The historical name for this condition is apoplexy. This is what the Roman surgeon Galen called a hemorrhagic stroke, denoting the main external signs of the disease - a sudden loss of consciousness, after which the person changed forever. Today, doctors know for sure that a vessel ruptures in the cranial cavity, blood flows out, after which up to 70% of patients die. However, the development of neuroimaging technologies, as well as the capabilities of neurosurgery, lead to the fact that the number of deaths from stroke is decreasing, and in some cases, rehabilitation sufficient for a good life is possible.
Why do blood vessels rupture?
The main cause is arterial hypertension, especially if untreated or during breaks in taking antihypertensive drugs. The vessels physically cannot withstand the pressure that blood exerts on their walls. A vessel breaks through at the site of thinning or damage, this happens in the presence of an atherosclerotic plaque, congenital aneurysms, head injuries, the use of certain medications that prevent blood clotting, tumors and encephalitis. Another important cause of rupture is arteriovenous malformations, when small arterial and venous vessels do not end in capillaries, but are intertwined into one large ball. Such congenital pathology can be detected during a preventive examination. If a person knows about it, he behaves more carefully and avoids unnecessary risks.
Nature has protected the brain as much as possible from damage, providing it with a mass of protective and backup systems. At a young age they work, but in the second half of life they don’t always work. Therefore, it is advisable that people at risk undergo an annual examination by a neurologist.
At CELT you can get advice from a neurologist.
- Initial consultation – 4,000
- Repeated consultation – 2,500
Make an appointment
The following people are at high risk of developing hemorrhagic stroke:
- hypertensive patients, they need to take medications daily;
- overweight people - the body grows approximately 1 kilometer of blood vessels per 1 kg of excess weight;
- people with high levels of cholesterol, namely low-density lipoproteins, which form atherosclerotic plaques on the vascular wall;
- people who eat insufficient amounts of protein and do not have the “building material” for complete tissue repair;
- those under chronic stress, often suffering from physical or emotional stress;
- alcohol abusers and smokers;
- those suffering from diabetes or heart disease;
- suffering from chronic infections that destroy the vascular wall - lupus erythematosus, vasculitis;
- people who constantly take medications to reduce blood viscosity;
- having direct relatives who died from cerebral hemorrhage.
Useful facts
An intracerebral bruise may have a liquid texture or consist of coagulated blood. In certain situations, in addition, detritus may be present in the bruise in much smaller quantities. The total volume of liquid can reach 100 ml. The increase in the diameter of the hematoma continues for several hours after the onset of hemorrhage, and during a failure of the coagulation function much longer. After the formation of the lesion, the process of compression of adjacent tissues begins, which subsequently leads to necrosis.
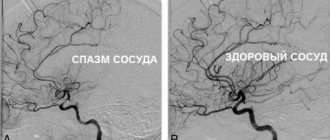
In addition, the occurrence of such a phenomenon affects the increase in the level of intracranial pressure and becomes a source of swelling. It can cause displacement of certain structures and the formation of dislocation syndrome if the bruise is large. Bleeding can lead to a reflex spasm and the onset of ischemia, first affecting the nearby cavities. Ischemia is considered an additional damaging cause, which shapes the progression of abnormal deformations far beyond the boundaries of the formation. According to average statistical information, in almost 14% of cases there is a breakthrough into the ventricles and hemorrhage.
How does a hemorrhagic stroke occur?
Vascular rupture can occur at any time of the day. This is usually preceded by physical or emotional stress. The person suddenly falls, sometimes with a loud cry, and loses consciousness.
Approximately 30% of patients have warning signs that develop within a few minutes to several days. On the eve of a rupture of blood vessels, there may be severe headaches - ones that the person has never experienced. There is a feeling of a rush and a sharp reddening of the face. Sometimes the sensations of numbness in the limbs, muscle weakness, and facial asymmetry appear.
