The President of the Society of Bariatric Surgeons of Russia, member of the board of the International Federation for the Surgery of Obesity (IFSO), Doctor of Medical Sciences Yuri Ivanovich Yashkov talks about the prospects for treating type 2 diabetes mellitus using surgical methods.
First of all, it is necessary to identify the subject of conversation. We will only talk about type 2 diabetes, or as it is also called non-insulin-dependent diabetes mellitus, which usually develops in adulthood, and, as a rule (in 85-90% of cases), against the background of excess body weight. We will not touch upon the treatment of type I diabetes mellitus, since its development occurs by a completely different mechanism and, therefore, the approaches to treatment are completely different.
Type 2 diabetes mellitus is a global problem
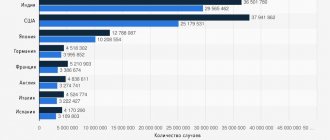
Why are we talking about the relevance of the problem of type 2 diabetes? Unfortunately, experts note an exceptionally rapid increase in incidence. According to the World Health Organization, more than 150 million people worldwide suffer from diabetes. In industrialized countries, type II diabetes occurs in 5-6% of the population. Even with modern treatments, diabetes continues to be the fourth leading cause of death in the United States. In our country in 1993-1996. About 2 million patients suffering from diabetes mellitus are registered, of which 1 million 700 thousand (85%) are patients with type II diabetes. It is estimated that after 65 years, every twelfth person suffers from diabetes, and this figure reflects only those who know about their disease and are registered with an endocrinologist. This is a very “expensive” disease: for example, in the USA, the average cost of treating one diabetic patient is $368 per month. And much more impressive are the figures reflecting the cost of treating complications that develop as a result of diabetes.
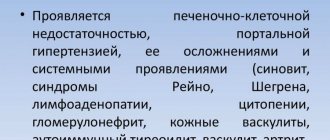
What are these complications? I will name the main ones:
- Nephropathy
resulting in renal failure. - Retinopathy
is damage to the retina of the eyes with the risk of vision loss. - Polyneuropathy
is a lesion of the peripheral nervous system. - The development of atherosclerotic vascular lesions
, and what is especially characteristic of diabetes is diabetic foot syndrome with the threat of limb amputation. In turn, the progression of atherosclerosis with uncorrected diabetes inevitably leads to the development of cardiovascular diseases (myocardial infarction, strokes), which are the main cause of mortality in the population.
Conservative methods of treating diabetes mellitus
Today, dietary products have been developed for those who suffer from diabetes, and “schools” operate where each patient can undergo special training. Is it possible to solve the problem of diabetic patients using these methods? It is possible, provided that the patient strictly follows the recommendations of an endocrinologist throughout his life. Treatment of type II diabetes mellitus primarily involves a radical change in lifestyle, changing decades-old dietary patterns and behavior. An endocrinologist will first of all explain to his patient how to eat properly, which foods should be avoided, and which ones should be consumed first. One of the indispensable recommendations will be advice to reduce body weight. The question is whether the patient will be able to eat on a limited basis, count calories and voluntarily for the rest of his life refuse to eat his usual fatty, floury, sweet foods in favor of crackers, vegetables, fruits and dietary products. The body will inevitably respond with a rise in blood sugar to any diet violations, and the more often and to a greater extent these violations occur, the greater the likelihood of complications developing. The question is whether our patient, who is no longer completely healthy, suffering from high blood pressure and shortness of breath, will be able to start playing sports and physical labor in his 40s, 50s, and 60s? Hardly. As practice shows, most people living in the modern world do neither of these things.
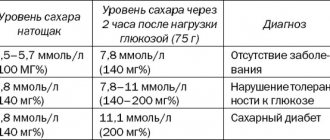
In recent years, a large number of different glucose-lowering drugs have been proposed. What can you say about this? Yes, indeed, many patients suffering from type 2 diabetes are forced to constantly take glucose-lowering medications. But do all of them normalize their blood glucose levels during the day? This can be easily checked by performing a fairly simple test for glycated (the term “glycosylated” is also used) hemoglobin. If the result exceeds the norm, this means that over the past 2-3 months episodes of increased blood glucose have occurred, and there is no question of compensation for diabetes. I have seen many who were constantly taking glucose-lowering medications, and despite this, their blood glucose levels were significantly higher than normal. Effective treatment and the illusion of treatment are completely different things. Of course, detection of elevated blood glucose levels is a signal that it is necessary to contact an endocrinologist and, under his guidance, begin the necessary treatment measures.
