- How to lower blood sugar
- Signs and dangers of high sugar levels
- Diet correction
- Lifestyle change
- Express ways to lower blood sugar
- Switch to healthy sugar substitutes
Blood glucose (sugar) levels are a serious marker of health and well-being, and unhealthy simple carbohydrates raise them dangerously. Sweeteners, which are produced under the name, help to avoid them. But what to do if glucose levels are already elevated and how to lower blood sugar? We answer pressing questions in the article.
Signs and dangers of high sugar levels
It’s not just people with diabetes who need to lower their sugar levels and control their glucose levels. This pathology occurs in other endocrine disorders that require immediate action, specialist help and daily attention.
Glucose increases due to stress, obesity, liver dysfunction, immune system, alcohol abuse and many other reasons. Its high level is a serious stress for the pancreas. It cannot cope with the load, which is why the body’s metabolism is globally disrupted and dangerous diseases develop, including prediabetes and diabetes.
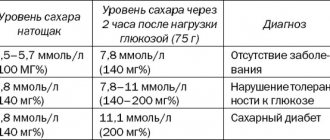
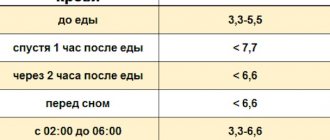
The normal blood sugar level for an adult is 3.3-5.5 mmol/liter on an empty stomach and up to 6.6 mmol/liter after meals.
If the parameter increases, the person becomes weak, gets tired quickly, begins to feel dizzy, has a headache, his weight jumps unreasonably and greatly, and his vision deteriorates. Other signs of the need to lower sugar are frequent urination, itchy skin, the appearance of a white coating on the tongue, and constant thirst.
If these symptoms occur, you need to take action and consult a doctor as soon as possible. Exceeding the blood sugar threshold can lead to dangerous pathologies, including:
- diabetes and its complications - ketoacidosis, hyperglycemic coma;
- dangerous vision pathologies - glaucoma, cataracts, complete blindness;
- renal failure;
- heart attack, stroke and vascular atherosclerosis.
Types of secretagogues
Secretagogues have been used in endocrinological practice for more than half a century. The medications have a pronounced hypoglycemic effect, but cause many side effects. First of all, incorrect use of secretagogues threatens a hypoglycemic crisis.
Long-term treatment provokes taphylaxis (addiction and decreased therapeutic effectiveness). The aggressive effects of the tablets over time lead to cell death and endogenous pancreatic dysfunction. The group is represented by two types of drugs that are similar in action.
Sulfonylurea derivatives
| pharmachologic effect | Side effects and contraindications | Basic principles of pharmacodynamics | Additionally |
| They force pancreatic cells to synthesize an increased amount of insulin, inhibit the activity of the enzyme that breaks down insulin (insulinase), inhibit the formation of glucose molecules from amino acids (gluconeogenesis), and slow down the breakdown of fats. | Hypoglycemia, changes in blood composition, epidermal dermatitis, difficult and painful digestion, disturbance of intestinal microflora. Not used during the perinatal and lactation periods, for chronic diseases of the renal system, liver and thyroid gland | The binding to proteins is about 97%; the maximum concentration in the body of the drug is reached 4 hours after administration. Excretion is carried out by the kidneys | With long-term use, pancreatic cells are killed, as a result of which the diabetic is transferred to insulin injections. Provoke polygaffia (increased appetite), which leads to excess body weight gain |
Meglitinides, or benzoic acid derivatives
| pharmachologic effect | Side effects and contraindications | Basic principles of pharmacodynamics | Additionally |
| Stimulate pancreatic cells to actively produce insulin, slow down gluconeogenesis and lipid breakdown | Hypoglycemia, allergies, liver and kidney dysfunction. Contraindicated in juvenile diabetes, during pregnancy and breastfeeding | Maximum activity is observed after 30 minutes, biotransformation takes place in the liver | Act short term but aggressively |
Diet correction
To maintain glucose within normal limits and reduce its level, you must first adjust your diet - eliminate or seriously limit foods that cause sugar levels to rise. This:
- sugar-containing sweets and products - baked goods, confectionery, carbonated drinks, juices and industrial jams;
- dishes containing simple carbohydrates - pasta, white flour bread, sweet fruits and honey, potatoes;
- canned and processed meat products - sausage, ham;
- industrial sauces, pickles, fatty meats.
