Full text of the article:
Diabetes mellitus, or “sugar,” affects people of all ages. We have learned to live with this diagnosis and identify it in the early stages. However, the likelihood of early diagnosis of the disease is possible only with regular preventive examinations by a doctor. To begin with, we suggest you understand what diabetes mellitus can be.
The essence of type 2 diabetes
The main difference between type 2 diabetes is the immunity of body cells to the action of the hormone insulin, i.e. their insulin resistance. In a healthy person, insulin “instructs” the cell membranes of various tissues to “let in” glucose, the main source of energy. In a patient with type 2 diabetes, the cells do not perceive the “commands” of insulin, and the membrane remains “locked.”
In patients with type 2 diabetes, insulin cannot open the glucose lock
As a result:
- The tissues of various organs do not receive the energy necessary to perform their functions normally.
- The glucose content in the blood exceeds the norm (hyperglycemia occurs), which most unfavorably affects the ability of the main fluid of our body to transport oxygen from the lungs to the tissues, and carbon dioxide from the tissues to the lungs.
- The liver, which normally always stores a “strategic reserve” of glucose, responds to “requests for help” from starving cells of skeletal muscles, brain, heart, etc. And releases the “stored” sugar into the blood, further increasing its content in it.
- The insulin-producing “islands” in the pancreas work “overtime” in response to high blood sugar. Over time, this leads to their depletion and loss of their secretory functions.
T1DM
There are two types of diabetes mellitus. Type 1 diabetes mellitus (T1DM) develops at a young age. The cause of the disease is an absolute lack of insulin in the body, which occurs due to the destruction of beta cells of the pancreas. Type 1 diabetes mellitus most often appears after treatment of an infectious disease or severe stress. The patient experiences severe thirst, increased urination, weakness, and weight loss. The disease progresses rapidly and may be accompanied by loss of consciousness. The patient needs medical care in a hospital.
Causes of type 2 diabetes
The exact causes of insulin resistance are not yet known, but the risk factors for type 2 diabetes have been well studied. The likelihood of disease increases:
- Hereditary predisposition.
A poor family history is a cause for concern. The tendency to hyperglycemia in children and grandchildren of diabetics is confirmed by long-term statistics. If one of your close relatives is sick or has had diabetes, you need to take this circumstance into account and try to minimize the effect of external factors that can trigger the onset of the disease. - Infectious diseases, hormonal and metabolic disorders.
A connection has been identified between hepatitis, polycystic ovary syndrome, hypertension, increased levels of glucocorticosteroids, excess “bad” cholesterol and the development of insulin resistance. - Diabetes in pregnant women (gestational).
All pregnant women must undergo a blood sugar test. This should not be considered the whim of a gynecologist or therapist. During pregnancy, a woman may experience disturbances in carbohydrate metabolism, which disappear after childbirth without any treatment. Hyperglycemia complicates the course of pregnancy, so expectant mothers with high sugar levels must adhere to a special diet. And although after childbirth, blood glucose levels usually normalize, you need to remember that a history of gestational diabetes is one of the risk factors for developing type 2 diabetes during menopause.
Pregnant women must have their blood sugar checked
- Poor nutrition.
Fast food, semi-finished products and ready-made products with a large amount of “fast” carbohydrates, i.e. almost instantly converted into glucose and absorbed from the intestines into the blood, today they prevail in our diet. Danger lurks even in those products that are positioned as healthy. For example, extrusion processing of oatmeal significantly increases the amount of sugar and broken down starch in Hercules flakes, so their glycemic index is not much lower than that of French fries. - Obesity
– The risk of diabetes is directly proportional to your body mass index. The greater the degree of obesity, the more likely it is to disrupt the hormonal regulation of glucose metabolism. The most dangerous are fat deposits of the android type, that is, in the abdomen and upper body, as well as fat accumulations inside the abdominal cavity (visceral fat). - Stress.
Back in the 19th century, during troubled times of economic crises, type 2 diabetes was aptly named “stockbrokers’ disease.” It was noticed that stockbrokers who risk a lot of money every day, as well as other people whose line of work was associated with constant stress, very often developed diabetes. - Intermittent, shallow night sleep with insufficient ventilation of the lungs
is another reason for impaired glucose metabolism and the onset of type 2 diabetes. Therefore, it is so important to know and follow the rules of healthy sleep. - Insufficient physical activity.