Is glucose good for diabetes?
11.06.2020
By 1950, the number of patients with metabolic syndrome and type 2 diabetes
Metabolic syndrome is a precursor to diabetes mellitus . During illness, the mass of visceral fat increases. the hormone produced in beta cells and stops responding to it. The level of glucose (dextrose) in the blood .
Diabetes mellitus is a disorder resulting in hyperglycemia. In the first type of disease, the pancreas does not produce enough hormone that controls the breakdown of carbohydrates and their absorption. Organ tissues stop responding to metabolism.
Non-insulin-dependent diabetes (type 2) develops in a person who consumes a lot of unhealthy foods. These are not necessarily sweets. Cells do not have time to absorb sugar. Sensitivity to the hormone decreases. The disease often occurs due to excess weight and gouty arthritis.
Nutritionists have replaced regular sugar with fructose (levulose, arabino-hexulose), which does not affect the release of insulin. But the number of patients has increased to two hundred million people. It is not associated with obesity . Scientists have suggested that the reason is a natural sweetener.
Harm from fructose
Sugar is a disaccharide, consisting of two carbohydrates: fructose and glucose. The liver metabolizes monosaccharides . This exocrine gland modifies levulose into dextrose, glycogen and lactose. But the cleansing organ cannot cope with excess of the norm; the excess turns into fat. the kidneys and heart increases .
Fruit sugar slows down the formation of leptin, hormone . A person eats more than normal, which reduces insulin production. Levulosis does not stimulate the formation pancreatic hormone . Liver cells stop perceiving it. The absorption of sugar is impaired, its level in the blood remains high. Fat accumulates faster. Type 2 diabetes develops
Between 1999 and 2004, fructose use increased by a third. During this time, the number of patients with hyperglycemia increased. Among them were teenagers.
The United States ranks first in the number of diabetics - 27 million, which is 20% of the people in the country. In America, since 1970, corn syrup has been added to dishes instead of sugar. The content of levulosis in it reaches 95%.
Benefits of fructose
Metabolic disorders cannot be treated. But diabetics need to stay healthy. Physical activity, proper nutrition, and blood are a recipe for good health.
Fructose in moderation is beneficial. It does not enter the liver in its pure form; it promotes the breakdown of carbohydrates in the digestive tract and their subsequent absorption into the blood . Controls the main enzyme of glucose metabolism, regulates the connection of glycogen. In hepatocytes, fruit sugar is converted to dextrose.
Everything needs moderation. Eating too little and only low-calorie foods is harmful. For humans, storing fat tissue is a natural process. The normal fat content in women is up to 20%, and in men – 17%. A strict diet without a drop of sweets causes ketosis - carbohydrate starvation of cells.
Published in Endocrinology Premium Clinic
When do surgeons come to the rescue?
Why is the question of using surgical methods for the treatment of type 2 diabetes mellitus being raised today? The fact is that surgeons who use operations aimed at reducing body weight note a clear positive effect of these operations on the course of type 2 diabetes mellitus, which, as already mentioned, most often develops precisely as body weight increases. It is well known that type 2 diabetes most often occurs in individuals with abdominal (intra-abdominal, visceral, android) type of obesity.
When is it necessary to contact a surgeon ? Firstly, in cases where, when type II diabetes is detected, your weight is significant, i.e. more than 40-50 kg exceeds the norm. In this case, the surgical operation will not only effectively reduce weight, but will also, most likely, save you from the need to follow a special diet, as well as take glucose-lowering medications, and even more so, from the need to inject additional insulin. It must be borne in mind that weight loss caused by surgery also effectively affects the course of other diseases associated with obesity and diabetes (arterial hypertension, respiratory failure, diseases of the joints and spine, hypercholesterolemia and a number of other problems associated with obesity).
