The level of antibodies to the thyroglobulin protein is normally insignificant, since they are formed as a reaction of the body’s immune system to contact with thyroglobulin. Typically, this colloidal protein is located in the enclosed space of the follicle and does not provoke the formation of antibodies. The reason for exceeding the norm for antibodies to thyroglobulin may be damage to the follicle and the release of a significant amount of thyroglobulin into the blood. Then, in the results of tests for antibodies to thyroglobulin, increased values are recorded.
Diseases of the thyroid gland that require testing for elevated thyroglobulin
An analysis for elevated thyroglobulin is done in the following cases:
• For thyroid carcinoma. But it should be remembered that only a third of patients with thyroid cancer have an increase in the concentration of this protein;
• For the purpose of early detection of metastases or relapses of tumors after surgical treatment has already been performed. A relapse of both malignant and benign thyroid tumors may be indicated by increased thyroglobulin in the blood plasma;
• Determination of the effectiveness of radioactive iodine therapy for the metastatic process in thyroid tumors;
• For the diagnosis of artificial thyrotoxicosis (against the background of hormone replacement treatment);
• Thyroglobulin, the norm of which is increased, is assessed in children to determine the origin of congenital hyperfunction of the thyroid gland;
• As a tumor marker and a means for assessing the effectiveness of treatment of thyroid tumors;
• To assess the activity of thyroiditis or confirm previous inflammation of the thyroid gland in the next 2 years;
• For mass studies in conditions of iodine deficiency.
References
- Histology (introduction to pathology) / ed. E.G. Ulumbekova, Yu.A. Chelysheva, 1997. - P. 147-163.
- Clinical guidelines for thyroid cancer - approved. Ministry of Health of Russia, 2021. - 47 p.
- Oncology / ed. acad. RAMS V.I. Chissova and prof. S.L. Daryalova, 2007. - pp. 83-99.
- Arthur, C., Hall, J. Textbook of Medical Physiology. 13th Edition, 2015. - P. 1042-1055.
- Kumar, V., Abbas, A., Fausto, N. et al. Robbins and Cotran Pathologic Basis of Disease, 2014. - 1464 p.
When are antibodies to thyroglobulin elevated?
• If antibodies to thyroid peroxidase and thyroglobulin are elevated, Hashimoto's chronic thyroiditis may be the cause.
• Antibodies to thyroglobulin are elevated during autoimmune inflammation of the gland tissue - thyroiditis.
• Hypothyroidism without a clearly identified cause, or idiopathic hypothyroidism, can also be manifested by increased antibodies in the blood.
• Antibodies to thyroglobulin can also be elevated in diffuse toxic goiter (Graves' disease).
Thyroglobulin - what is it?
It is a protein that is a precursor to thyroid hormones in the human body.
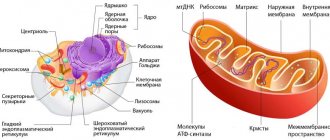
The synthesis of thyroid hormones T3 and T4 in the human body does not occur immediately, but through the formation of thyroglobulin. This complex protein consists of amino acid residues tyrosine and iodine. In fact, thyroglobulin is a chain of almost ready-made molecules of the hormone thyroxine (T4), which only needs to be “cut” before the hormone is released into the blood. The protein is stored in the lumen of the thyroid follicles as a kind of “reserve”. The cells of the gland form single-layer spherical clusters, the internal lumen of which is filled with a viscous transparent gel - a colloid containing a large amount of thyroglobulin. It is stored in the lumen of the follicle until it is required by the body - then its molecule is captured by thyrocytes (thyroid cells) and passed through them, cutting into residues of two tyrosine molecules and four iodine atoms in each residue. Such “chopped” thyroglobulin is nothing more than a ready-made molecule of the main thyroid hormone, thyroxine, which is released into the blood.
Recommendation 63
- Patients with low and average risk who have undergone surgical removal of the thyroid gland or adjuvant therapy, who do not have evidence of disease progression based on the results of ultrasound examination of the neck area, need to determine thyroglobulin (TG) during the period of 6-18 months during Levothyroxine therapy using sensitive methods (<0.2 ng/ml) or after TG stimulation to confirm the absence of disease progression.