Modern man lives at high speeds. To be on time everywhere, we use a personal car, taxi, and public transport. For a successful career, we sit in front of computer screens for 10-12 hours. Fortunately, lately morning jogging and cycling, swimming and working out in the gym have become fashionable mainstream. Unfortunately, not everyone understands their importance and makes it a part of their life. In the absence of physical activity, metabolic disorders overtake a person at a much earlier age - this is also why non-insulin-dependent diabetes becomes “younger”.
Sedentary work and constant overwork provoke the development of type 2 diabetes
- Important! The combination of the above factors further increases the risk of type 2 diabetes. And the presence of the disease, in turn:
- reduces the tolerance of the cardiovascular system to stress and physical activity;
- reduces muscle tone and endurance;
- disrupts nighttime sleep and metabolism, turning the normal desire to lose weight into an almost impossible task.
Prevention
To prevent the development of diabetes, you must:
- normalize body weight;
- constantly practice moderate physical activity, play sports, walk in the fresh air;
- switch to a healthy diet, which involves eating plenty of fruits and vegetables;
- promptly treat pancreatic diseases.
People with obesity, frequent stress, and poor diet need to be especially careful. Diabetes mellitus is also possible during pregnancy.
Symptoms and consequences of type 2 diabetes
Unlike type 1 diabetes, T2DM develops slowly and imperceptibly: mild or moderate hyperglycemia does not manifest itself at all for a long time (often years). However, a violation of glucose metabolism can be detected already at the asymptomatic stage - by chance or during a routine preventive examination.
If this can be done at the very beginning, the onset of the disease can at least be delayed, and without any treatment. A good night's rest, stress relief, weight loss and diet correction can restore hormonal regulation, improve metabolism and forget about the problem for many years.
The first symptoms of type 2 diabetes, as a rule, occur when the disease has already started, hyperglycemia is persistent and the person needs glucose-lowering therapy.
What are the first symptoms of type 2 diabetes to appear?
At first, an increase in blood sugar signals itself with the following symptoms:
- dry mouth, thirst, resulting in a person drinking a lot of liquid;
- causeless weakness and drowsiness - diabetics constantly feel sleep-deprived and quickly get tired during physical and mental stress;
- frequent urination, including at night;
- skin itching, which is most pronounced in areas with thin skin (for example, in the perineal area in women);
- bulimia (abnormally high appetite);
- slow and poorly healing wounds - in a patient with diabetes, even the smallest scratches do not heal well;
For a diabetic, even a small scratch can become a big problem.
- blurred vision (veil before the eyes) due to damage to the vessels of the retina;
- numbness of the limbs (manifestations of diabetic neuropathy).
Symptoms for moderate to severe disease
As type 2 diabetes progresses, the symptoms become more pronounced, and the above symptoms are accompanied by manifestations of dysfunction of various organs.
Brain and heart cells need glucose and oxygen the most. They are the first to “get hit”, experiencing chronic oxygen starvation and lack of “fuel”. In addition, excess sugar in the blood leads to obliteration of arterial vessels - they lose elasticity and firmness (become “glassy”), the lumen of the arteries narrows, and cholesterol plaques appear on the walls. As a result, patients:
- blood pressure rises;
- heart rhythm is disturbed;
- The risk of heart attack and stroke increases significantly.
Diabetes affects blood vessels, heart, brain, kidneys, lower limbs
If not detected in time and uncontrolled, the disease also affects other tissues and organs. In diabetics, the kidneys and liver suffer, resistance to infections decreases, osteoporosis develops, and trophic ulcers appear on the feet and legs. Any cold is fraught with serious complications, and pneumonia is extremely difficult to treat – this is also why covid is usually severe in people with type 2 diabetes.
Complications
If a person has diabetes, this can lead to serious consequences. First of all, the immune system deteriorates greatly. Because of this, for various diseases, recovery lasts much longer, and chronic pathologies appear.
Wounds heal much worse. Blood vessels and nerve tissues are also affected. Atherosclerosis gradually develops. Possible damage to the kidneys and eyes.
Another complication is diabetic foot syndrome. This area of the limb is considered the most vulnerable place for diabetes. Pathological changes can lead to inflammation, ulcers, and necrosis. In advanced cases, the leg may be amputated.
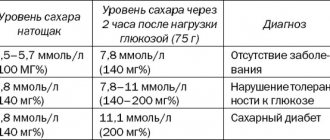
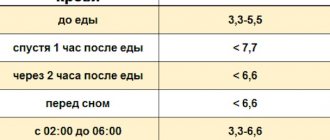
Diagnostics
In modern clinical practice, the diagnosis of diabetes mellitus is established based on the result of an analysis for glycated hemoglobin (HbA1C). Once in the blood, glucose molecules can penetrate into red blood cells and firmly bind to the receptors of the hemoglobin protein - glycate it. The more glucose in the blood, the more of its molecules “settle” on hemoglobin. Glucose is retained on the protein for 3-4 months, preventing it from performing its function - transporting oxygen and carbon dioxide.