Secondly, consultation with a specialist surgeon is also advisable when the patient fails to achieve the desired goal - compensation of carbohydrate metabolism - using conservative methods (diet therapy, treatment with glucose-lowering drugs, etc.). That is, essentially when the patient himself is not able to change his previous lifestyle: eat limited food, give up favorite foods, switch to a special diet, stop overeating at night, significantly increase physical activity.
Thirdly, when type II diabetes mellitus is combined with high levels of cholesterol and triglycerides in the blood, especially with the so-called “familial hypercholesterolemia”. With this combination, the risk of cardiovascular disease increases sharply. The operations in question, along with the normalization of carbohydrate metabolism, effectively reduce cholesterol and triglycerides in the blood.
The right foods for diabetics
Now let's talk about those foods that should be included in the diet in large quantities, as well as those that are better to forget about.
To determine foods that are beneficial and harmful for diabetics, nutritionists and endocrinologists have introduced a universal indicator - the hyperglycemic GI index. Pure sugar, the hyperglycemic index of which is 100 units, was recognized as the reference product.
The safest and healthiest foods for diabetics have a GI value not exceeding 50 units:
- milk and dairy products - GI 35–40;
- lean meat and fish - GI 10–20;
- tomatoes, cucumbers, cabbage, lettuce, etc. - GI 5–15;
- nuts - GI 15;
- lentils and beans - GI 30–40, etc.
A low hyperglycemic index is not a guide to consuming these foods in unlimited quantities, but in general they will not harm a patient with diabetes, but, on the contrary, will help maintain normal blood sugar levels.
You should also consider “harmful goodies”:
- alcoholic drinks - GI above 85;
- chocolate - GI 70;
- sugar beet - GI 65;
- potatoes - GI 65;
- white bread - GI 90;
- corn flakes - GI 85, etc.
A high GI does not mean that foods that are “bad” in carbohydrate content should be completely and forever abandoned. You just need to consume them rarely and in strictly limited quantities so as not to provoke exacerbation of diabetes.
The effectiveness of surgical treatment
When the result of the operation becomes obvious, i.e. Is there normalization of blood glucose levels? After the patient noticeably loses weight? No, this is observed almost from the second week after surgery, long before significant weight loss. The fact is that from the very first days after the operation the patient is forced to switch to a low-calorie diet, which he was not able to do before the operation. Secondly, the operation helps reduce the consumption and absorption of fat in the small intestine, which also helps reduce glucose levels. Gastric bypass and biliopancreatic bypass surgeries interrupt signals to the pancreas that cause it to work under constant strain. And, finally, subsequent weight loss helps reduce insulin resistance, a condition that underlies the development of diabetes. Thus, surgical methods used to treat obesity simultaneously affect several mechanisms of the development of type 2 diabetes mellitus.
What types of surgeries do you offer to patients who have type II diabetes? All types of operations aimed at reducing body weight to one degree or another have a positive effect on the course of diabetes, but gastric bypass
and
biliopancreatic bypass
.
What is the probability of achieving an effective result? According to American researchers, gastric bypass surgery leads to stable remission in type II diabetes mellitus in 92% of patients. Achieving sustained remission means there is no need for additional treatment aimed at lowering blood glucose. Those surgeons who use biliopancreatic bypass surgery guarantee their patients freedom from the need to take glucose-lowering medications. At the same time, patients can eat quite freely, i.e. There are practically no prohibitions on certain types of products.
That is, it will be possible to eat whatever you want, in any quantity, not take antidiabetic drugs and still have normal blood sugar? In fact this is true. For example, during biliopancreatic bypass surgery, the patient will quickly eat a small amount of food. Firstly, because at the same time the stomach decreases in volume. Secondly, because the rapid passage of food from the stomach into the ileum will contribute to early satiety. Thirdly, because the area of the small intestine where food is absorbed is reduced. And finally, and very importantly, this operation prevents the breakdown and absorption of fat in the small intestine, removing a significant part of the dietary fat in an undigested form. More detailed information about these operations can be obtained by consulting our Center.
Preoperative preparation of patients with diabetes mellitus
Diabetes is a high surgical and anesthetic risk factor,
BUT IS NOT A CONTRAINDICATION TO OPERATIONS
Postoperative complications and recovery period in patients with diabetes correspond to population values with fasting glycemia less than 8 mmol/l and postprandial less than 10 mmol/l
General principles of perioperative management of patients with diabetes
- Planned surgical interventions in patients receiving drug glucose-lowering therapy are performed in the morning (first of all)
- Intraoperative antibiotic prophylaxis is indicated for any surgery, including the “pure” type.”