It is necessary to give preference to foods that lower blood sugar. Their difference is a low glycemic index (less than 20-30) and the content of substances that normalize glucose. These are primarily green vegetables. Cabbage, spinach, zucchini, cucumbers, asparagus, celery and a variety of greens slow down the absorption of glucose and normalize metabolism.
Cinnamon is also useful. It directly affects sugar in the body, normalizes protein metabolism, and improves the functioning of the pancreas. Other spices that help overcome glycemia include fenugreek and rosemary (they reduce the amount of “bad” cholesterol in the body), bay leaf, ginger, turmeric and cloves.
You also need to add a number of other products to your diet:
- vegetables with a low glycemic index - onions, turnips, Jerusalem artichokes, pumpkin, beets, radishes;
- cereals and legumes - buckwheat, peas, lentils;
- fruits and berries - sour and sweet and sour apples, citrus fruits, black currants, cherries, blueberries and cranberries;
- sources of healthy fats - avocado, sunflower seeds, olive oil, salmon and sardines;
- nuts (little by little) - almonds, hazelnuts, walnuts, cashews;
- whole grain bread – reduces the level of “bad” cholesterol, has a low glycemic index and contains fewer carbohydrates than regular bread;
- oat bran – due to beta-glucans in its composition, it reduces the level of glucose, insulin and lipids in the blood;
- Garlic – It is found in many medications and dietary supplements for diabetics, as it significantly lowers blood sugar levels and improves insulin sensitivity.
Groups of hypoglycemic drugs
Tablets that lower blood glucose levels are divided into several groups. The classification of medications is determined by their effect on biochemical processes associated with the formation and consumption of insulin and glucose. Depending on the stage of diabetes, the individual characteristics of the patient and therapeutic dynamics, the endocrinologist prescribes drugs from one group or combination treatment with different antidiabetic tablets.
There are four main groups of tablets for the treatment of insulin-resistant diabetes mellitus:
- Sulfonylurea derivatives and benzoic acid derivatives (meglitinides). Medicines are combined into a group of secretagogues that stimulate the pancreas to actively produce insulin.
- Guanidine derivatives (biguanides) and glitazones (otherwise thiazolidinediones). They are representatives of a group of sensitizers whose action is aimed at restoring the sensitivity of the body's cells and tissues to insulin.
- Alpha-glucosidase inhibitors. The drugs do not affect the production and absorption of insulin. Their task is to inhibit fermentation processes, as a result of which the absorption of glucose into the systemic bloodstream slows down.
- Dipeptidyl peptidase (DPP-4) inhibitors. They stimulate the production of pancreatic hormone and inhibit the synthesis of glucagon (an insulin antagonist) by blocking DPP substances that destroy digestive hormones (incretins).
List of tablets by group affiliation
| Secretagogues | Sulfonylurea derivatives | Diabeton, Gliquidone, Gliclazide, Glimepiride, Maninil, Amaryl, etc. |
| Benzoic acid derivatives | Novonorm, Starlix, Repaglinide, Nateglinide. | |
| Sensitizers | Guanidine derivatives | Siofor, Glucophage, Diaformin, Glycomet, Metformin |
| Thiazolidinediones | Avandia, Actos, Rosiglitazone, Pioglitazone | |
| Alpha-glucosidase inhibitors | Glucobay, Miglitol | |
| Dipeptidyl peptidase inhibitors | Januvia, Galvus Ongliza | |
| Combined agents (sensitizers and dipeptidyl peptidase inhibitors) | Janumet, Galvusmet | |
The dosage and regimen of taking tablets is determined by the treating endocrinologist individually for each patient.
Additionally
In addition to tablets, the latest hypoglycemic drugs in the form of a syringe pen are used in the treatment of diabetes mellitus - incretins (glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide). These are representatives of the hormones of the gastrointestinal tract.
