Authors of the article: Candidate of Medical Sciences O.Yu. Ermolaev
Obstetrician-gynecologist, specialist in proper nutrition during pregnancy E.K. Ermolaeva
Preterm birth is birth between 22 and 37 weeks of pregnancy.
Premature birth is one of the most common causes of childhood death and illness today.
Premature babies are often weakened, they may have breathing problems (in some cases, respiratory arrest), problems with feeding and maintaining body temperature.
In premature babies, diseases of the respiratory system and gastrointestinal tract occur more often and recur (recur many times), and mental or physical disabilities are more often identified.
The above personal family and social problems determine the importance of taking the threat of miscarriage and premature birth seriously.
| 3D profile photo of a fetus at 33 weeks |
- What is premature birth, threat of miscarriage?
- Why do they arise?
- What to do?
- Why lie down?
- What will happen if you don't lie down?
- How does the child feel? Is he hurt?
- Symptoms (signs) of threatened miscarriage, threatened premature birth
- Signs of ruptured membranes
- What to do if the membranes rupture?
Conditions in which there is a risk for a successful pregnancy are given the COMMON NAME “threat of miscarriage” or “THREAT of premature birth”.
The term “threatened miscarriage” is usually used when the pregnancy is less than 22 weeks.
The term “threat of preterm birth” is used between 22 and 37 weeks of pregnancy.
Causes of premature birth
- The cause of premature birth and the threat of miscarriage is psycho-emotional STRESS of the pregnant woman and/or fetus, FEAR.
- A common cause of premature birth and threatened miscarriage is inadequate physical activity (physical stress). Pregnancy is NOT THE TIME for RECORDS! Long walking (more than 20 minutes continuously), running, jumping, long jump, jumping rope, extreme sports, carrying bags, buckets, lifting and carrying a child and objects weighing more than 3 kg are not advisable. NOT DESIRED during pregnancy participation in general cleaning, performing work with a bent torso and “squatting”, long-term (more than 20 minutes continuously) standing.
- The cause of premature birth and the threat of miscarriage in the early stages of pregnancy is placental or decidual (due to abruption of the placenta or mucous membrane of the uterine cavity) BLEEDING.
- A serious cause of premature birth and the threat of miscarriage in early pregnancy is INFLAMMATION in the decidual tissue (endometritis during pregnancy), amnionitis (inflammatory reaction in the amniotic fluid), chorionitis (inflammation of the fetal membrane, “fetal membrane”).
- One of the causes of premature birth (birth before term) is wearing shoes with HEELS more than 3 cm. Wearing high-heeled shoes changes the angle of the pelvis, making the gait unstable. Unsteady gait is compensated by increased tone (compensatory tension) of the muscles of the back, legs, abdomen and uterus! The pregnant uterus actively participates in balancing the torso!
- The cause of premature birth and the threat of termination of pregnancy can be a SHARP movement, getting up from a chair, or falling. A sharp change in body position causes a protective tone - protective tension of the uterus.
- HOT WEATHER. According to statistics, the threat of miscarriage and premature birth (birth before term) are significantly more likely to occur in hot weather due to changes in vascular tone.
Timing of the threat of pregnancy, timing of the threat of miscarriage
The threat of miscarriage most often occurs during
5-6 weeks of pregnancy 7-8 weeks of pregnancy 10-12 weeks of pregnancy 15-16 weeks of pregnancy 20-21 weeks of pregnancy 24-25 weeks of pregnancy 26-28 weeks of pregnancy 30-31 weeks of pregnancy 32-34 weeks of pregnancy
During these periods of pregnancy, PHYSIOLOGICALLY (provided for by the natural characteristics of human physiology), the tone of the uterus increases significantly and there is a threat of miscarriage, the threat of termination of pregnancy, and the threat of premature birth.
Why is it necessary to lie down when there is a threat of miscarriage or a threat of premature birth?
The uterus is a muscular organ consisting of multidirectional muscle fibers that make up a single muscle.
Thus, the cervix and the body of the uterus are a single muscle. A protective increase in tone (PROTECTIVE SPAS) of the cervix protects the uterus from opening and at the same time, due to the painful sensation, ALLOWS a woman to RECOGNIZE the wrongness of the actions she has committed (or is performing).
The HORIZONTAL POSITION can significantly reduce the load on the cervix and, in most cases, contributes to the natural normalization of uterine tone.
Taking medications aimed at reducing the tone of the uterus has a similar effect.