- Particularly careful prevention of nausea, vomiting and gastrointestinal atony - with diabetic autonomic neuropathy and with decompensation of diabetes
- Monitoring regular bladder emptying to prevent ascending infection in autonomic neuropathy
- Mandatory non-drug and drug prophylaxis of venous thrombosis/embolism, especially in decompensated patients with diabetes
Examination of a patient with diabetes to reduce perioperative risk:
- Glycemia, ketonuria, HbA1c before elective surgery
- Degree of hydration (BP, diuresis), acid-basic acid (at least pH and bicarbonate), K+, Na+
- Coagulogram
- Cardiovascular system (before medium and major operations):
- ECG, blood pressure;
- Detailed medical history and orthostatic tests to diagnose diabetic autonomic neuropathy of the cardiovascular system (if present, high epidural and high spinal anesthesia are contraindicated)
- Ophthalmoscopy with pupil dilation.
- Kidneys and urinary tract: creatinine, proteinuria, GFR, history to diagnose autonomic neuropathy of the bladder
- Gastrointestinal tract: history taking to diagnose diabetic autonomic neuropathy (gastroparesis, enteropathy)
In the postoperative period in the surgical department:
- Regular meals, including intermediate meals;
- Express analysis of glycemia in the department and rapid correction of insulin dosage;
- Patients with type 2 diabetes, previously compensated on a diet or PSSP, should be transferred from insulin to PSSP/diet before discharge from the hospital only with full confidence in the absence of purulent-inflammatory complications and in good wound healing (optimally - not before the removal of sutures).
Features of drug therapy
| Planned therapy | On the eve of the operation | During surgery | ||
| Small operations | Moderate operations | Major surgeries | ||
| Diet | — | Glycemia every 3-4 hours | Infusion of 5% glucose, glycemia every 2–3 hours | Parenteral nutrition. Glycemia hourly, insulin have ready |
| Biguanides | Cancellation 48 hours before surgery | Glycemia every 3–4 hours | 5% glucose infusion, glycemia hourly | Infusion of 5–10% glucose, glycemia hourly. Before surgery – 50% (type 2 DM) or 80–100% (type 1 DM) IPD or NVVI |
| Sulfonylureas or glinides | If you can have dinner: take the usual dose; if not possible , reduce the dose by half | |||
| Other PSSP* | Cancel | |||
| IPD** | If you can have dinner: usual dose; if not possible , reduce by 20-50% | Before surgery, administer 50% of the morning dose of IPD. 5% glucose infusion, glycemia hourly | Infusion of 5–10% glucose, glycemia hourly. Before surgery – 50% (type 2 DM) or 80–100% (type 1 DM) IPD or NVVI**** | |
| ICD*** +IPD | If you can have dinner: the usual dose of ICD + IPD; if not possible - only IPD | |||
*Oral hypoglycemic drugs
**Long-acting insulin
***Short-acting insulin
****Continuous intravenous insulin administration
It is necessary to determine K+ before and after surgery. With normal kidney function and
normal K+ - 18–20 ml of 4% KCl solution for each liter of 5% solution
glucose (more in case of hypokalemia).
Galstyan G.R., Mayorov A.Yu., Kuraeva T.L., Peterkova V.A. et al. Methodological recommendations “Algorithms for specialized medical care for patients with diabetes mellitus” (edited by Dedov I.I., Shestakova M.V.). Fifth edition, Moscow, 2011.
Operation. Features and contraindications
A few words about the features of the operations themselves. Today, such operations are performed in an open way, i.e. through an incision on the anterior abdominal wall. In the near future, similar operations will be performed in our Center laparoscopically, i.e. through several punctures, without large incisions. Such operations are already being done around the world. Patients are examined on an outpatient basis and are usually admitted to the hospital on the eve of surgery. All operations are performed under general anesthesia. Patients begin to walk the next day after surgery. Postoperative hospital stay is 5-6 days.