Their active synthesis occurs when food enters the body. The biochemical effect is based on enhancing the production of insulin and inhibiting the production of glucagon. As a result of the use of incretins, it is possible to avoid an increase in glucose levels. In Russia, two types of drugs in this category are used: Byeta and Victoza.
Incretins are produced by European pharmacological companies Bayeta - Astrazeneca UK Limited (UK) and Victoza - Novo Nordisk (Denmark)
Medicines do not have a negative effect on the kidneys, liver and other organs of the hepatobiliary system. Regular use of the drugs helps reduce body weight, which is especially important for obese diabetics.
Byeta and Victoza are not prescribed for liver and kidney failure, progressive diabetic ketoacidosis, or during pregnancy and breastfeeding. There are few side effects from taking the medications. They may be associated with individual allergic reactions (redness of the skin in the injection area), or heaviness in the epigastric region.
Lifestyle change
In addition to adjusting the grocery list, it is important to change your daily routine. Glucose levels will be reduced by quitting smoking and excessive alcohol consumption - habits that are dangerous to the pancreas. It is important to drink at least 1.5-2 liters of water per day, including herbal infusions, green tea, linden decoction, in order to more effectively remove sugary compounds from the body.
It is advisable to “break” the entire daily amount of food into portions and eat little by little, but more often. Optimally, five times a day, including two small snacks. Proper sleep and control of emotional health reduce stress, and therefore glucose levels.
Add sports to your life. The more a person moves, the more efficiently the body uses glucose. You can choose one of the types of load recommended by doctors:
- swimming;
- yoga, Pilates, gentle exercises like tai chi;
- cycling or roller skating;
- slow jogging;
- hiking, Swedish walking (with special poles).
Dipeptidyl peptidase (DPP-4) inhibitors
Medicines reduce blood glucose levels by stimulating the digestive tract hormones incretins (glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide). Inhibitors do not put constant pressure on the pancreas; insulin production occurs only during digestion (at times when sugar levels rise), and not constantly, as when taking other hypoglycemic drugs.
Thus, it is possible to lower glucose levels, maintain stable glycemia and glycosylated hemoglobin. At the same time, without overloading the pancreatic cells. The effect of the medication reaches its highest activity after three hours, bioavailability is more than 85%. The elimination process is carried out by the renal apparatus.
A valuable property of inhibitors is their lack of effect on appetite and body weight. Medicines are contraindicated in patients with insulin-dependent type of diabetes, with the development of ketoacidosis, with exacerbation of chronic inflammatory processes in the gastrointestinal tract (gastrointestinal tract).
Combined products
In the treatment of diabetes mellitus, a combination of DPP-4 with Metformin (sensitizer) is used. For ease of administration, pharmacological companies have developed combined tablets Janumet and Galvusmet. The combination of Metformin and dipeptidyl peptidase inhibitors has a different ratio.
Only an endocrinologist can determine the correct dosage of tablets. In parallel with hypoglycemic drugs, diabetics are prescribed dietary supplements that have a positive effect on the absorption of carbohydrates in case of impaired metabolism.
Express ways to lower blood sugar
If you need to reduce your glucose as quickly as possible, within a week or a day, do not take any medications without the advice of a doctor. Instead, you can resort to safe products and recipes available at home:
- chicory decoction on an empty stomach (they are recommended to replace coffee) - the dry collection is poured with boiling water and left for up to two hours;
- rosehip infusion - dried or fresh berries are poured with boiling water and left for 10-12 hours;
- oat milk - a glass of bran or natural flakes is poured with a liter of boiling water, left for 10-12 hours (preferably in a thermos) and drunk on an empty stomach at least three times a week;
- low-fat kefir with cinnamon (a pinch per glass of liquid) - on an empty stomach plus an hour before bedtime;
- sauerkraut and its juice - you can drink 1/3 glass several times a week;
- infusion of linden blossom, black currant leaves, nettle, bay leaf or hawthorn - pour boiling water over them, leave for half an hour and drink 100-150 ml before meals.