However, when moving to a vertical position, the cervix, relaxed by the drug, cannot fully perform the retaining function!
THE RISK OF MISCARRIOR (premature birth) when the body is in an upright position while taking medications that relax the uterus increases sharply.
JUST LIE! And strictly follow your doctor’s recommendations!
A protective INCREASE in the TONE of the uterus is a natural PROTECTIVE REACTION aimed at preserving the offspring. You need to LIE!
How does a baby feel when there is a threat of premature birth?
We can only guess the answer to this question based on physiological data.
A pregnant woman and her fetus share a common circulatory system. Stress hormones (cortisol, adrenaline, prolactin), entering the general bloodstream, cause certain reactions from the central nervous system (brain and spinal cord), muscular system and other organs and systems.
If a pregnant woman is scared, experiencing pain, uncertainty about the future, her heartbeat and breathing become more frequent. The child may experience similar emotions and physiological reactions: FEAR, pain, tachycardia (rapid HEARTBEAT).
Increased uterine tone fixes the fetus and LIMITS its freedom of movement. Restriction of freedom of movement can cause some discomfort in the fetus.
When do symptoms appear?
Oddly enough, the first week of pregnancy is determined by the date of the last menstruation.
Your last period counts as the first week of pregnancy, even if you weren't actually pregnant yet. The approximate date of birth is calculated from the first day of the last menstruation.
Taking a home pregnancy test is the most affordable and easiest way to find out if you are pregnant. Remember that home pregnancy tests measure the level of a hormone called human chorionic gonadotropin (hCG) in the urine, and there is usually less of it in the urine than in the blood.
The test gives the most accurate results starting from the moment of missed menstruation.
A menstrual cycle is considered delayed if your period does not start 5 or more days after the day it was expected to start.
However, it is worth remembering that even the day after the expected delay, more than a third of women give a negative result from such home tests, and if you take the test too early, the result may be negative, even if you are already pregnant. You can do another test at home after a couple of days to get a more accurate result.
Symptoms of threatened miscarriage, signs of premature birth:
A pregnant woman and her husband MUST KNOW the symptoms of threatened miscarriage and signs of premature birth!
- A symptom of a threatened miscarriage and a sign of premature birth is a dull, ACHING PAIN in the lumbar spine (LOWER). The pain does not stop (does not disappear) spontaneously (spontaneously) within 10 MINUTES or intensifies.
- A symptom of a threatened miscarriage and a sign of premature birth is aching pain in the lower abdomen, AS WITH MENSTRUATION.
- A symptom of a threatened miscarriage and a sign of premature labor are cramps (CONTRACTS) in the lower abdomen. Spasms (contractions) in the lower abdomen can be of varying strength and duration in primiparous and multiparous women. The feeling of pain is also very subjective and depends on the moral readiness for childbirth, the contractility of the uterus, the content of microelements in the woman’s body (in particular, calcium, potassium, magnesium and phosphorus), etc. IMPORTANT that when there is a threat of premature birth, the STRENGTH of contractions DO NOT weaken (do not change) or increase; The DURATION (time) of the contraction DOES NOT SHORTEN (does not change) or increase; and the frequency of contractions does not change or increases.
- A sign of premature birth is PRESSURE in the VAGINA, the sensation of a foreign body, something preventing you from walking.
- A sign of premature birth is a feeling of the urge to defecate, pressure on the rectum with the desire to empty the intestines.
- A sign of premature labor is the appearance of thin, clear vaginal discharge.
- A sign of premature birth is the expulsion of a mucous plug, amniotic fluid, or the appearance of pink (scarlet) discharge from the genital tract before 38 weeks of pregnancy.
Every healthy pregnant woman, starting from 32 weeks of pregnancy, may periodically experience short-term, cramping, mild PAIN (the uterus “comes to tone”).
Short-term pain (harbingers of labor) is associated with the preparation of the uterus for childbirth - “working out the interaction” of muscles and nerve receptors (nerve endings).
But if the pain is aching or cramping in nature or occurs more often than 4-5 times within an hour, you are probably going into labor. In some cases, prenatal contractions may not be accompanied by pain.
If you think you're going into labor, don't panic, lie on your left side and COUNT THE NUMBER OF CONTRACTIONS. If you experience 5 or more contractions within an hour, CALL your doctor.
If you begin to leak clear water or other fluid from your genital tract, TELL your doctor. The doctor will tell you what to do next.
Perhaps you have increased uterine tone.
