Cancer of the antrum of the stomach is more common than other malignant neoplasms of this organ. It can be asymptomatic for a long time, so it is often diagnosed already at stage 4. It is no longer possible to carry out radical treatment in such a situation. Advanced cases can be prevented with regular gastroscopy.
- general information
- Reasons for development
- Symptoms of gastric antrum cancer
- Classification
- Localization and metastasis
- Diagnosis of gastric antrum cancer
- Treatment
- Complications and relapses
- Forecast
- Prevention
Reasons for development
The following factors lead to gastric antral cancer:
- Lifestyle - stress, weakness, bad habits, lack of routine, etc.
- The nature of the diet is an excess of table salt and carbohydrates, a lack of vitamins and microelements, rough food that injures the surface of the epithelium and promotes the colonization of the bacterium Helicobacter pylori on the mucous membranes of the duodenum and stomach.
- Infection with the bacterium Helicobacter pylori.
- Composition of consumed water. If it contains nitrates and nitrites, under the influence of microorganisms they are converted in the stomach into nitrosamines, which are powerful carcinogens.
- Endogenous causes - duodenogastric reflux, heredity, decreased local and humoral immune response, etc.
The process of carcinogenesis in the stomach is usually triggered by free radicals formed during inflammation. Therefore, cancer almost always occurs against the background of chronic pathology. Precancerous diseases include:
- adenomatous polyp-like growths (gastric adenomas);
- chronic ulcer;
- stomach operated for benign pathologies;
- chronic inflammation of various nature, including Ménétrier's disease and autoimmune gastritis type A.
Dysplasia of the mucous membrane plays a major role in the development of malignant neoplasms.
According to a number of studies, about 75-85% of cases of stomach cancer occur due to chronic gastritis.
How to treat
Arterial hyperemia is not treated in 85% of cases. In such a situation, intensive blood supply to tissues begins as a consequence of independent regeneration of damage. The cells of the stomach receive the necessary amount of oxygen and nutritional components, due to which metabolic processes are accelerated. As a result, cells begin to divide rapidly, and healthy tissues replace damaged structures. In the arterial form of the pathology, doctors only prescribe proper nutrition and help balance the diet.
In the remaining 25% of cases, active hyperemia, as well as venous blood filling, indicate the presence of gastritis. In case of inflammation of the mucous membrane, complex treatment is carried out. The patient must follow a strict diet, take antibiotics to suppress the growth of Helicobacter pylori and other medications to accelerate tissue regeneration. You are allowed to drink herbal infusions and eat honey.
Symptoms of gastric antrum cancer
Among the clinical symptoms accompanying malignant neoplasms of the stomach, several groups can be distinguished:
- general (asthenic syndrome, anemia);
- gastric (dyspeptic complaints, pain syndrome);
- associated with distant metastases (at stage 4) and characterized by damage to specific organs and structures.
According to the nature of the course, malignant tumors of the stomach have 3 clinical variants:
- latent (asymptomatic);
- painless;
- with pain syndrome.
At the initial stage, cancer can develop asymptomatically or be accompanied by a clinical underlying disease. Most patients (2/3) present with complaints typical of chronic gastritis. They experience periodic discomfort, a feeling of fullness in the stomach after eating, belching, heartburn, nausea, vomiting, bloating and other symptoms.
Sometimes the first sign of cancer is a palpable tumor in the stomach, which is typical for a latent form of the disease. As a rule, severe pain syndrome soon follows.
In order not to miss the development of malignant formation in the antrum, you should use the recommendations of A.I. Savitsky, who back in 1951 created a symptom complex of “small signs”. He stressed the importance that the initial manifestations of cancer must be assessed in totality.
This syndrome includes:
- Unexplained regular or constant weakness, rapid physical and mental fatigue, decreased performance.
- Unmotivated persistent loss of appetite, up to anorexia, with a predominant aversion to meat foods.
- Sudden loss of body weight.
- A systematic feeling of gastric discomfort, when periodically or constantly after eating there is a feeling of heaviness, fullness of the stomach, pain, as a result of which a person becomes picky in choosing food.
- Changes in the emotional background - the patient becomes withdrawn, alienated, loses interest in the environment, up to apathy and deep depression.
When a tumor of the antrum becomes infected, signs of intoxication of the body appear. If the gastric neoplasm is complicated by bleeding , typical symptoms will be observed - vomiting “coffee grounds”, tarry stools, tachycardia, severe weakness, dizziness, even fainting. When wall is perforated, sharp unbearable “dagger pains”, cold sweat, a sharp deterioration in general condition, and sometimes loss of consciousness will appear. Also, a tumor located in the antrum can completely block the exit from the stomach into the duodenum, which will lead to stagnation of food and the corresponding clinical picture - vomiting of eaten food, pronounced “heaviness” in the epigastrium, exhaustion, etc.