Results
Hypoglycemic tablets are allowed for use only on the recommendation of a doctor. Individual regimens and dosages of medications have been developed for patients with type 2 diabetes mellitus. Tablets of several pharmacological groups help reduce blood glucose levels:
- secretagogues (sulfonylurea derivatives and meglitinides);
- sensitizers (biguanides and glitazones);
- alpha-glucosidase inhibitors;
- DPP-4 inhibitors.
The newest medications are incretins, available in the form of a syringe pen.
Switch to healthy sugar substitutes
In order not to limit yourself to sweets and not experience stress because of this, which increases glucose levels, it is worth switching to sweeteners - always carbohydrate-free, with a low glycemic index.
The choice of sugar substitutes is quite large. It is important to understand that not all of them are useful. Thus, artificial sweetener can cause allergies or eating disorders. Most synthetic supplements contain carcinogens that affect hormonal levels and overall well-being. If they are abused, they can cause headaches and causeless mood swings.
We recommend including natural supplements in your diet to minimize the risk of diabetes complications. One of them is stevia, a natural, non-nutritive sweetener that contains no carbohydrates. Doctors officially recommend it as a means to improve well-being in diabetes. Replacing sugar with stevia in your daily diet will reduce your daily caloric intake by 25%.
Buy stevia
This sweetener contains diterpene glycosides, vitamins and other components to effectively correct glucose levels. Products based on honey grass extract normalize carbohydrate metabolism and sugar absorption and are useful for the prevention and treatment of diabetes.
The sweeteners of our brand have almost zero calorie content and, thanks to multi-stage purification, do not taste bitter. Their sweetness relative to sugar is up to 400:1. With products from our brand, you can more effectively lower your glucose levels, feel good, stay healthy and vigorous.
CALL +7 499 390 31 53 or
Clinical pharmacologist to assist the endocrinologist: the choice of oral glucose-lowering therapy
Currently, there is a wide arsenal of inpatient and outpatient agents that can affect almost all known links in the pathogenesis of type 2 diabetes mellitus (DM). There are many classifications of them, including division by main effect, by points of application, by mechanism of action, by duration, etc.
There are hypoglycemic agents and antihyperglycemic agents. The purpose of hypoglycemic drugs (sulfonylurea derivatives and meglitinides) is to stimulate the synthesis of endogenous insulin, as a result of which, among the positive aspects of treatment, negative events also occur: weight gain and an increased risk of developing hypoglycemic conditions.
Antihyperglycemic drugs (α-glucosidase inhibitors, biguanides, thiazolidinediones, incretin mimetics) improve peripheral glucose utilization, but do not have a stimulating effect on pancreatic β-cells. Due to this, the level of insulin in the blood does not increase and blood glucose does not decrease below normal [1].
Antihyperglycemic agents affecting the small intestine prevent complete absorption of carbohydrates in the intestine by inhibiting α-glucosidase enzymes that affect the pancreas (secretogens) - causing its β-cells to secrete endogenous insulin, and affecting hepatocytes, adipose and other peripheral tissues (sensitizers) - increase the sensitivity of target organs to insulin.
Examples of secretogenic hypoglycemic drugs are sulfonylureas (glibenclamide, gliclazide, glimepiride) and prandial glucose regulators - meglitinides (nateglinide, repaglinide). Sensitizers are represented by biguanides (metformin) and thiazolidinediones (pioglitazone, rosiglitazone).
A relatively new class of glucose-lowering drugs are incretin mimetics (vildagliptin, saxagliptin, exenatide, liraglutide), the insulinotropic effect of which is glucose-dependent and is realized only at elevated glycemic levels. When normoglycemia is achieved, the insulin concentration returns to the basal level, which helps reduce the risk of developing hypoglycemia while taking these medications. The mechanism of action of these drugs is glucose-dependent and does not interfere with the normal glucagon response to hypoglycemia [2]. The main classes of oral hypoglycemic drugs and their mechanisms of action are presented in Table. 1 and in Fig. 1.