What are the risks of the operation itself and are there any contraindications to surgical treatment? Of course, any surgical intervention carries an element of risk. These operations are quite complex. In addition, patients suffering from diabetes have an increased risk of inflammatory complications and their wound healing processes are slowed down. At the same time, speaking about the risk in general, we first of all emphasize that the risk of developing deadly complications with uncorrected diabetes (heart attack, stroke, kidney failure, blindness, etc.) is significantly higher than the risk of surgery.
Contraindications to performing such operations are severe irreversible changes in vital organs (heart, liver, lungs, kidneys). We consider smoking and alcoholism as serious contraindications. Patients who have inflammatory changes in the esophagus, stomach and duodenum need short preparation.
Does the patient need additional treatment after surgery? After gastric or biliopancreatic bypass surgery, lifelong intake of mineral and vitamin supplements is necessary. This is a condition for the operation. In the first 2-3 months after surgery, antiulcer drugs are sometimes prescribed prophylactically. If there is a need for treatment with glucose-lowering drugs, they may be needed only in the first days of the postoperative period.
Directions for use and doses
In adults
CYTOFLAVIN® is used only intravenously in a dilution of 100–200 ml of 5–10% dextrose solution or 0.9% sodium chloride solution. The injection rate is 3–4 ml/min. 1. In case of cerebral infarction, the drug is administered as early as possible from the onset of the disease in a volume of 10 ml per injection with an interval of 8–12 hours for 10 days. In severe cases of the disease, the single dose is increased to 20 ml. 2. For the consequences of cerebrovascular diseases (cerebral infarction, cerebral atherosclerosis), the drug is administered in a volume of 10 ml per injection once a day for 10 days. 3. For toxic and hypoxic encephalopathy, the drug is administered in a volume of 10 ml per injection twice a day every 8–12 hours for 5 days. In a comatose state - in a volume of 20 ml per injection diluted with 200 ml of dextrose solution. In case of post-anesthesia depression of consciousness - once in the same doses. In the treatment of hypoxic encephalopathy during cardiac surgery using artificial circulation, 20 ml of the drug diluted with 200 ml of a 5% dextrose solution is administered 3 days before surgery, on the day of surgery, and for 3 days after surgery. 4. For the prevention of cognitive disorders after extensive surgical interventions in elderly patients, the drug is administered in a volume of 20 ml per injection diluted with 200 ml of 0.9% sodium chloride solution. The course of treatment is 7 days according to the following scheme: first administration - one day before surgery; the second is intraoperative administration after induction of anesthesia (start of infusion within 30 minutes from the start of the operation), then within 5 days after the operation. In the future, it is recommended to use the drug "CYTOFLAVIN® enteric-coated tablets" 2 tablets 2 times a day with an interval between doses of 8-10 hours for 25 days.
In children (including premature infants)
in the neonatal period with cerebral ischemia, the daily dose of CYTOFLAVIN® is 2 ml/kg. The calculated daily dose of the drug is administered intravenously (slowly) after dilution in a 5% or 10% dextrose solution (in a ratio of at least 1:5). The time of the first administration is the first 12 hours after birth; The optimal time to start therapy is the first 2 hours of life. It is recommended to administer the prepared solution using an infusion pump at a rate of 1 to 4 ml/h, ensuring a uniform flow of the drug into the bloodstream throughout the day, depending on the calculated daily volume of solutions for basic therapy, the patient’s hemodynamic state and acid-base parameters. The course of treatment averages 5 days.
Practice will not let you lie
How new is the formulation of this issue in our country? How is it going in the world? The operations in question are used to treat obesity quite widely throughout the world. That is why we talk about their proven effectiveness in type II diabetes. That is why bariatric surgeons, those who treat obesity surgically, widely discuss the use of surgical data for type II diabetes mellitus, regardless of the degree of excess body weight. In recent years, a number of publications have been presented, the results of which are truly impressive. In Russia, the first biliopancreatic bypass operation, the main purpose of which was the treatment of type 2 diabetes mellitus and at the same time hypercholesterolemia, was performed by the author of these lines in 1999, and its results were published in the country and abroad. Unfortunately, gastric bypass and biliopancreatic bypass operations are little known in our country, but the Center for Endosurgery and Lithotripsy already has some experience in their use. It is likely that surgical treatment methods will in the near future mark new prospects for the treatment of type II diabetes mellitus.