Why is pressure inside the skull needed, why can it be elevated, and how does this indicator relate to blood pressure? What are the norms and when is blood pressure dangerous to health and life, how to feel it and how to reduce it, let's talk with an expert ALENA PARETSKAYA
Pathophysiologist, immunologist, WHO expert POLINA PETROSYAN Neurologist at SM-Clinic, specialist in cerebrovascular diseases and headaches
What is intracranial pressure
The brain is surrounded by a fluid called cerebrospinal fluid, which nourishes and protects nerve cells.
Cerebrospinal fluid is continuously produced and flows away from the skull, thereby maintaining a constant pressure. This is intracranial pressure - a certain force that puts pressure on the brain and the walls of the skull. This pressure is changed in mmHg.
Art., and normally it is from 10 to 15 mm. If it is higher, this is a reason to be wary, and if the pressure exceeds 25 mm Hg. Art., this can be dangerous for brain function. If the value is more than 35 mmHg. Art. Severe and irreversible changes in the brain are possible - such situations are considered critical.
Reasons for the development of the disorder
The factor that provokes an increase in pressure is the impaired outflow of cerebrospinal fluid from the brain. Normally, it occupies about 10% of its total volume, performing various functions, which include:
- protection of the brain from trauma - in the event of an impact or fall, the cerebrospinal fluid will “soften” the contact of the cranial bones and delicate tissues;
- it is also with the movement of cerebrospinal fluid that toxins and decay products are removed from the brain;
- Finally, it ensures that the correct electrolyte-water balance is maintained.
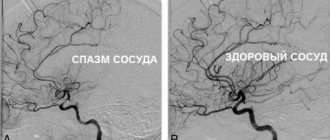
The most common causes of ICP include metabolic disorders that provoke insufficient flow of fluid into the blood, as well as spasm of the vessels through which the cerebrospinal fluid moves. In addition, oxygen deprivation of the brain, excess fluid in the body, obesity, severe intoxication, and inflammation of the brain can also provoke ICP. The presence of tumors in the body - benign or malignant - can also cause disruption of the outflow of cerebrospinal fluid.
If the outflow of cerebrospinal fluid from the intracranial space is disrupted for any reason, this provokes the accumulation of its excess volume and an increase in pressure. At the same time, in both a child and an adult patient, an increase in intracranial pressure to more than 30 mm Hg can lead to the development of irreversible changes in tissues and, as a consequence, disability and even death.
Causes of intracranial pressure in adults
Increased intracranial pressure (ICP) is not an independent disease, but a syndrome.
Doctors sometimes call it intracranial hypertension. Pressure inside the brain (similar to arterial pressure) fluctuates when the head is tilted back and forth or to the sides, during physical activity or sneezing. But it can increase to serious numbers in case of pathologies, and there are many of them. “ICP (intracranial pressure) occurs as a result of an increase in the volume of intracranial contents (cerebrospinal fluid or cerebrospinal fluid), tissue fluid, or the appearance of foreign tissue (tumors, cysts, brain abscess), says neurologist Polina Petrosyan.
In addition, the causes of increased ICP may be:
- traumatic brain injury;
- tumor;
- intracerebral hemorrhage;
- neuroinfections (encephalitis, meningitis).
“The cause may also be long-term use of drugs from the group of hormonal contraceptives, corticosteroids or antibiotics,” adds Dr. Polina Petrosyan.
Pressure increases because fluid is either produced in excess (for example, due to an infection that has spread to the brain or its membranes), or because fluid flows out of the skull through special pathways less easily. If volumetric processes develop in the cranial cavity (for example, a tumor grows or hemorrhage occurs), there will be less space for fluid, and its pressure will also increase.
Gymnastic exercises
Therapeutic exercises for intracranial hypertension can become an alternative to certain drugs during conservative therapy, as well as a prophylactic agent to reduce attacks of the disease. Depending on the cause and stage of the pathological process, the specialist selects techniques that have lowering properties of brain pressure and alleviate the condition of patients.
A specially developed set of gymnastic exercises is aimed at normalizing ICP, relieving pain and increasing blood circulation.
The most effective exercises to reduce high cerebral pressure:
- We alternately tilt our heads to the right and left sides, forward, backward, pulling the chin to the chest. Next, we slowly rotate the head in any direction. Movements should be smooth, the number of repetitions of exercise elements should be an average of 20 times.
- Grasp the lower occipital region with both hands so that the thumbs are located on the neck muscles, at the level of the earlobe. Then, for 15 minutes, fingers should be rubbed over the muscles from top to bottom to improve the outflow of cerebrospinal fluid. After the exercise, heaviness in the temporal and occipital areas decreases.
