A healthy person does not feel the work of his heart in any way. And if heart rhythm disturbances occur, he may feel palpitations, interruptions or “loss of pulse.” The normal heart rate of an adult is from 60 to 90 beats per minute.
Tachycardia is an increase in heart rate to values exceeding 90 beats per minute. Often in such situations, patients complain of increased beating, “fluttering” or “jumping out” of the heart, they say that “the heart is pounding.” Of course, such a condition is a deviation from the norm.
Causes of tachycardia:
Heart diseases
Diseases of the heart and blood vessels that can provoke tachycardia include:
- heart failure;
- coronary heart disease, myocardial infarction;
- aortic insufficiency;
- abnormalities of the cardiac conduction pathways;
- heart rhythm disturbances;
- arterial hypertension.
Other (non-cardiac) causes of tachycardia
:
- respiratory failure, emphysema;
- obesity;
- binge eating;
- alcohol abuse;
- excessive consumption of strong coffee, tea;
- use of narcotic and psychotropic drugs;
- diabetes;
- increased thyroid function;
- pheochromocytoma;
- vegetative-vascular dystonia;
- panic attacks.
Associated symptoms
Tachycardia may be accompanied by:
- nausea;
- cold sweat;
- dizziness;
- shortness of breath;
- pain in the chest, a feeling of squeezing;
- weakness;
- loss of consciousness;
- frequent yawning;
- anxiety, etc.
Tachycardia in heart disease
described in the sections on heart failure, myocardial infarction, aortic insufficiency, cardiac rhythm and conduction disorders, and arterial hypertension.
Other causes of tachycardia are briefly listed below.
Tachycardia and diabetes mellitus
Tachycardia is one of the manifestations of decompensation of diabetes mellitus. Disturbances in the nervous regulation of the heart often lead to increased heart rate, which is difficult to treat.
Tachycardia in diseases of the stomach
In some cases, tachycardia after eating is caused by the so-called gastrocardial syndrome. It is characterized by the fact that spicy or fatty foods lead to exacerbation of stomach pathologies, manifested by pain in the abdominal cavity, combined with an increase in heart rate.
But in itself, an increase in heart rate after eating is not a heart disease, but a symptom that should alert the patient and force him to seek advice from a cardiologist and gastroenterologist.
Tachycardia, sweating and weakness - a triad characteristic of the so-called. dumping syndrome, a condition that occurs after gastric resection surgery. In this case, food from the reduced stomach quickly enters the small intestine and causes the above sensations.
Tachycardia after eating
In overweight people, fat deposits appear not only in the subcutaneous layer, but also on the membranes of internal organs, over time increasingly limiting their natural mobility. In such situations, after a heavy meal, a full stomach puts pressure on the diaphragm, which provokes increased breathing and, as a result, an increase in heart rate.
We must not forget that the processes of digestion and assimilation of eaten food are a serious burden for the body, which requires increased energy consumption. To do this, the heart is forced to increase its contraction rate to ensure sufficient blood flow to the stomach, intestines and digestive glands. And if you are overweight, this task is complicated by large amounts of adipose tissue.
Tachycardia in pathology of the nervous system
An increase in heart rate is also typical for people with psycho-emotional disorders, which can serve as one of the manifestations of a neurotic state. In this situation, the patient just needs to calm down - and then the heart rate will quickly return to normal.
Tachycardia in diseases of the thyroid gland
Increased activity of the thyroid gland (thyrotoxicosis) leads to sustained tachycardia. This occurs with inflammatory diseases of this endocrine organ, as well as the appearance of hormonally active formations (nodes).
