the past.
Primary treatment for heart failure usually involves taking medications regularly, maintaining a healthy lifestyle, and closely monitoring your condition. If the disease progresses, the patient may require surgical treatment of heart failure.
What medications are used to treat congestive heart failure?
Strict adherence to the schedule and dosage of medications recommended by your doctor is an important condition for maintaining your own health. Most often prescribed for the treatment of heart failure:
- Angiotensin-converting enzymes (ACE);
- Angiotensin II receptor blockers (ARBs);
- Beta blockers;
- Digoxin;
- Diuretics;
- Blood vessel dilators;
- Potassium or magnesium;
- Calcium channel blockers;
- Medicines to support heart function.
A must read! Help with treatment and hospitalization!
Symptoms
Precursors of an attack of cardiac asthma can be: shortness of breath, tightness in the chest, coughing during slight physical activity or moving to a horizontal position that has appeared in the previous 2-3 days. Attacks of cardiac asthma are more often observed at night, during sleep, due to a weakening of adrenergic regulation and an increase in blood flow into the pulmonary circulation system in the supine position. During the daytime, an attack of cardiac asthma is usually associated with physical or neuropsychic stress. Typically, attacks of cardiac asthma occur suddenly, causing the patient to wake up from a feeling of acute lack of air and increasing shortness of breath, turning into suffocation and accompanied by a hacking dry cough (later with a small separation of clear sputum). During an attack of cardiac asthma, it is difficult for the patient to lie down; he takes a forced vertical position: stands up or sits down in bed with his legs down (orthopnea); usually breathes through his mouth, speaks with difficulty. The state of a patient with cardiac asthma is excited, restless, accompanied by a feeling of panicky fear of death. On examination, cyanosis is observed in the area of the nasolabial triangle and nail phalanges, tachycardia, and increased diastolic blood pressure. On auscultation, dry or scanty small bubbling rales may be noted, mainly in the lower parts of the lungs. With a prolonged and severe attack of cardiac ascyanosis, cold sweat, swelling of the neck veins; the pulse becomes threadlike, blood pressure drops, and the patient feels a sharp loss of strength. The transformation of cardiac asthma into alveolar pulmonary edema can occur suddenly or as the severity of the disease increases, as evidenced by the appearance of copious frothy sputum mixed with blood, moist small- and medium-bubble rales over the entire surface of the lungs, and severe orthopnea.