- Grasp a small round stick with both hands and place it behind your head. For 15 minutes, with light pressure, we move the stick over the neck muscles and lower occipital region.
Important! In the first days of the gymnastics course, painful sensations may occur due to tension in the neck muscles, but subsequently, when performing the exercises, the discomfort will disappear.
Symptoms of intracranial pressure in adults
In many cases, a slight increase in ICP may not manifest itself for a long time. If the pressure rises sharply or high enough, the following symptoms may occur:
- headache - it can be pressing or bursting, usually occurs in the morning, this pain has no clear localization, it can be felt in different parts of the skull;
- nausea and vomiting - they usually occur at the peak of the headache;
- drowsiness, malaise, general poor health;
- memory impairment (forgetfulness), attention disorders, problems with thinking;
- changes in the autonomic nervous system – surges in blood pressure, slow pulse, increased sweating;
- visual impairment up to complete blindness.
Symptoms may come on suddenly or develop gradually over weeks or months.
Signs of pathology
Changes in intracranial pressure affect the general condition of the patient. This is often preceded by injuries or blows to the head, complications during childbirth, and diseases of the meninges. In this case, the patient cannot lead a normal lifestyle, and the symptoms of increased or decreased ICP are not relieved by taking medications. Such patients are treated in a hospital setting. It is also impossible not to notice pathological changes in this indicator in children. In addition, in the absence of a reason, the pressure cannot increase or decrease and stop at a critical level for the child - serious reasons are required for this.
The physiological basis of painful sensations with an increase or decrease in pressure, as well as other symptoms, is an insufficient supply of blood to the brain and various disorders of its circulation. If fluid is retained in the vessels and cerebral ventricles, the tissues are under constant pressure, which can provoke gradual necrosis (death) of cells. Hypoxia (insufficient oxygen supply) and nutrient deficiency are also observed - this causes disturbances in brain activity or loss of reflexes, depending on the location of the damaged area of brain tissue.
With high blood pressure
High blood pressure is manifested by a pronounced set of symptoms that affect all vital processes. They may be combined with additional clinical signs characteristic of a particular disease. The symptom complex indicating increased ICP includes:
- painful sensations in the head, which are pressing in nature and spread to all areas, often occur immediately after waking up and intensify during the day;
- sleep disorders, insomnia;
- ineffectiveness of standard drugs against headaches;
- nausea and vomiting, decreased heart rate;
- a sharp decrease in vision, inability to focus on small objects for a long time, deterioration of memory and concentration.
For headaches that occur as a result of serious pathologies of intracranial pressure, the patient remains in bed. During physical activity, attacks of dizziness, loss of consciousness, and memory loss may occur. Also, peripheral vision disorders periodically appear, the appearance of dark spots and “floaters” in the field of vision is a consequence of permanent fluid pressure on the optic nerve. With exacerbation, the situation worsens, normal reflex responses to stimuli may partially disappear.
In children, behavioral problems and hyperactivity are often associated with increased intracranial pressure. However, these diagnoses may not be related. Increased ICP in infants is indicated by symptoms such as bulging fontanel, rapid increase in head circumference, and divergence of the bones of the skull. Another alarming symptom is the overgrowth of the fontanel too slowly. If these signs appear in combination with general apathy or excitability, poor sleep, lack of innate reflexes, this may indicate pathological fluid pressure inside the skull.
At low pressure
Reduced intracranial pressure can also be determined by clinical signs. The symptoms are not as pronounced as when this indicator increases, but also affect the patient’s well-being and performance. If the pressure inside the skull is not normal, this leads to the following consequences:
- headaches, which are especially worse when raising the head;
- frequent mood swings, lethargy, apathy, irritability;
- simultaneous decrease in blood pressure if the syndrome is caused by a general lack of fluid in the body;
- headaches, dizziness, fainting may occur after minor physical exertion;
- decreased visual acuity, appearance of dark spots before the eyes;
- nausea, abdominal pain;
- Possible pain in the heart area that spreads to the chest.
First aid for a sharp decrease in intracranial pressure is to take the correct position. Lying on your back with your head down makes the outflow of fluid difficult, so the pressure is partially restored. This factor may also have diagnostic significance - when you raise your head and sit or stand, the pain intensifies, and lying on your back it decreases slightly.
Diagnostics
It is extremely difficult to suspect an increase in ICP based on external signs.