University
→ Home → University → University in the media → A cold is not as terrible as its consequences
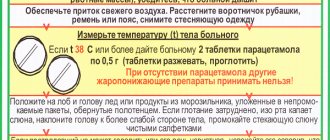
The incidence of acute respiratory tract infections is increasing worldwide. This is due to increasing environmental pollution, irrational use of antibiotics, household allergies, smoking, deterioration of the immune system, and unfavorable social factors. Against this background, pulmonologists note with regret the increase in the number of chronic diseases, mainly pneumonia and bronchitis. Most often they occur after repeated respiratory infections, especially when patients, feeling better, voluntarily stop treatment. ARVI is perhaps the most common diagnosis of the autumn-winter season. Maybe that's why he is perceived as absolutely 'not scary'. A person suffers from a so-called cold on his legs over and over again, but once again he is surprised: where did he get bronchitis or pneumonia from? It seemed like he was doing everything as always: aspirin, something for a cough... About 200 varieties of viruses are known that cause ARVI - acute respiratory (respiratory tract) viral infections. What they all have in common is that they are transmitted by airborne droplets, have the same symptoms, and are not treated with antibiotics. The most famous of them is the influenza virus. The symptoms of ARVI are familiar to everyone: fever, runny nose, dry cough, headache, general weakness. Actually, the treatment of ARVI consists of the treatment of these manifestations. Temperature requires special attention. It is an indicator that the body is fighting infection. It is the increase in temperature during ARVI that helps kill the causative agent of the disease. In this condition, a person should remain in bed (under no circumstances try to “overcome” a cold on the legs), drink more - drinking plenty of fluids helps remove toxins from the body that are formed during illness. People handle heat differently. More often, in order to minimize the discomfort associated with fever, they try to fight it - this is not at all difficult, because there are dozens of antipyretic drugs in pharmacies. Their use 'blurs' the clinical picture of the disease. The biological significance of fever is the activation of the body's immune (defense) reactions. Increased body temperature prevents the proliferation of viruses. But if you have a fever for more than three days and your temperature is 38°C or higher, then this is a serious sign that bacterial complications have joined ARVI (acute sinusitis, otitis media, bronchitis, pneumonia). And they require other treatment, including antibiotics. If the temperature is artificially reduced with medications, diagnosis and treatment may be delayed. All of the above applies to adults; in children, approaches to diagnosis and treatment are somewhat more complicated. You need to see a therapist. He will prescribe treatment, if necessary, additional examination, and refer you to a specialist. Every year, after the winter flu epidemic, new and new legions are added to the army of constantly coughing people. The production of a small amount of sputum and a slight cough are usually of little concern. Many people quickly get used to them and consider them to mean nothing. But coughing and sputum production are signs that allow one to suspect trouble, and more often these are symptoms of bronchitis (possibly already chronic) or pneumonia. These diseases also involve the cardiovascular system in the process - the so-called cor pulmonale is formed. About 7% of the adult population suffers from chronic lung diseases. Chronic cor pulmonale develops in approximately 3% of these patients, and in the overall structure of mortality from congestive heart failure, chronic cor pulmonale accounts for 30% of cases. The disease called cor pulmonale is very insidious; it may not manifest itself with special symptoms until a certain time. That is why timely diagnosis is a decisive factor in curing the patient. Pulmonary heart is a condition of overload and hypertrophy of the walls of the right ventricle of the heart as a result of increased pressure in the pulmonary circulation. Chronic cor pulmonale can develop over many years. I give the floor to a colleague who is competent in this problem. Pulmonary heart Diseases of the bronchi and lungs have a significant impact on the state of the cardiovascular system. Damage to the heart and a complex of circulatory disorders caused by a disorder of the bronchopulmonary system are called cor pulmonale. This condition develops as a result of about seventy diseases: most often (80% of cases) - diseases of the bronchi and lungs (chronic obstructive pulmonary disease, pneumoconiosis, sarcoidosis, tuberculosis, etc.); rarely - diseases affecting the chest and diaphragm (curvature of the spine, multiple injuries to the ribs with limited mobility of the chest, Pickwick syndrome in obesity, pleurisy); sometimes - as a result of primary damage to the pulmonary vessels (primary pulmonary hypertension, recurrent thromboembolism of the branches of the pulmonary artery, etc.). The main mechanism for the development of cor pulmonale is considered to be an increase in pressure in the arterial vessels of the pulmonary circulation and pulmonary artery (pulmonary hypertension). Impaired blood oxygen saturation causes a