Analysis for glycated hemoglobin reveals the percentage of such “long-occupied” molecules. In a healthy person this figure does not exceed 5.7%. A glycated hemoglobin level of 5.7% to 6% signals the first problems with glucose metabolism. When HbA1C increases to 6.1%-6.4%, prediabetes is indicated; a reading above these values indicates the presence of the disease.
Glucose attaches to hemoglobin receptors and prevents it from doing its “job”
Knowing the percentage of glycated hemoglobin, the doctor can not only make a diagnosis, but also monitor the course of the disease, adjusting treatment if necessary.
For type 2 diabetes, diagnosis also includes assessing pancreatic function. The choice of methods of glucose-lowering therapy depends on this indicator.
In addition, in diabetics, a “lipid panel” is determined, the condition of the kidneys, fundus of the eye, peripheral nerves and blood vessels is assessed, and if possible and necessary, 24-hour blood pressure monitoring (SBP) and cardiogram (Holter monitoring) are prescribed.
With an understanding of the course and proper treatment of type 2 diabetes, the symptoms of the disease lose their intensity, a person’s quality of life improves, and the risk of severe complications decreases.
Methods for treating type 2 diabetes mellitus
Treatment for type 2 diabetes is selected and carried out taking into account the stage of the disease, the state of the insulin-producing “islands of Langerhans” in the pancreas and associated pathologies.
With an HbA1C level of 5.7% to 6%, you can only manage by adjusting your diet and lifestyle. In the vast majority of cases, it is possible to normalize glucose metabolism and avoid the onset of the disease:
- reducing the consumption of sugar and fast carbohydrates;
- improving the quality of night sleep;
- weight correction;
- long walks, visiting the pool, gym;
- eliminating the source of constant stressful situations (if necessary, up to changing jobs, places of residence, etc.).
Recently, leading Western diabetologists have been persistently advising such patients to combine the above measures with taking medications that work in two directions:
- returning muscle cells the ability to respond to insulin and use glucose for their vital functions;
- slowing down and preventing the absorption of easily digestible carbohydrates in the intestines.
Can type 2 diabetes be cured without insulin?
If the pancreas is not yet completely “tired” and produces the hormone in the amount required by the body, you can reduce the level of glucose in the blood without insulin injections.
In mild cases of type 2 diabetes in the initial stages, medications that improve glucose metabolism in combination with a low-carbohydrate diet and sugar-lowering foods (artichoke, ginger, chicory, cinnamon, decoctions and infusions of blueberries, bean pods, etc.), as a rule, allow you to bring the disease under control . How well this works is judged by the level of glycated hemoglobin: during treatment it should not exceed 6.5% -7%. The analysis should be done no more than once every 3-4 months and no less than every six months.
If necessary, the endocrinologist adds other medications. Diabetics are also prescribed treatment aimed at supporting glucose-lowering therapy and preventing complications of the disease:
- antioxidant injections;
- magnetic therapy, which can reduce the manifestations of diabetic neuropathy and angiopathy, improve the functioning of the kidneys and pancreas;
- antihypertensive drugs, antiarrhythmics, etc.
Important! Every medicine has its own side effects. Therefore, during the treatment process it is necessary to undergo tests periodically. Based on their results, the doctor makes adjustments to the antidiabetic and auxiliary therapy regimen.
When is type 2 diabetes treated with insulin?
If the disease is diagnosed in the later stages, and the “worn out” gland is not able to produce the required amount of insulin, insulin therapy is added to the treatment regimen. The type of insulin, frequency of injections and dose are selected individually, focusing on blood sugar levels and the body’s response.
Global threat to all humanity
It is no coincidence that World Diabetes Day is celebrated on November 14th. It was on this day that the Canadian doctor Frederick Banting , the discoverer of insulin, was born, who in 1922 gave the first insulin injection to a patient in history, and in 1923 received the Nobel Prize for his discovery. Since then, much research has been carried out in world medicine and pharmaceuticals on the treatment and prevention of this terrible disease, but every year the problem of the spread of diabetes mellitus on a global scale is becoming more acute. According to WHO, over the past 30 years, the prevalence of diabetes mellitus has been growing along with the prevalence of obesity and overweight: in 1980, 108 million people with diabetes were registered in the world, and by 2014 their number had already increased to 422 million. The incidence of diabetes is growing especially rapidly in low- and middle-income countries.