The main symptoms of hemorrhagic stroke are:
| Contralateral hemiplegia | The nerve pathways intersect, so the paralysis is located on the side opposite to the hemorrhage. During a stroke, the left arm and leg stop moving in the right hemisphere, and the right ones in the left hemisphere. |
| Contralateral hemianesthesia | In paralyzed limbs, sensitivity disappears on the side opposite to the rupture. |
| Aphasia | Loss of speech occurs when the dominant (dominant) hemisphere is damaged. For right-handers - right, for left-handers - left. |
| Spatial hemiagnosia with damage to the non-dominant hemisphere | If a right-hander's left hemisphere is affected, and a left-hander's right hemisphere is affected, then the person behaves as if half of the real space does not exist for him. A person does not realize that he has two halves of the body, that food can be eaten from the entire plate, and not from half. Half of everything that is located around a person is not perceived by him. |
| Facial asymmetry | One half of the face does not receive innervation and cannot contract. One nasolabial fold is smoothed out, the smile becomes one-sided, the tongue deviates to one side, water and food flow out of the mouth. |
From the moment these symptoms appear, there is only 3 hours to help the person as much as possible. After 3 (sometimes 6) hours, irreversible changes will occur, then nothing can be corrected.
Symptoms of intracerebral hematoma
Symptoms are especially pronounced and observed in full in elderly patients.
When an intracerebral hematoma forms, a clinical picture with the following symptoms can be observed:
- General cerebral symptoms. Often, patients seek help in a clear consciousness, less often - while in moderate stupor.
- Mental disorders. Such symptoms directly depend on the age of the patient. An elderly body is weaker and more vulnerable.
- Epileptic seizures. They are rare, sometimes accompanied by convulsions, but the patient is often conscious.
- Headache. It appears when the head is tilted and provokes unconscious facial expressions. The pain is often local in nature and is observed at the site of hematoma formation.
- Asthenia.
- Shell symptoms. Rigidity of the neck muscles is observed.
- Hypertensive changes in the fundus as a consequence of high intracranial pressure.
- Disorders of the musculoskeletal system.
- Disorders of the speech apparatus and swallowing function.
- Decreased muscle tone, the presence of tremor, hypomimia, stiffness of movements or their slowness.
- A voluntary or reflexive upward gaze indicates that the trunk is being pinched.
- Lucid interval". It can be long lasting – from several hours to several years.
Our doctors
Novikova Larisa Vaganovna
Neuropathologist, Candidate of Medical Sciences, doctor of the highest category
Experience 39 years
Make an appointment
Pankov Alexander Rostislavovich
Neurologist
40 years of experience
Make an appointment
Types of strokes
Depending on which part of the brain the hemorrhage occurred, there are 4 types of stroke:
- Intracerebral or parenchymal, when the spilled blood saturates an area of the brain. In turn, they also have their division into:
- hemispheric, when an area of the hemispheres is affected;
- subcortical, located under the cortical (gray) matter of the brain;
- hemorrhage in the cerebellum, where the balance centers are located;
- hemorrhage in the brain stem, where the respiratory center and the area that is responsible for the functioning of the heart and maintaining the pressure in the vessels necessary to support life are located.
- Subarachnoid (bleeding into the space between the meninges).
- Ventricular (hemorrhage into the ventricle of the brain).
- Mixed: ventricular-parenchymal, subarachnoid-parenchymal, parenchymal-ventricular-subarachnoid and so on.
Survival depends not only on the location of the vessel rupture, but also on how much blood was released. Small hemorrhages are considered to be those in which from 1 to 20 ml are poured out, medium - from 20 to 50 ml, large - more than 50 ml. The greater the amount of blood shed, the more severe the consequences. A stroke is almost always accompanied by disturbances in cardiac activity, breathing and swallowing, oculomotor disturbances, and changes in the size of the pupils.
Classification of intracerebral hematomas
All intracerebral hematomas can be classified according to different criteria.
According to etiology, the most common intracerebral hematomas are:
- aneurysmal;
- hypertension;
- tumor, traumatic;
- iatrogenic;
- for craniocerebral imbalances, intoxications, etc.
By frequency, cerebral hematomas are divided into:
- Primary (formed immediately after injury).
- Secondary or delayed (hematoma formation occurs after a day or longer). They are much more difficult to tolerate than the first one. Have more side effects.
Based on their location, intracerebral hematomas are divided into:
- Supratentorial (frontal, fronto-temporal, fronto-parietal, fronto-parieto-temporal, fronto-parieto-occipito-temporal, parieto-occipital, parieto-temporal, temporal).
- Infratentorial (stem and cerebellar). Brainstem hematomas are the most dangerous and usually incompatible with life, cerebellar hematomas are the rarest type, accounting for approximately 6-8% of all intracerebral hematomas.
- Multiple.
Regarding the surface of the cerebral hemispheres and cerebellum, hematomas are:
- basal;
- parabasal;
- sagittal;
- parasagittal;
- convexital;
- parasagittal-convexital.