The reader is presented with dozens of names of medicines belonging to different pharmacological groups, each with its own mechanism of action, evidence base and cost. With such an abundance of medications, within a short period of communication with the patient, as well as in conditions of comorbidity and forced polypharmacy, choosing the right medication in an adequate dosage regimen is very difficult to do - almost impossible, which dictates the need to designate the clinical and pharmacological niches of these drugs, as well as their advantages and disadvantages (Fig. 2–8).
α-glucosidase inhibitors should be used primarily for the prevention of type 2 diabetes mellitus in patients with early manifestations of insulin resistance. In addition, they are the drugs of choice for people with prediabetes, which is accompanied by postprandial hyperglycemia at normal fasting levels (reduction in HbA1c levels by 0.5–0.8%).
Indications for prescribing glinides are type 2 diabetes mellitus when diet and exercise are ineffective. They are also designed to preferentially reduce postprandial hyperglycemia (0.5% to 1.5% reduction in HbA1c).
The clinical niche for the prescription of glitazones (thiazolidinediones) is reduced to type 2 diabetes mellitus, as monotherapy or in combination with a sulfonylurea drug, biguanides or insulin in the absence of effect from diet therapy, exercise and monotherapy with one of the above drugs (reduction of HbA1c level by 0 .5–1.4%).
Biguanides are the drugs of choice both for people with prediabetes, accompanied by fasting hyperglycemia and with normal sugar levels after meals, which indirectly indicates insulin resistance, and for patients with type 2 diabetes mellitus. Their administration is possible in the form of monotherapy and in combinations, primarily with secretogens (when the latter do not provide complete correction of hyperglycemia) and with insulin (in the presence of insulin resistance) (reduction of HbA1c levels by 1–2%).
The administration of sulfonylurea derivatives is usually associated with the presence of type 2 diabetes in cases where diet and exercise, the administration of α-glucosidase inhibitors and biguanides were ineffective (reduction in HbA1c levels by 1–2%).
Drugs with incretin activity (Fig. 7), which primarily affect GLP1, are prescribed for type 2 diabetes as an addition to therapy with biguanides, sulfonylurea derivatives, thiazolidinediones in case of inadequate glycemic control (reduction in HbA1c level by 0.8–1.8 %).
Another type of incretin mimetics are drugs that affect DPP4 (Fig. 8), which are advisable to prescribe for type 2 diabetes mellitus as monotherapy in combination with diet therapy and exercise; in combination with biguanides as initial drug therapy when diet therapy and exercise are insufficiently effective; as well as as part of two-component combination therapy with biguanides, sulfonylurea derivatives, thiazolidinediones or insulin in case of ineffectiveness of diet therapy, exercise and monotherapy with these drugs (reduction in HbA1c levels by 0.5–1.0%).
The mechanism of action of DPP4 inhibitors is as close as possible to the natural processes occurring in a healthy human body. Under their influence, there is a decrease in the frequency of protective snacks that patients eat to avoid hypoglycemia, a decrease in the absorption of fat from the intestine, an increase in energy expenditure, and an increase in lipid oxidation during meals [3]. In addition, in diabetes, as a result of increased apoptosis, β-cells lose their mass, which is reflected in significant impairments in their functions, the main of which is insulin synthesis. The physiological effect of this group of drugs supports the viability of pancreatic β-cells, increases their mass by 75% and reduces apoptosis by 65% [4]. A comparison of the main representatives of DPP4 inhibitors is presented in table. 2.
The cardiovascular effects of DPP4 inhibitors are reduced to reducing myocardial remodeling, improving endothelial function, reducing atherogenic lipoprotein fractions, lowering blood pressure (BP), reducing symptoms of circulatory failure, protecting the myocardium from ischemia, as well as functional restoration of the myocardium after ischemia and increasing the number of receptors to insulin in cardiomyocytes [5]. Cardiometabolism of DPP4 inhibitors is presented in Table. 3.
Summary data reflecting the advantages and disadvantages of the main classes of glucose-lowering drugs are presented in table. 4.