There may be individual characteristics of your pregnancy.
In this case, the doctor will advise you to LIMIT physical activity, temporarily abstain from sexual intercourse, REST more, limit productive activity or stop working, visit the doctor more often and, possibly, prescribe medications that reduce the tone of the uterus and normalize the state of the nervous system.
It is important to call or visit your doctor PROMPTLY if you experience these symptoms.
Consulting an obstetrician-gynecologist will REDUCE the RISK of premature birth.
There are no two women who gave birth the same way, just as there are no two identical births for the same woman.
Don’t take everything that other women tell you about their personal experience as absolute truth and instructions to follow.
ASK your obstetrician-gynecologist any QUESTIONS you are interested in. You will receive an objective, competent answer based on the observations and experience of generations of obstetricians and gynecologists.
We are AT YOUR FULL DISPOSAL if you have any doubts or wishes.
Hypertension in pregnant women
High blood pressure during pregnancy
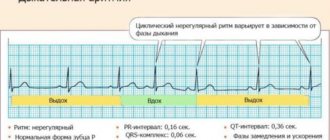
Changes in blood pressure (BP) in women during pregnancy are observed quite often, which can adversely affect the mother and fetus. Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work under increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure usually decreases slightly, due to the action of hormones. In later stages of pregnancy, as the fetus grows and the blood flow necessary for its nutrition increases, blood pressure may increase relative to physiological indicators before pregnancy. Arterial hypertension is said to exist if a pregnant woman’s blood pressure exceeds 140/90 mmHg. However, in women with low blood pressure before pregnancy, arterial hypertension may be present at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Why is high blood pressure dangerous during pregnancy?
High blood pressure during pregnancy poses a great danger to the mother and fetus. Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disrupted. Due to the lack of essential nutrients and oxygen, the growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can cause the development of a dangerous pregnancy complication - preeclampsia. Manifestations of preeclampsia can also include swelling, large weight gain, and the presence of protein in the urine. Very dangerous symptoms of preeclampsia are: headache, blurred vision (“floaters”, “veils” before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, and vomiting. Preeclampsia can provoke a serious complication - eclampsia. In this condition, the pregnant woman loses consciousness and experiences convulsions.
Register for pregnancy at the antenatal clinic as early as possible!
A very important feature of arterial hypertension during pregnancy is that often even with high blood pressure numbers the patient feels normal. High blood pressure is detected by chance, during the next visit to the antenatal clinic. The absence of clinical manifestations of high blood pressure does not exclude the development of dangerous complications.
In order to promptly identify unwanted abnormalities during pregnancy and prevent the development of complications in the mother and fetus, pregnant women need to regularly monitor their blood pressure. It is very important to register for pregnancy at the antenatal clinic in a timely manner. The doctor will promptly detect changes in blood pressure and prescribe optimal therapy to maintain normal blood pressure. If a woman had high blood pressure before pregnancy and she is taking medications, it is necessary to adjust the treatment and individually select medications that can be taken during pregnancy. To prevent high blood pressure, a pregnant woman should eat a healthy and balanced diet, follow a drinking regime, and monitor weight gain. The antenatal clinic doctor will also give the correct recommendations on these issues. A pregnant woman must follow the recommendations and not violate the prescribed therapy.
What to do if a pregnant woman has high blood pressure?
If a pregnant woman regularly monitors her blood pressure on her own and notices even a slight increase in it while feeling well, she should visit a doctor at the antenatal clinic as soon as possible (before the scheduled next appointment). Self-administration of medications in this case is strictly prohibited. Before visiting a doctor, you can lower your blood pressure by taking a mild sedative based on motherwort or valerian.
If necessary, you can consult with an obstetrician-gynecologist at the remote medical advisory console of the Emergency Medical Care Station named after. A.S. Puchkova, Moscow by phone.
When is it necessary to call an ambulance?
If blood pressure rises suddenly, or you feel unwell, urgent hospitalization is necessary, and it is advisable for the patient to immediately call an emergency medical team. Signs that should alert you are: headache, sensation of flashing dots or “floaters”, blurred vision, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with increased blood pressure. There may be a high level of convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness and convulsions are possible.
What to do before the ambulance arrives?
First of all, go to bed, if possible eliminate all unwanted irritants (turn off all sources of noise, close the curtains), do not leave the pregnant woman alone, as convulsions may occur and help will be needed. Give it a position with the head end raised. You can take blood pressure lowering medications prescribed by your doctor. If a woman has not previously taken antihypertensive drugs, then she should not take drugs on the advice of others.