The doctor must know all the complaints and those facts from life that preceded the symptoms. This could be a hypertensive crisis, head injury, severe infection, kidney or liver problems. In order to confirm the diagnosis, the doctor will prescribe a number of studies to the patient: CT or MRI of the brain to evaluate the structure of all tissues of the skull, note the condition of the ventricles of the brain where cerebrospinal fluid accumulates;
- echoencephaloscopy to determine brain function;
- Ultrasound of the brain (mainly in children through the fontanelle);
- examination of the condition of the fundus by an ophthalmologist;
- spinal cord puncture with measurement of the pressure of the escaping cerebrospinal fluid (the cerebrospinal fluid itself is taken for analysis).
Which doctor should I contact?
If symptoms of liquor-hypertensive syndrome appear, you should contact a neurologist. An experienced specialist can be seen at the medical office by appointment. You can make an appointment by phone @. The doctor will see you at a time convenient for the patient.
The neurologist from the SmartMed clinic has many years of experience in treating noise in the head of various origins, including those caused by intracranial hypertension. To determine the cause of poor health, the doctor will conduct a visual examination.
The examination begins with a study of the patient's complaints and neurological testing. It is important for the doctor to know the person’s medical history, conditions of occurrence, frequency and intensity of noise in the head.
Increased VChP cannot be determined by external signs
The doctor must prescribe instrumental research methods:
- Spinal or lumbar puncture. Designed not only for studying cerebrospinal fluid, but also for measuring intracranial pressure. The procedure is invasive and involves inserting a puncture needle into the spinal canal and then connecting a pressure gauge.
- MRI of the head. Allows you to identify the causes and signs of intracranial hypertension: cerebral edema, vascular thrombosis, enlargement or narrowing of the cerebral ventricles, cysts, tumors, hematomas, hemorrhages. The study is the most informative and safe. In medical MRI of the head, it is carried out on a new ultra-precise Siemens Symphony 1.5 Tesla tomograph, thanks to which it is possible to obtain a highly accurate 3D image. The examination takes no more than 15 minutes, no special preparation is required.
- Ultrasound of the head. Used for children of the first year of life. The study is carried out through an open fontanel.
- Ultrasound of the vessels supplying the brain. Allows you to assess the condition of the arteries, as well as the direction, speed and intensity of blood flow in them, to identify the main vascular disorders that can cause high ICP and noise in the head.
- Electroencephalography. Designed to study the electrical activity of the brain, it allows you to identify areas of irritation of various brain structures.
Additionally, the neurologist may prescribe a consultation with an ophthalmologist. Papilledema, which can be detected during fundus examination, is a sure sign of increased ICP. If necessary, other highly specialized specialists are involved in the examination: a neurosurgeon, an oncologist.
Important! The reliability of the examination for intracranial pressure depends on the technical parameters of the diagnostic equipment and the qualifications of the diagnostician.
Modern methods of treatment
In some cases, the patient does not require treatment; he is observed and treated for the underlying disease, which caused the increase in ICP.
If it is necessary to treat pathology, two approaches are used - conservative and surgical.
Conservative interventions are carried out for those patients whose ICP elevation is chronic and there is no significant deterioration of the condition over time. The basis of treatment is drugs that have a diuretic effect, which reduce the volume of fluid in the head. The specific medicine is determined by the level of pressure and the situation. In severe and acute processes, osmotic diuretics (mannitol) are used, in chronic cases - furosemide, hydrochlorothiazide, spironalactone. While taking them, you need to drink a potassium preparation - Asparkam, Potassium orotate, Panangin.
Surgical methods for treating increased ICP depend on the stage and severity of the disease. In acute situations, craniotomy is performed to reduce fluid pressure on the brain and drain excess fluid. Special shunts (tubes) are installed as planned, which drain fluid from the brain into the abdominal cavity.
Traditional methods of correction
What should patients do to independently stabilize ICP? You can lower the level of cranial pressure at home using folk recipes. It is recommended to use herbs and plants that have sedative and vasodilating properties. However, non-traditional treatment is used for chronic intracranial hypertension in remission.
The following non-traditional remedies will help reduce intracranial pressure:
- Lavender infusion. 1 tbsp. l. place dry raw materials in a container and pour 500 ml of boiling water. Leave for an hour, then remove the sediment. Take 3 times a day, 1 tbsp. l. Therapeutic course - 3 weeks.
- Decoction of bay leaves. To prepare, you need to prepare several leaves, which are filled with 1.5 liters of water. Bring the mixture to a boil and use as inhalation. Course - 14 days.
- Clover tincture. Dried flowers of the plant should be taken in an amount equal to 0.5 liters of container. Fill with alcohol so that the liquid covers the dry raw materials. Leave for 2 weeks, then filter, take the tincture 3 times a day, 1 tsp. The duration of the course is 30 days.
Birch sap has a diuretic effect, due to which it normalizes ICP parameters
Treats intracranial hypertension with a mixture based on honey:
- To prepare, take 150 ml of fresh lemon juice, 350 g. liquid flower honey and 2 cloves of chopped garlic.
- Mix the ingredients thoroughly.
- Leave the mixture in a dark, cool place for 10 days.
- Take in the morning, in the evening 60 minutes after a meal at a dose of 1 tsp.
To quickly eliminate headaches accompanying a hypertensive attack, use lavender essential oil. A few drops of the product should be applied to the temporal area and rubbed in with light massage movements for several minutes.
Prevention of intracranial pressure in adults at home
Prevention of increased ICP is the prevention of various diseases affecting the cranial cavity.
This includes protection against infections that can affect the brain - vaccination against meningococcal and hemophilus influenzae infections, influenza vaccination. It is also necessary to treat various pathologies that can affect brain function. General recommendations are simple:
- follow a daily routine and lead the healthiest lifestyle possible;
- avoid head injuries;
- protect yourself from stress and nervous overload;
- Get enough sleep.
Make an appointment with a neurologist
Experienced specialists conduct consultations in the neurological department of the private Multidisciplinary Medical Hospital. Get rid of unpleasant symptoms and prevent complications caused by increased intracranial pressure by completing a course of treatment.
Information on prices for initial and repeated paid appointments with a neurologist is presented on our website. You can make an appointment with a specialist at a convenient time by phone or using the online form on our website.
Moscow, st. Krasnodarskaya, house. 52, bldg. 2
+7
We work on weekdays and weekends from 8.00 to 21.00
Measurement principles
The principles of measuring intracranial pressure differ significantly from measuring blood pressure. To date, there are no devices for quickly measuring ICP. Since the structural elements located in the cranium occupy a certain volume of the cranial cavity, determined by its parameters, therefore it cannot change. Due to the fact that the volume of the cranial cavity cannot be changed, the ratio of brain structures is constant.
Measuring intracranial pressure is difficult because there are not enough indirect parameters by which to determine the pressure in the cranium. Depending on the diagnosis, age and functional state of the body, visual examination methods or modern research methods are used to diagnose patients, which make it possible to use equipment to determine the reasons that provoked changes in brain pressure. Invasive techniques through surgery are used to establish clear pressure values.
Lumbar puncture
If hardware diagnostics do not help identify the cause of the disease, the neurologist prescribes a lumbar puncture - a lumbar puncture. It is an invasive procedure performed to obtain a sample of cerebrospinal fluid. The procedure can be performed for diagnostic and therapeutic purposes. During diagnosis, a lumbar puncture helps to more accurately determine the degree of pressure increase. For therapeutic purposes, the procedure is performed for benign intracranial hypertension to improve the patient’s condition.
NORMOTENSIVE HYDROCEPHALUS
Normal pressure hydrocephalus (NPH) is associated with impaired CSF absorption, and dilatation of the cerebral ventricles develops in the presence of normal intracranial pressure.
EPIDEMIOLOGY
The prevalence of NG is 1-2 cases per 1,000,000 people. In the practice of a neurologist specializing in patients with extrapyramidal diseases, as a rule, no more than a dozen patients are recorded per year. This type of hydrocephalus is more common in older people. The condition should be excluded in persons over 60 years of age with a combination of cognitive impairment (dementia), pelvic organ dysfunction (usually urinary incontinence) and walking impairment (lower body parkinsonism) - the Hakim-Adams triad. Due to the fact that in a significant proportion of cases, bypass surgery in the early stages leads to improvement in walking, it is important to suspect and confirm this condition in a timely manner.
CLINIC
The structure of cognitive impairment is dominated by frontal-subcortical disorders: decreased activity, apathy, and behavioral disorders. Walking disorders have been described as magnetic gait, gait apraxia, and frontal ataxia. Patients experience the greatest difficulty when starting to walk. The area of support is increased, the length and height of the step is reduced, the smoothness of movements is impaired, and there is a progressive slowdown in walking with each step. Patients always have postural instability; often, upon questioning, you can find out that there have been falls before.
DIFFERENTIAL DIAGNOSIS
However, other diseases with cognitive and motor impairments may have a similar pattern of impairments. When carrying out differential diagnosis, the following are considered: vascular dementia (discirculatory encephalopathy stage III), Parkinson's disease with dementia and dementia with Lewy bodies, Alzheimer's disease. The main diagnostic method is MRI of the brain. The examination reveals the expansion of the lateral ventricles, the rounded shape of their anterior horns, and the smoothness of the relief of the cerebral cortex. It is important to use the Evans ventricular-hemispheric index, which is the ratio of the distance between the most distant points of the anterior horns of the lateral ventricles to the largest internal diameter of the skull. Ventriculomegaly is diagnosed if the index exceeds 0.31. NG is characterized by changes in the periventricular white matter, similar to leukoaraiosis (see above). Their severity correlates with the degree of cognitive impairment].
Figure 2 MRI signs of cerebral atrophy (A) in Alzheimer's disease and (B) normal pressure hydrocephalus
At first glance, the images are quite similar, but the image on the right shows the rounded shape of the horns of the lateral ventricles and the smoothness of the sulci of the cerebral hemispheres.
Figure 3 Gliotic and atrophic changes after traumatic brain injury, replacement hydrocephalus
Ways to lower blood pressure permanently
In the initial stages of hypertension, the first step is to prescribe therapy with non-drug methods associated with changing the patient’s lifestyle:
- To give up smoking. Tobacco smoking is recognized as one of the main risk factors for the development of arterial hypertension. One cigarette smoked leads to a sharp increase in blood pressure and increased heart rate.
- Normalization of body weight. Numerous studies have proven that losing weight in overweight or obese patients leads to stabilization of blood pressure.
- Increasing physical activity. Regular dynamic physical exercises in the air for 50-40 minutes at least 4 times a week are recommended.
- Reducing salt intake to 5 g/day.
- Limit alcohol consumption.
- Compliance with the work and rest regime.
- Balanced diet. Increasing the proportion of plant foods and low-fat dairy products in the diet.
While blood pressure is slightly elevated, following the principles of a healthy lifestyle can stabilize blood pressure at a normal level with minimal drug support or even without drugs at all.
As the disease progresses, hypertension is treated using medications from various pharmacological groups to achieve a reduction in blood pressure to normal levels.
First aid at home for symptoms of high blood pressure:
- It is necessary to reassure the patient and create conditions for physical and emotional peace.
- Provide a flow of fresh air into the room.
- Breathing exercises help to quickly reduce pressure: take a deep breath, hold your breath for 10 seconds, exhale noisily through your mouth, then take short breaths in and out through your mouth for 2 minutes.
- Give the patient Corvalol to drink: dissolve 30 drops in 100 ml of water.
If attacks recur repeatedly, you should consult a doctor to find out the cause of the increase in pressure.
Invasive methods for monitoring ICP
To accurately diagnose cerebral hypertension, invasive methods are used; they are carried out through surgery, when a special sensor is inserted into the cranial cavity through a burr hole. The procedure is carried out in a hospital equipped with the necessary equipment. During the examination, there is a high risk of injury to the brain and spinal cord, so this method is used in extreme situations that require immediate confirmation of the diagnosis.
You can measure cerebral pressure using an invasive method if you have the following indications:
- intracranial hemorrhage;
- stroke;
- hydrocephalus;
- meningitis of an infectious nature;
- posthypoxic encephalopathy.
Important! Thanks to cerebral pressure monitoring, it is possible to coordinate perfusion pressure, which reflects the effectiveness of cerebral hemodynamics, and also makes it possible to evaluate the results of decongestant therapy.
Depending on the location of the drainage system, indicators are measured using the following techniques:
- intraventricular;
- intraparenchymal;
- subdural;
- subarachnoid.
Intraventricular technique
The earliest method of cranial pressure control. The main advantage is the possibility of drainage of cerebrospinal fluid and direct endolumbar administration of medications.
External ventricular drainage
The procedure for measuring ventricular pressure is carried out using a strain gauge. The technique is easy to interpret the results and does not require the use of expensive equipment. This procedure is not only diagnostic, but also therapeutic, since it allows you to control cranial pressure by draining the cerebrospinal fluid.
Parenchema method
During the study, the sensor is installed through the trefination hole in the parenchyma of the medulla to a depth of no more than 2.5 cm. This method is preferable, since the data obtained during the study are more consistent with the readings of intraventricular pressure.
Epidural technique
Direct technique for monitoring ICP using sensors. The technique is based on the introduction of special devices into the cerebral ventricles, which make it possible to measure cerebral pressure values to set accurate pressure.
The following examination systems are used:
- Microsensory. The tensor apparatus is introduced into the required brain area, after which the information converted into electrical signals is reflected on the monitor.
- Fiber optic. Additionally, a drainage system is connected, which allows a moderate reduction in cerebral pressure values.
- Pneumatic. A catheter with a latex balloon filled with air is installed.