If cancer metastases have affected the liver, characteristic manifestations will be jaundice, itching, pain and discomfort in the right hypochondrium. With carcinomatosis, the main symptom will be ascites (accumulation of fluid in the abdominal cavity). Constipation and abdominal pain may indicate Schnitzler metastasis (tumor of the pouch of Douglas).
Tuberculosis of the oral mucosa
Tuberculosis of the oral mucosa occurs due to the introduction of Mycobacterium tuberculosis, also known as Mycobacterium tuberculosis. Simply put, Koch's wand. Tuberculosis of the oral mucosa is a manifestation of the main chronic disease – tuberculosis. In principle, the occurrence, manifestation, course and outcome of the disease depend on the general condition of the body, its reactivity and immunity.
The route of entry of Mycobacterium tuberculosis is simple. This is either endogenous penetration, that is, through the blood, lymph; or exogenously (airborne droplet route).
But the oral mucosa is not sensitive to this bacterium and is slightly susceptible. Therefore, the introduction of Mycobacterium tuberculosis is possible only through the oral mucosa, which is damaged, inflamed, and already has foci of inflammation: erythema, ulcers. That is, the entrance gates for oral tuberculosis can be:
- Pathological pockets;
- Gums over erupting teeth;
- Wound after tooth extraction;
- Damaged epithelium, regardless of the nature of the injury.
Tuberculosis as a chronic disease can be primary and secondary. So, primary tuberculosis of the oral mucosa most often occurs in children or infants (since Koch’s bacillus can be transmitted through the milk of cows), or in schoolchildren aged 8 to 12 years, whose families have people suffering from an open form of tuberculosis.
Tuberculosis of the oral mucosa can be of several forms: it is either tuberculous lupus, or miliary ulcerative tuberculosis, or in the form of a tuberculous ulcer. These two forms of tuberculosis of the oral mucosa are the most common.
There is also another form of tuberculosis of the oral mucosa, which is very rare - “Cold abscess,” in other words, these are isolated, separate tuberculous gummas.
Tuberculous ulcer - Clinical picture
The incubation period for the occurrence of a tuberculous ulcer in tuberculosis of the oral mucosa lasts from 8 to 30 days. After this period of time, an ulcer appears at the site of the introduction of Mycobacterium tuberculosis. The size of the ulcer in tuberculosis of the oral mucosa reaches up to 1.5 cm in diameter. The edges of a tuberculous ulcer are uneven, undermined, and can be dense or soft. The ulcer itself in tuberculosis of the oral mucosa is shallow, but painful. The bottom of a tuberculous ulcer is granular.
The shape of the ulcer is not always oval; for example, if the manifestation of tuberculosis is on the transitional fold or tongue, most likely the shape of the tuberculous ulcer will be slit-like. It is clear that the reaction of the lymph nodes in tuberculosis of the oral mucosa will be positive. Lymph nodes increase in size, become denser, at first they are mobile, but the more time passes from the day of infection, the more strongly they adhere not only to each other, but also to the skin. Moreover, over time, the lymph nodes can fester and open.
Tuberculous lupus
Tuberculous lupus is a phenomenon that manifests itself primarily on the skin, most often the skin of the face. But there are also combined forms, when in addition to the facial skin, the mucous membrane of the oral cavity is also involved in the process. The favorite place for this form of tuberculosis of the oral mucosa is the gums and soft palate. So what to look for on the gums and soft palate if tuberculosis is suspected? The answer is obvious - tuberculous tubercles!
Tuberculous lupus - Clinical picture
The clinical picture of tuberculous lupus is quite clear. There is a tuberculous tubercle on the soft palate. The size of the tuberculous tubercle is small, often compared to the head of a pin. We looked and assessed the color – yellowish-pink. Needs to be palpated. The tubercular tubercle will be soft.
Often with tuberculous lupus, tuberculous tubercles are located in groups on the soft palate. That is, they are susceptible to merging and rapid disintegration with exposure of the ulcerative surface. The ulcerative surface in tuberculous lupus is bright red, bleeds easily, covered with a yellow-gray coating, which causes pain when trying to remove it.
On the gums, tuberculous lupus also manifests itself as tubercles, but these tubercles quickly turn into ulcers and spread to the interdental papillae and the edge of the gums. All the same signs as with the appearance of tubercles on the mucous membrane of the soft palate.