As can be seen from the table presented:
- in case of cardiovascular diseases, patients should avoid drugs with a high likelihood of developing hypoglycemia, which can be very dangerous for them;
- overweight patients should be prescribed antihyperglycemic drugs that do not promote further weight gain;
- when treating women of childbearing age, the possibility of pregnancy should be taken into account, in which tableted hypoglycemic drugs are contraindicated;
- all tableted hypoglycemic drugs are contraindicated in persons with diabetic ketoacidosis;
- in patients with alcoholic visceropathy and liver cirrhosis, the choice of hypoglycemic therapy should be based on the characteristics of the drug’s metabolism, as well as the duration of its action;
- in patients with CKD (including those resulting from diabetic nephropathy), glycemic correction should be carried out under the control of glomerular filtration rate (GFR).
The inability to maintain compensation of carbohydrate metabolism in patients on monotherapy, as well as the high risk of developing acute and chronic complications of diabetes mellitus in comorbid patients are sufficient grounds for combination treatment. In the case of combined glucose-lowering therapy, improvement in the effectiveness of treatment is a consequence of the combination of the mechanisms of action of drugs (for example, secretogens and sensitizers) [6]. Combination therapy is accompanied by an improvement in the quality of life of patients and is well tolerated by them, which is associated with a parallel effect on different parts of the pathogenesis of diabetes and with a decrease in the number of simultaneous administration of tablet drugs while improving the compensation of carbohydrate metabolism (Fig. 9).
However, the evolution of oral glucose-lowering agents continues - in November 2012, the first representative of the newest class of oral sodium-glucose cotransporter type 2 (SGLT2) inhibitors, dapagliflozin, was approved in Europe, and in March 2013, the Food and Drug Administration The Food and Drug Administration (FDA) has approved canagliflozin for the treatment of adult patients with type 2 diabetes mellitus. Registration applications for empagliflozin, ipragliflozin and luseogliflozin have also been submitted to US, European and Asian regulatory authorities, with large-scale studies currently ongoing.
The mechanism of their action is as follows. Due to the active reabsorption system, this glucose is almost completely reabsorbed in the proximal tubule of the nephron. The urine entering the loop of Henle is free of glucose. An increase in the concentration of glucose in the blood plasma leads to an increase in its filtration in the glomeruli. When the rate of glucose entry into the proximal tubule increases above 260–350 mg/min/1.73 m2, for example in patients with diabetes, excess glucose exceeds the reabsorption potential and it begins to be excreted in the urine. In a healthy adult, this corresponds to a blood glucose concentration of about 10–11 mmol/L (180–200 mg/dL). Since glucose is not able to freely penetrate the cell membrane, sodium-dependent glucose transporters (SGLT1 and 2) are involved in its absorption in the intestine and reabsorption in the kidneys [7]. Accordingly, SGLT inhibitors reduce blood glucose concentrations by stimulating its excretion in the urine.
Expert opinion regarding registered SGLT2 inhibitors that have become an alternative to metformin, including in cases of intolerance, is ambiguous. On the one hand, drugs of this class offer new opportunities in the treatment of diabetes: first of all, a new, insulin-independent mechanism of action, no negative effect on body weight and even a slight decrease in weight, favorable pharmacokinetic properties and generally good tolerability [8]. On the other hand, the mechanism of action of SGLT2 inhibitors is aimed at the clinical manifestations of diabetes, and not at its cause [9]. Due to SGLT2 inhibition, the degree of glycosuria depends on renal function, and since in patients with diabetes it decreases as the disease progresses, the long-term effectiveness of these drugs remains unknown. In addition, the presence of glucose in the urine has always been considered an undesirable phenomenon, and many doctors are not ready to prescribe drugs that cause glucosuria. The latter is also the cause of the most common side effects - urinary tract infections and fungal infections of the genitals [10].
The clinical and pharmacological niches of this class of drugs will be revealed by time, and the answers to many questions should be dispelled by the results of clinical studies of these drugs, but today there is no doubt about the postulate that when choosing a hypoglycemic drug, the doctor must remember that in each specific case adequate therapy for diabetes is possible only if the patient’s age, sex, gender characteristics, body weight, as well as the etiological and pathogenetic mechanisms of the development of the disease are taken into account.