If an attack of convulsions occurs, the pregnant woman should be laid on a flat surface, her head should be turned to the side (to prevent aspiration of vomit), protected from injury (covered with a blanket), and not physically restrained. After an attack, clean the mouth with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
The ambulance will arrive quickly and provide the necessary assistance. Hospitalization for this condition is mandatory. Only in a hospital is it possible to fully monitor the condition of the mother and child, complete therapy and determine a delivery plan.
We wish you health and happy motherhood!
Chief Specialist
in obstetrics and gynecology Arkhipova N.L.
Leading specialists in the management of complex pregnancies in the Southern Federal District
Ermolaeva Elvira Kadirovna is a well-known and recognized specialist in the North Caucasus in the field of diagnosis and treatment of miscarriage, miscarriage, recurrent miscarriage, management of pregnant women with thrombophilia, antiphospholipid syndrome (APS), systemic lupus erythematosus (SLE), uterine fibroids, management of pregnancy in young and older pregnant women (after 38 years), management of capricious pregnant women, management of pregnant women with excess body weight. A good obstetrician-gynecologist, a specialist in rational nutrition during pregnancy, a physiotherapist-resortologist, an experienced ultrasound doctor. Those who want to maintain their figure and successfully carry woman's pregnancy.
Ermolaev Oleg Yurievich Candidate of Medical Sciences, gynecologist-endocrinologist with 25 years of experience and successful experience in managing pregnancy in women with uterine prolapse, bicornuate uterus, saddle uterus and other malformations of the genital organs, managing pregnant women with livedo, thrombophilia and antiphospholipid syndrome (APS) , polycystic ovary syndrome. Management of multiple pregnancies, which require special attention and experience from doctors. Management of pregnancy after IVF, ICSI, after artificial insemination. Management of pregnant women with placental insufficiency. Management of pregnancy against the background of an IUD.
About the doctors of the Clinic in detail...
INTERNATIONAL RECOGNITION of the reputation and achievements of the Women's Health Resort Clinic in the development and implementation of effective and safe treatment methods and the quality of medical services provided is the AWARDING of the Women's Health Resort Clinic in Pyatigorsk with the SIQS International QUALITY CERTIFICATE in the field of medicine and healthcare. International Socratic Committee, Oxford, UK and Swiss Institute for Quality Standards, Zurich, SWITZERLAND. Read more…
Signs of ruptured membranes
The amniotic sac may rupture (rupture) in the CENTER just above the cervix. In the event of a central rupture of the amniotic sac, the amniotic fluid will come out in a hot stream (“gushing out like a bucket”), the waters will break.
In some cases, rupture of the membranes occurs above the internal os (opening) of the cervical canal. In the case of a high lateral rupture of the membranes, a SIGN OF RUPTURE of the membranes is the leakage of amniotic fluid in small portions (water leakage).
Often a pregnant woman feels that the pad or underwear has become wet, but cannot understand the reason - it is heavy discharge or rupture of water, leakage of amniotic fluid.
Increased vaginal discharge when coughing (“COUGH TEST”) is a sign of high rupture of the membranes and leakage of amniotic fluid.
Features of hypertension during pregnancy
Initially, it is worth finding out whether high blood pressure occurred at some point during pregnancy or before it. Many women have chronic hypertension from birth or from a young age, but they may not know it until the problem shows up during testing early in pregnancy.
If hypertension began before pregnancy or at the very beginning of pregnancy, then there is a chance that it will remain after childbirth. A gynecologist will help you cope with it with the help of medications. Often pregnant women are prescribed the drug “Dopegit 250 mg”.
Under no circumstances should you prescribe anything to yourself!
What to do if the membranes rupture?
RUPTURE of the amniotic sac always occurs unexpectedly and WITHOUT PAIN.
If amniotic fluid leaks or is suspected of leaking, you should NOTE THE TIME of the incident (“note the time”), PLACE a clean SHEET between your legs, take a horizontal position (LIE) and CALL your doctor.
If it is impossible to discuss the situation with your doctor, you should immediately CALL an ambulance.
This algorithm of actions in case of rupture of membranes is the only correct one, since after 12 hours the probability (risk) of infection of the fetus and the pregnant woman increases significantly, and the need arises to resolve the issue of the method of delivery (birth).