Milliary - ulcerative tuberculosis - Clinical form
Milliary ulcerative tuberculosis is the most common form of secondary tuberculosis in children. Often occurs in children with open form of tuberculosis. That is, when you cough, sputum is released, in the sputum - Mycobacterium tuberculosis, which easily penetrates through the damaged oral mucosa.
The clinical picture of milliary ulcerative tuberculosis is characterized by the fact that red dots appear on the mucous membrane of the cheeks, on the back and lateral surfaces of the tongue, and on the soft palate. In this form of tuberculosis of the oral mucosa, these red dots are slightly convex and rise above the normal mucous membrane. However, this stage changes quickly and is often not even noticeable to the eye. But these red dots ulcerate and an ulcer occurs. Often these ulcers quickly grow to the periphery and can merge with each other. An ulcer in the milliary-ulcerative form of tuberculosis of the oral mucosa is irregularly shaped, with undermined, uneven edges, the bottom can be granular, the mucous membrane around the ulcers is swollen and hyperemic.
Treatment of tuberculosis of the oral mucosa
Treatment of tuberculosis of the oral mucosa, of course, should first of all be aimed at treating general tuberculosis, that is, in a special medical institution. The dentist must identify such patients and organize clinical observation.
Classification
Malignant tumors of the antrum of the stomach are classified according to:
- Histological structure - mucinous adenocarcinoma, medullary cancer with lymphoid stroma, undifferentiated form, etc.
- According to Lauren - intestinal, diffuse, mixed, unclassified types.
- The macroscopic criterion is early and advanced cancer.
- Japanese classification based on lymphatic drainage pathways and damage to regional lymph nodes.
- International TNM system with definition of process stage.
Other classifications are used less frequently.
Prevention measures
To avoid irritation and inflammatory plethora of the mucous membrane, doctors recommend adhering to the following preventive measures:
- stop smoking;
- limit the intake of alcohol-containing drinks and strong coffee;
- Healthy food;
- avoid stress;
- See a doctor on time and treat chronic somatic diseases.
It is also necessary to exercise and not overwork. This will help boost immunity and ensure protection and rapid restoration of the mucous membrane.
Localization and metastasis
Malignant neoplasms can be located in any part of the stomach. If its antral region is affected, the tumor may be localized closer or further from the pylorus, which will determine the clinical course and surgical tactics.
In antral cancer, metastasis occurs in several ways:
- Along the wall of the stomach with invasion into the surrounding healthy mucous membrane.
- With blood flow to distant organs - liver, lungs, bones, pancreas, etc.
- Lymphogenously to regional lymph nodes.
- With the help of implantation of cancer cells in the peritoneum - carcinomatosis.
Lymphogenous metastasis is more common. In case of antral cancer, tumor “dropouts” in the lymph nodes are found in half of the patients.
Therapeutic measures
For people interested in how to restore the gastric mucosa, it is important to know that when this disease is diagnosed, in most cases no treatment is prescribed, since it is believed that the body independently fights the problem through self-regeneration. During this process, accelerated metabolism occurs, which causes the process of tissue self-healing to enter an active stage.
This condition is a positive phenomenon in the development of arterial hyperemia. In some cases, doctors create an additional flow of blood fluid to stimulate regenerative processes and speed up recovery. If you are interested in how to restore the gastric mucosa in case of other pathologies, you need to contact your doctor with this question.
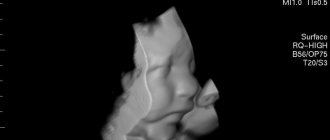
Diagnosis of gastric antrum cancer
Diagnostic measures for stomach tumors always begin with a survey, history taking and examination of the patient. The doctor finds out whether the patient had relatives who died of cancer, whether the person has bad habits, chronic diseases of the digestive system, etc. Further diagnosis has two objectives: to establish the presence and spread of the tumor process in the antrum of the stomach and to detect distant metastases.
The survey plan includes:
- laboratory tests;
- endoscopic examination of the esophagus, stomach, duodenum, with targeted sampling of material from 6-8 different points;
- analysis of gastric juice;
- X-ray methods.
Additionally, the following may be prescribed: ultrasound of the stomach, CT scan of the abdominal cavity and chest, skeletal scintigraphy, blood for tumor markers (CEA, CA19.9, CA72.4 and SCC) and other studies.
Providing assistance with hyperemia of the gastric mucosa
If unpleasant symptoms appear in the stomach area due to hyperemia of its mucous membrane, it is necessary to contact a specialist as soon as possible to prescribe the correct treatment. But if you can’t see a doctor right away, you can temporarily use a few simple tips.