Classification of hematomas by lateralization:
- right-sided;
- left-sided;
- bilateral.
By volume, intracerebral hematomas are:
- small (up to 50 cm3);
- medium (50-100);
- large (more than 100).
They are classified according to the volume of hematomas for the practical purpose of determining treatment tactics.
Based on computed tomography readings, hematomas are also classified according to their density:
- hypodense;
- hyperdense;
- heterodense;
- isodense.
Based on their structure, intracerebral hematomas are divided into:
- single-chamber;
- two-chamber;
- multi-chamber.
Regarding the clinical phase there are:
- compensation;
- subcompensation;
- moderate decompensation;
- severe decompensation.
Cerebral hematomas are also grouped according to the progression of the clinical picture:
- gradual;
- fast;
- avalanche-like;
- undulating;
- progressive.
Additional Research
MRI of the brain
- Cost: 14,000 rub.
More details
The initial diagnosis is established after examination by a neurologist, but instrumental diagnostics are always required to clarify the boundaries of the lesion. The most informative method is computed tomography, which allows a good examination of the brain matter. MRI is used for the same purpose if there is time for it.
Angiography gives excellent results, this is a study of blood vessels with contrast. It identifies malformations, dissections (dissections) and other vascular pathology. The important thing is that this study can be conducted in healthy people at risk. This is the best prevention of stroke if research is supplemented with treatment.
Lumbar puncture is used for diagnostic and therapeutic purposes.
Features of treatment
Treatment of hemorrhagic stroke today is more in the purview of neurosurgeons than neurologists. The blood has already been shed, and the possibilities of medical assistance are limited. Removal of an intracerebral hematoma can save lives and maintain an acceptable level of health. Surgical removal is more successful the earlier it is performed. Optimally, the patient should be operated on on the first or, in extreme cases, on the second day after the incident.
The main intervention is aspiration (suction) of the hematoma and clipping of the aneurysm. It is only possible when the artery is in an accessible place. There is no way to help with an aneurysm deep in the medulla. In a typical case, the blood is aspirated, a clip is placed at the base of the aneurysm, and the aneurysm is isolated from the bloodstream.
Malformations are excised whenever possible. These are complex operations that require not only the skill of a specialist, but also first-class equipment.
Mechanism of occurrence
The described disease can manifest itself due to the following factors:
Rupture of vascular walls due to injury (for example, head injury, concussion, etc.).- Post-traumatic diapedesis at the point of contusion.
- Deformation of an aneurysm or arterial-venous malformation due to tumor formation (stroke, hypertension, atherosclerosis, etc.).
- Changes in the rheological functions of blood vessels during hemophilia, leukemia, painful conditions of the liver and others.
How to help a stroke victim?
Recovery largely depends on how the people around the patient behave. First of all, you need to call an ambulance, and until it arrives, try not to move the person. You need to place a cushion or pillow under the shoulders and head, carefully turn the person on the right side, and place a basin or bag in case of vomiting. It is advisable to measure blood pressure. Anti-pressure pills should not be given before the ambulance arrives: there is a possibility of a sharp drop in blood pressure. Only specially trained medical personnel know the rules for lowering blood pressure when it rises above 150/100 mmHg. If respiratory depression occurs, you need to start resuscitation - chest compressions, mouth-to-mouth breathing.
The best prevention is timely treatment of hypertension, atherosclerosis, identification of malformations and aneurysms before they rupture.
Our neurologists see patients every day, and every patient at the clinic can find out their risk for developing a hemorrhagic stroke. Visit your doctor while you still have time.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Prognosis of intracerebral hematoma
The prognosis of intracerebral hematoma depends on many factors:
- localization of education;
- volume;
- density;
- condition and age of the patient;
- presence of concomitant risk factors for treatment complications (high blood pressure, obesity, chronic and infectious diseases).
With adequate treatment, timely treatment of the patient and identification of the formation, the prognosis can be favorable, even for elderly patients.
The patient should be informed of the possible risks of complications despite a favorable prognosis. Among the complications of treatment of intracerebral hematomas can be noted: hemorrhage, recurrence of hematoma, cerebral edema, formation of postoperative hematoma.
Conservative treatment regulates the rate of brain decompression, so complications are less common than with surgical treatment. Fatal outcomes from treatment of intracerebral hematomas are not frequent (less than 1%) and occur mainly in elderly patients due to pulmonary artery thrombus.