Literature
- De Fronzo R. Pharmacologic therapy for type 2 diabetes mellitus // Ann Inter Med. 1999; 131:281–303.
- Dedov I. I., Shestakova M. V. Incretins: a new milestone in the treatment of type 2 diabetes mellitus. M., 2010. pp. 55–62.
- Rosenstock J. Comparison of vildagliptin and rosiglitazone monotherapy in patients with type 2 diabetes: double-blind, randomized trial // Diabetes Care. 2007, 30(2): 217–223.
- Matikainen N. Vildagliptin therapy reduces postprandial intestinal triglyceride-rich lipoprotein particles in patients with type 2 diabetes // Diabetologia. 2006, 49: 2049–2057.
- Duttaroy A. The DPP-4 inhibitor vildagliptin increases pancreatic beta-cell neogenesis and decreases apoptosis / Poster No. 572 presented at ADA, 2005.
- Balabolkin M.I., Klebanova E.M., Kreminskaya V.M. Combined hypoglycemic therapy and the possibility of achieving long-term compensation of carbohydrate metabolism in patients with type 2 diabetes mellitus // Russian Medical Journal. 2007, no. 17, p. 492–496.
- Hardman TC, Dubrey SW Development and Potential Role of Type-2 Sodium-Glucose Transporter Inhibitors for Management of Type 2 Diabetes // Diabetes Ther. 2011; 2 (3): 133–145.
- Experts Express Mixed Thoughts on Canagliflozin Approval. Medscape Medical News. Apr 18, 2013. https://www.medscape.com/viewarticle/782712.
- Kim Y., Babu AR Clinical potential of sodium-glucose cotransporter 2 inhibitors in the management of type 2 diabetes // Diabetes Metab Syndr Obes. 2012; 5:313–327.
- Ushkalova E. A. A new class of antidiabetic drugs - inhibitors of sodium-glucose cotransporters // Pharmateka. 2013, no. 16, p. 33–36.
A. S. Skotnikov*, 1, Candidate of Medical Sciences M. G. Selezneva**
* State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after. I. M. Sechenova, Moscow ** GBUZ City Clinical Hospital No. 5 DZM, Moscow
1 Contact information
Honey and bee products
Diabetes mellitus, contrary to popular belief, is not a contraindication to the use of honey as a remedy. Honey has regenerative, anti-inflammatory, antibacterial properties, strengthens the immune system, heart and blood vessels. Diabetics are allowed in small quantities. Preference should be given to varieties with the lowest glycemic index (acacia, chestnut, buckwheat).
To prepare the medicine, a liquid version of the product is used. It is recommended to consume honey not in its pure form, but in combination with nuts or bee products (propolis, dead bees). A mixture of honey and propolis is an effective remedy for stimulating the intrasecretory activity of the pancreas. Grind ten grams of propolis and dissolve in a water bath, mix with 200 g. honey
For daily use, 1 teaspoon is enough. The mixture should not be swallowed, but dissolved slowly. Bee dead contains the powerful antioxidant chitosan, which accelerates regeneration processes. Vodka tincture from dead bees is prepared at a ratio of 1:1. Infuse for 30 days in a dark place. Add to honey water (250 ml of water, a teaspoon of honey and tincture).
Before using bee kill, you should consult your doctor. Medical treatment is contraindicated in the stage of decompensated diabetes
Ways to normalize hyperglycemia
The state of acute hyperglycemia in diabetic patients is relieved in a hospital setting. Emergency medical care and subsequent treatment can prevent the development of diabetic coma. If the sugar level is not critically elevated and the condition is not urgent, diabetics use traditional medications to stabilize glycemia: tableted hypoglycemic drugs for the insulin-dependent type of the disease, injections of medical insulin for type 1 diabetes.
In addition to medications, the following methods of neutralizing hyperglycemia are used:
- Diet correction.
- Physiotherapy.
- Traditional medicine recipes.
Important! Uncontrolled independent attempts to reduce sugar can be harmful to health. If the reference values deviate, you should consult a doctor and, if necessary, undergo additional examination.