Considering that RUPTURE of the amniotic sac always occurs UNEXPECTEDLY, a pregnant woman must constantly CARRY with her an outpatient (exchange) card, a copy of her passport, and an insurance policy. YOU CAN have electronic COPIES of your exchange card, passport, insurance policy in your PHONE.
CHECK that your doctor's telephone number, obstetric hospital telephone number and emergency medical service telephone number are available in your phone book (in your phone).
If a critical situation arises, DO NOT rely only on yourself - LOUDLY, thinking about the child and WITHOUT HESITATION, seek help from others, warning about your pregnancy.
Starting from 24 weeks of pregnancy, it is very wise to form an “ALARM SUITCASE”. A complete list of things for the maternity hospital in detail...
The threat of miscarriage, the threat of premature birth, rupture of amniotic fluid are contraindications to driving: call an ambulance, DO NOT RISK the health of the baby, your life and the well-being of your family!
How to reduce the risk of hypertension
Choose foods high in omega-3 acids and fiber. They all improve heart health. What products contain these substances?
- Fish is rich in omega-3 and fatty acids. The choice is extremely large: tilapia, salmon, sardines, flounder and canned tuna. Add fish to your daily diet at least two to three times a week.
- Vegetables are another good choice, especially greens and leafy herbs, picked from your own garden or brought home from your parents' garden. To make your daily meals healthy, you need to include broccoli, cauliflower, spinach, celery, pumpkin, green beans, Brussels sprouts and bell peppers.
- Fresh fruit is a must on a pregnant woman’s menu. Most fruits contain a large amount of fiber, which no pregnant woman can do without. Eat apricots and apples with the skin on to improve the effect.
- Seeds and nuts that also provide health benefits include peanuts, hazelnuts, almonds, sunflower seeds and walnuts.
- Oats and wheat, although they are not as tasty as all of the above, also contain incredibly useful substances that pregnant women need. They will improve the absorption of food and streamline the functioning of the digestive system.
Try to avoid foods high in carbohydrates, such as rice, potatoes, bread and pasta. Forget about coffee during breakfast, because it contains caffeine, which artificially affects the functioning of the heart.
Eat right and monitor your health.
When to go to the maternity hospital?
- if your water starts to break;
- if you start BLEEDING;
- if you have CONTRACTS every 6-8 minutes.
Doctors and midwives of the Women's Health Resort Clinic are always ready for pregnant women registered for pregnancy in our Clinic, if it is impossible to contact them in person, to comment remotely (by phone, Internet) on an existing or newly emerging situation.
We are at your FULL DISPOSAL if you have any doubts or wishes.
Subsections
- Pregnancy management
- Cost of pregnancy counseling
- Screening during pregnancy
- Examination of pregnant women for congenital malformations of the fetus
- Comprehensive assessment of pregnancy markers
- Ultrasound of pregnancy
- Development of pregnancy by week
- Critical periods of embryonic development
- Possible problems during pregnancy
- Proper nutrition during pregnancy
- Hygiene for a pregnant woman
- Sleeping during pregnancy
- Risk factors (caution for pregnant women)
- Determining acceptable weight gain during pregnancy
- Determining your child's date of birth
- Assessment of fetal movement activity
- Sexual life during pregnancy
- Breathing and relaxation techniques during childbirth
- Literature for preparing for childbirth and raising children
- Premature birth, threatened miscarriage
- The first days after childbirth
- Program No. 7. Postpartum rehabilitation and VUM-building
- Program No. 16. How to remove belly fat
- Breastfeeding or bottle feeding?
- Breastfeeding: problems and rules
- Swaddling a baby
- Let's go to the maternity hospital! Things for mom and baby
- Measuring basal temperature and maintaining a graph
- Teeth and pregnancy
- Our mothers
- School of Natural Motherhood
- Questions and answers about pregnancy
- Reviews about pregnancy management in our Clinic
Why is this condition dangerous?
Hypertension usually does not affect the general health of the mother and baby, but the woman is exposed to certain risks, which is why she will have to undergo examinations more often than usual.
In severe cases, hypertension can hinder a baby's growth, preventing him from getting the right amount of food, blood, and oxygen. If high blood pressure is left untreated, it can cause the placenta to separate from the uterus too early.
The biggest complication that hypertension during pregnancy can lead to is the development of preeclampsia. This is a very serious disease. Its symptoms:
- frequent dizziness;
- visual impairment;
- pain in the abdomen.
Most gynecologists will order additional tests and test your urine for proteins to look for signs of preeclampsia.