narrowing of the blood vessels in the lungs, their restructuring and insufficient blood supply to the tissues (tissue hypoxia). In addition to changes in blood vessels and lung tissue, the volume of circulating blood increases, the number of blood cells increases, and its viscosity increases. Against the background of the development of respiratory failure, changes occur in the right ventricle of the heart: metabolic disorders occur in the heart muscle, then its hypertrophy (increase in mass). The right chambers of the heart, experiencing increased stress when pushing blood into the pulmonary artery, expand, their contractility decreases - heart failure develops. If signs of heart failure appear suddenly, within a few hours, the development of cor pulmonale is called acute; within a few weeks - subacute; for several months, years - chronic. Chronic cor pulmonale develops almost imperceptibly over many years, without obvious clinical signs of circulatory failure. Anyone who has diseases of the bronchi and lungs must undergo examinations to identify signs of chronic pulmonary heart disease. ECG and X-ray methods reveal signs of hyperfunction and/or hypertrophy of the right ventricle. An informative method for measuring pressure in the pulmonary artery and assessing the condition of the heart muscle is echocardiography. With decompensated cor pulmonale, a person may feel pain in the heart area, in the right hypochondrium, swelling appears in the legs and/or feet, and the nature of shortness of breath changes. A common sign of cor pulmonale is rhythm disturbances: palpitations (tachycardia), irregular contractions. Undoubtedly, treatment of chronic pulmonary heart disease must begin as early as possible - with measures to prevent exacerbations of bronchopulmonary infection. It is very important to quit smoking (active and passive!). It is necessary to avoid hypothermia and prevent acute respiratory diseases. In case of heart failure, it is necessary to limit physical activity and follow a diet with limited salt and liquid. In the treatment of pulmonary heart disease, medications are used that improve blood circulation, normalize metabolic disorders, restore the structure of the heart and blood vessels, and lower blood pressure (systemic and in the pulmonary artery). If indicated, diuretics are added, using them with caution to prevent a significant decrease in the volume of circulating blood and its thickening. Other drugs are prescribed according to indications (cardiac glycosides, prostaglandins, vasodilators, etc.). Hypoxemia and hypoxia (low oxygen content in the blood and, as a result, in the tissues of the body), as a rule, lead to an imbalance of magnesium and potassium in the body. The use of diuretics and cardiac glycosides aggravates the deficiency of these vital ions and causes a deterioration in metabolic processes in the myocardium, as well as cardiac arrhythmias. The administration of drugs containing potassium and magnesium (panangin) helps improve myocardial metabolism and normalize heart rhythm. In the treatment of respiratory failure in cor pulmonale, the use of oxygen therapy is of great importance. Evgenia Trisvetova, Doctor of Medical Sciences, Professor of the 2nd Department of Internal Diseases of the Belarusian State Medical University Rule for everyone: self-medication for the flu is unacceptable, all medications must be prescribed by a doctor This attitude may raise doubts, especially in conditions of a full-blown epidemic, when clinic doctors have terrible time pressure. But it is difficult to predict the course of the flu, and complications can be varied, including life-threatening and developing at lightning speed. This danger distinguishes influenza from other acute respiratory diseases. We will try to outline the reasonable actions of a person sick with influenza or ARVI before the first visit to the local doctor. When the first symptoms occur, it is recommended: 1. Drink plenty of fluids - tea with lemon, cranberry or lingonberry juice, alkaline mineral waters (Borjomi with milk, etc.); However, it should be remembered that excessive fluid intake is contraindicated in patients with chronic heart failure. 2. For high hyperthermia (above 38°) - antipyretics: paracetamol, ibuprofen in an age-appropriate dosage; aspirin - only for adults. 3. To facilitate nasal breathing - vasoconstrictors. It is necessary to remember about the development of atrophy of the nasal mucosa with their long-term use and the contraindication of these drugs for hypertension. Vasoconstrictors reduce swelling of the mucous membrane and improve the outflow of mucus from the paranasal sinuses, which prevents the development of sinusitis. Take seriously the advice on how to blow your nose correctly: clear each nostril in turn, while pressing the other with your thumb to the nasal septum. This must be done every time before putting drops into your nose. You can’t “sniff”: the viruses and inflammatory products contained in the nasal secretions enter the body, increasing intoxication. 4. Means for thinning and removing sputum (mucaltin, licorice root, marshmallow tincture, bromhexine, etc.). 5. If the cough is very strong, dry, painful, and prevents you from sleeping, use antitussives (mainly in pediatric practice). 