Ensure complete rest by taking a lying position. Drink a glass of clean, cool water. Take No-shpa or another antispasmodic drug. Apply a heating pad with ice to the epigastric area. Follow a strict diet by reviewing your diet.
Remember! It is strictly forbidden to apply heat to the stomach, take painkillers and continue physical activity. All this can provoke various complications of the disease, the main one of which is gastric bleeding.
Treatment
For malignant tumors of the gastrointestinal tract, surgical intervention is considered radical treatment. With surgical removal of stage 1 and 2 gastric tumors, in most cases it is possible to achieve a complete cure.
“Early cancer” (in situ or T1a-N0M0) is predominantly removed using an endoscopic approach, with dissection of the submucosal layer. The tumor must be highly or moderately differentiated, not exceed more than 2 cm in diameter, and not have ulceration. In other cases, the question of the operation, its volume and access is decided individually, taking into account many factors. The main ones are:
- stage of the process, form of growth of the primary neoplasm, local spread of cancer;
- the degree of damage to regional lymph nodes;
- the general condition of the patient, his readiness and “ability” to undergo surgery, with the removal of part or all of the stomach;
- the presence of distant metastases.
When the tumor is localized in the pyloroantral region, subtotal distal gastrectomy is indicated in most cases. The scope of radical surgery for cancer is removal of the tumor “in a single block”, with a distance of 5-7 cm from healthy tissue, depending on the type of growth, with mandatory lymph node dissection. If a gastrectomy is performed (the entire organ is removed), an important step is subsequent reconstruction to restore the possibility of enteral nutrition. Also, for malignant tumors of the stomach, palliative surgical interventions (bypass anastomoses, elimination of metastases, etc.) can be performed.
Surgery is often combined with radiation and/or drug therapy. The latter can be prescribed before, during or after surgical manipulation. Radiation therapy is carried out either intraoperatively or after surgery. The combined method is used most often, as it ensures the removal of the main focus and “kills” existing and potential “screenings” of cancer in the lymph nodes and other organs and tissues of the body.
In some cases, PDT (photodynamic therapy) and targeted drugs are used. Also, all patients with gastric tumors receive adequate symptomatic treatment and rehabilitation measures.
Diagnostic measures
If any suspicious symptoms appear (for example, nausea, bloating, heartburn, belching, pain), it is very important to visit a gastroenterologist in a timely manner. One of the main methods for studying the condition of the mucosa is a procedure called esophagogastroduodenoscopy. It is performed using an endoscope - a special probe with a camera at one end to view the internal state.
Using this method, you can accurately assess the condition of the body and the internal walls of the stomach, take a piece of tissue for analysis (biopsy), visualize the presence of a pathological process, and prescribe the correct course of therapy.
A competent specialist will easily determine the presence of pathology in hyperemic epithelium, since healthy tissue looks shiny and produces mucus normally. During the examination, when inflated with air, the folds are straightened, the surface is smooth, the epithelial cover is intact and clean, without wounds or ulcerations. The color is pink, there may be a yellowish coating.
As the disease develops, the symptoms worsen, redness of the epithelial layer appears, the folds increase, do not straighten when inflated, and swelling is observed.
Complications and relapses
After removal of a tumor from the stomach, especially during major operations, there is a high risk of developing subsequent complications. These include:
- cancer recurrence;
- bleeding and anemia;
- purulent-septic complications, up to peritonitis;
- failure of the gastric stump or created anastomoses;
- hypoxia;
- pancreatic necrosis;
- intestinal obstruction;
- thromboembolism;
- myocardial infarction, pneumonia and other complications from the surgery and anesthesia.
After operations for gastrointestinal cancer, the risk of death remains high, especially with voluminous, technically complex interventions, for example, after complete removal of the stomach - from 11 to 25%. The level of training of the surgeon and anesthesiologist has a great influence on the incidence of complications and mortality.
Recommendations for nutrition in pathology
If hyperemic mucosa is detected, the patient is advised to follow a diet. Substances that irritate the mucous membrane should be excluded from the diet: spicy, salty, sour, fatty foods, smoked meats and marinades, alcohol, strong coffee. Fried foods are not recommended. For heat treatment, food should be boiled or steamed.
In the diet you can use:
- chicken, rabbit, turkey, veal, low-fat sea fish;
- a small amount of vegetable fats;
- skim milk, cottage cheese;
- non-acidic fruits and vegetables;
- cereals (rice, oatmeal, buckwheat);
- eggs, no more than 1 per day;
- wheat bread 1-2 grades, crackers.
Meals should be fractional (5-6 times a day), small portions. It is also necessary to observe the temperature regime; the dishes should not be too hot or cold. The optimal temperature is between 15 and 60 degrees Celsius.