(Strong recommendation, moderate quality of evidence)
- Repeating the TG stimulation test is not recommended for low- and intermediate-risk patients with an excellent response to therapy.
(Weak recommendation, low quality of evidence)
- A TG stimulation test may be performed in patients with an indeterminate, biochemically incomplete or structurally incomplete response to treatment, in patients with a spontaneous decrease in TG values on thyroid hormone therapy over a long period of time in order to review/reassess the response to therapy.
(Weak recommendation, low quality of evidence)
- In the future, a stimulation test is not required for patients without signs of the disease, because the benefit of its use in this population is small. The use of sensitive methods for determining serum TG helps to avoid the use of this test in low-risk patients on Levothyroxine therapy with TG levels below 0.1-0.2 ng/ml.
Serum TG measurement and clinical utility
- Determination of serum TG levels is an important method for monitoring patients with residual or recurrent disease.
- Most laboratories now use immunometric methods to measure serum TG levels, it is important to note that these methods are calibrated against international standards (CRM-457).
- Despite improvements in the standardization of TG analysis methods, there are often still differences between the results of different methods. This led to the recommendation that patient measurements should be performed using the same method.
- Variability in methods for measuring TG Ab levels can lead to false-negative antibody levels, which in turn leads to undetectable TG in serum.
- However, radioimmunological methods for measuring TG are not widely used and are less sensitive to the influence of antibodies than immunometric methods.
Most of the data are from studies using 1 ng/mL functional sensitivity methods. The functional sensitivity of many modern methods is ≤0.1 ng/ml. High sensitivity ensures reliable measurement of TG in patients on thyroid hormone therapy, even compared to the stimulation test.
- Since TSH stimulation increases basal serum TG by 5-10-fold, significant serum TG levels (>1-2 ng/ml) detected after stimulation using a method with a functional sensitivity of 0.5-1 ng/ml may be predicted in patients on Levothyroxine therapy without stimulation, using a highly sensitive method for measuring TG, provided that the TG level is above 0.2 ng/ml.
The highest degrees of sensitivity of serum TG were observed with the abolition of thyroid hormones or with stimulation using recombinant human thyrotropin. Serum TG measurements obtained during TSH suppression may be insufficient in identifying patients with relatively small amounts of residual tumor.
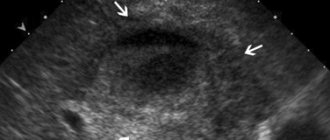
- Residual tumor tissue is often located in the neck, and ultrasound examination in such patients has great diagnostic value for recognizing or excluding neoplastic processes, even if it is impossible to determine serum TG.
- Conversely, even measurement of TG levels during TSH stimulation may be unreliable for patients with a clinically noticeable tumor due to the presence of antibodies to TG or, less commonly, due to insufficient production and secretion of immunoreactive TG by tumor cells.
- The TG level should be assessed in light of the likelihood of detecting clinically significant residual tumor.
- An aggressive and poorly differentiated tumor may be present even despite low basal or stimulated TG levels; in contrast, minimal increases in TG after stimulation may be observed in patients at low risk of clinically significant disease progression.
- However, a stimulated serum TG level of <0.5-1.0 ng/ml in the absence of anti-TG antibodies provides a 98%-99.5% probability of developing remission.
- Measurement of stimulated TG does not require a repeat test in most cases; detection of an undetectably low basal serum TG and absence of signs of disease progression according to ultrasound is sufficient. However, 0.5% to 0.3% of patients may experience clinical or biochemical relapse despite stimulated TG levels <0.5 ng/mL.
Initial follow-up of low-risk patients (approximately 85% of postoperative patients) undergoing total or subtotal thyroidectomy and radioiodine treatment should be based primarily on stimulated TG and neck ultrasound.
- However, a TG method with a functional sensitivity of 0.1–0.2 ng/mL may reduce the need for stimulation testing. In one study using this method: serum TG levels on Levothyroxine <0.1 ng/ml were rarely (2%) associated with an increase in stimulated TG >2 ng/ml;
- however, 42% of patients had a basal TG level with TSH suppression >0.1 ng/mL, but only one patient had residual tumor.
- Annual determination of serum TG levels during levothyroxine therapy with periodic ultrasound examination of the neck are sufficient methods to detect relapse without further need for stimulated TG testing in patients with serum TG <0.2-0.3 ng/ml on thyroid hormone therapy.
Approximately 20% of patients in remission with a serum TG level <1 ng/ml while receiving suppressive doses of levothyroxine have a stimulated TG level >2 ng/ml 12 months after surgery or radioactive iodine therapy.
- In this cohort of patients: in 1/3 with a persistent course or relapse of the disease, an increase in the level of serum TG is detected,
- and in 2/3 – without progression of the disease, the level of stimulated serum TG is stable or gradually decreasing
- It appears that stimulated TG levels above 2 ng/mL are highly sensitive for identifying patients with persistent tumors.
[C7] AT to TG
- The presence of anti-TG antibodies, which is found in approximately 25% of those with thyroid cancer and 10% of the general population, will underestimate serum TG levels when measured by immunometric methods.
- Serum antibodies to TG should be measured in combination with serum TG by an immunometric method.
- Although standardization of International Reference Preparation 65/93 methods has been recommended, wide-ranging differences in the results of different methods and their analytical sensitivities remain.
- Anti-TG antibodies may increase transiently after surgery due to an apparent immune reaction to the operation itself, and may also increase after ablative therapy.
- Anti-TG antibodies should be measured repeatedly if routine anti-TG antibody testing is negative in patients with surgically confirmed Hashimoto's thyroiditis. This may be useful when measuring anti-TG antibodies immediately after thyroidectomy and before ablation, as high levels may predict the likelihood of relapse in patients without Hashimoto's thyroiditis.
- Decreasing levels of antibodies to TG may indicate successful therapy.
The recent development of liquid chromatography-coupled mass spectrometry TG assays promises to be a more accurate method for measuring TG in the presence of anti-TG antibodies, but future studies will need to first validate this method in terms of functional sensitivity, correlation with immunoassays, and patient outcomes.
[R8] What is the role of TG measurement in patients not treated with radioactive iodine?
And the most important…
At the end of this short article, I would like to say that thyroglobulin is a highly specialized laboratory indicator that is used only in some selected situations. It should be used only for its intended purpose and not used where you can do without it. Elevated thyroglobulin
Blood tests aimlessly scare thousands of people every year, but for thousands of people every year,
the thyroglobulin level
gives hope for a normal life - it’s all just a matter of who prescribes the test, in what situations and how the results are then interpreted. The 3rd generation immunochemiluminescent laboratory of the Northwestern Endocrinology Center determines thyroglobulin with extreme accuracy, and the center’s specialists know very, very much about it, so if you suddenly have any questions or misunderstanding of your tests or your doctor’s tactics, come to us to the center for a consultation or re-analysis in order to remove all questions and understand how and where to move on.
Preparing the patient for the procedure and features of blood donation
In order for the research results to be accurate and reliable, simple rules should be followed. The patient can take a TG test 3 months after the end of surgical treatment. If a person was treated with radioactive iodine, he should wait at least six months to donate blood. If these deadlines are not met, the results of the study will be incorrect and there is a possibility that the possibility of relapse will be shown when in fact the harmful tumor does not develop.
When determining the level of iodine globulin, a test is carried out for antibodies to the protein. If a large number of antibodies are detected, the hormone level will be considered quite low. After stopping thyroxine for several weeks, the effectiveness of the manipulation will become more reliable, but the doctor must make sure that the patient does not have antibodies to the test hormone using special tests and diagnostics.
In order for the results of the study to be without distortion, blood should be donated on an empty stomach in the morning. 24 hours before the procedure, the patient should not engage in sports; 1.5-2 months before the procedure, it is prohibited to use medications containing iodine and hormones.
The manipulation is carried out in the treatment room. The patient sits on the couch and the nurse examines the veins in his arms. The patient's forearm is clamped with a special tourniquet, and the place where the needle will be inserted is lubricated with a cotton pad previously soaked in ethyl alcohol. The specialist pierces the vein with a hollow needle and begins collecting the biomaterial into a flask or other sterile container.
The resulting sample is placed in a test tube and a smear is made on the glass. The biomaterial can be sent to the laboratory, and the patient applies cotton wool with alcohol to the injection site and fixes it with a bandage on top. The patient should hold his hand tightly and not move it for 5 to 10 minutes to avoid bleeding and bruises on the skin.