6. Children over 2 years of age and adults in the first days of illness benefit from steam inhalations with infusions of chamomile, calendula, mint, sage, St. John's wort, pine buds, and a 1-2% soda solution (wait with this at high temperatures). 7. Taking ascorbic acid and multivitamins. All this is used to alleviate the typical symptoms of influenza and ARVI and does not affect the reproduction of the pathogen. The development of any complications of influenza requires emergency hospitalization and intensive treatment. Antibacterial drugs are prescribed only by a doctor in the presence of complications, as well as in the presence of chronic foci of infection (chronic sinusitis, pyelonephritis, etc.). According to one study conducted in Russia, three-quarters of surveyed primary care physicians were willing to use antibiotics in adults for influenza, starting from the first days of the disease. They considered the purpose of the prescription to be to prevent the occurrence of bacterial complications. But responsibility for the erroneous prescription of antibiotics that do not affect viruses should not be placed solely on the doctor. Most of the respondents pointed to pressure from the patient or his relatives, who believe that taking antibiotics is mandatory for fever. Question and answer I’m already used to coughing in the morning - I’ve been smoking for a long time. Recently, when walking fast, shortness of breath and stabbing pain in the heart appear. If you quit smoking, will it help you feel good again? (I.P. MOROZOV) - Undoubtedly, smoking aggravates your condition and you need to get rid of your addiction. Shortness of breath and pain in the heart area can occur with many heart diseases. However, a long history of pulmonary disease (smoking and coughing) indicates the possible development of cor pulmonale. You need to see a doctor. I have had a curvature of the spine since childhood. From the doctor I heard that my heart is “pulmonary”. However, I don’t smoke, I haven’t suffered from serious lung diseases... (Nina EGOROVA) - 'Cor pulmonale' is a collective concept that is used to characterize changes (structural and functional) that occur in the vascular bed of the pulmonary circulation and in the heart. These disorders can develop due to curvature of the spinal column. Are there early signs of heart damage in lung diseases? (TRIFONOVA Galina Sergeevna) - Unfortunately, subjective signs indicating dysfunction of the cardiovascular system appear at a later date. At the same time, it is known that prevention of exacerbations of bronchopulmonary infections, timely treatment of lung diseases and the use of medications that improve blood circulation in the pulmonary circulation, as well as normalize metabolic processes in the heart muscle, lengthen the period of normal heart activity. In my childhood I suffered from pulmonary tuberculosis. I undergo annual examinations; there have been no signs of process activity for many years. However, shortness of breath, enlarged liver, and swelling in the legs appeared. Doctors believe that the cause is heart damage due to a long-standing tuberculosis process in the lungs. Is this really possible after so many years of prosperity? (Igor KOROTCHENYA) - In the case of a widespread sclerotic process in the pulmonary tissue as a result of an infectious or non-infectious lung disease, circulatory disorders occur in the pulmonary circle and a pulmonary heart can form. The process of formation of chronic pulmonary heart lasts for years. I suffered from pneumonia several times as a child. Now (I am a 2nd year student) I have been diagnosed with bronchial asthma. I passed the winter session well, but was ill for two weeks: I was coughing, short of breath, and had pain in my heart. In addition to asthma medications, the doctor advised me to take potassium and magnesium supplements to improve metabolic processes in the heart. Is taking heart medications justified? (Maria Selkhanovich) - With bronchial asthma, attacks of bronchial obstruction occur, which lead to changes in the gas composition of the blood and metabolic disorders in the tissues of many organs. The use of drugs including magnesium and potassium has a normalizing effect on metabolic processes in the myocardium. In addition, since a tendency to bronchospasm can occur if the magnesium content in the body’s cells is reduced, potassium and magnesium supplements have a positive effect by reducing the reactivity of the bronchi.
doctor Alexander Nefagin Vecherniy Minsk , February 1, 2008
Share
Treatment of tachycardia
In the case when tachycardia occurs once and quickly stops on its own, this should not be a cause for concern. But if this symptom appears constantly, then you need to consult a cardiologist. It should be remembered that tachycardia can be a symptom of both a functional disorder of the nervous system and a serious heart disease.
Depending on the indications, cardiologists at the CELT clinic conduct examinations to identify the cause of the patient’s tachycardia:
- ECG;
- Holter ECG monitoring;
- Stress test;
- Transesophageal ECG and atrial stimulation;
- EchoCG;
- Study of sugar metabolism disorders;
- Tests for the activity of thyroid hormones.
Having determined the cause of the increased heart rate, the doctor will be able to choose the optimal treatment regimen for the underlying disease.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions