Description
Pre-stroke is a temporary deterioration in blood supply to the brain (brain). The painful state of an impending stroke has a number of characteristic signs that can be used to identify a crisis and prevent it in advance. The body can turn on self-regulation mechanisms, thanks to which the symptoms disappear without a trace within 24 hours, and the functions of the brain are completely restored.
If circumstances are unfavorable and medical care is not provided, cerebrovascular accident can result in a stroke - hemorrhagic or ischemic. This condition in some cases leads to death.
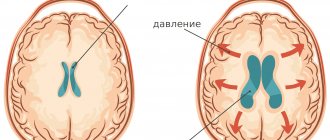
Stroke (ICD-10 code – I63-I64) is characterized by an acute disruption of cerebral blood supply, usually leading to damage and death of nerve cells. Body functions corresponding to the affected areas simply disappear. A person may have problems with speech, memory, vision, movement, balance, swallowing, etc.
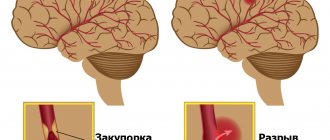
Types of strokes:
- hemorrhagic - occurs as a result of rupture of an intracerebral vessel, bleeding into the surrounding tissues, formation of a hematoma, pressing on nearby areas of the brain and causing disruption of their functioning;
- ischemic - appears as a result of blockage of a blood vessel by a thrombus, atherosclerotic plaque or embolus, while the blood supply to the brain area stops and necrosis occurs.
During a microstroke, only small areas of the brain are affected. The duration of the painful condition is from 5 minutes to several hours. In this situation, blood supply is disrupted only in the smallest vessels.
Stroke is an acute vascular accident in the brain. Lost functions may be restored after some time, or they may disappear forever. If a person shows signs of a pre-stroke, he urgently needs to provide first aid and call an ambulance.
Temporal lobe
The work of this area ensures normal memory, internal speech and mental activity, and hearing in general.
- Epileptic seizures. As is the case with those with lesions of the frontal lobes, they develop suddenly. But they last less time. Otherwise, it is not possible to notice the difference without instrumental techniques. The difference is in the localization of the pathological impulse.
- Lack of hearing. The so-called cortical deafness. The patient completely loses the ability to navigate sounds. This is a temporary phenomenon; treatment as such does not make sense.
- Lack of speech perception. Formally, there is a noise stimulus, but it is impossible to evaluate the logic of the statements, the meaning of them, and even recognize the words.
- Verbal hallucinations of the mental type. So-called pseudohallucinations in outdated terminology. The proverbial voices in my head. Associated with disruption of Wernicke's area.
It is responsible for the production of inner speech. As a result of the anomaly, the signal moves to Broca's center.
He, in turn, identifies external stimuli and perceives them as such, as outside speech. A paradoxical reaction arises.
- Memory impairments of various types. Amnesia, failures. The feeling of a repetition of something that once happened (déjà vu).
Causes
If a person shows signs of a pre-stroke condition, there are a number of reasons for this. These include: strong feelings, heavy physical activity, unhealthy lifestyle and bad habits. Most often, a pre-crisis situation is observed in patients with a number of serious pathologies. This group of patients belongs to the risk group, that is, to the category of people who need to be attentive to their health.
The following factors can precede a crisis:
- prolonged exposure to stress or severe nervous disorder;
- hard physical labor, overwork;
- addiction to alcohol and tobacco;
- uncontrolled use of medications;
- severe hypothermia or overheating of the body;
- non-compliance with diet, fatty, spicy foods, lack of fresh vegetables and fruits in the diet;
- changes in weather conditions, atmospheric pressure, magnetic storms, etc.
Risk group:
- hypertonic disease;
- obesity;
- diabetes;
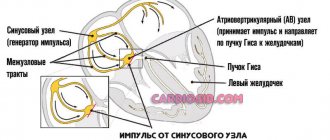
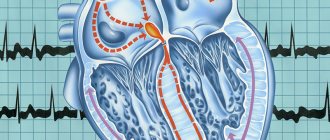
- heart rhythm disturbance;
- high cholesterol;
- blood clotting disorder;
- sedentary or bedridden patients;
- advanced age;
- gender (crisis occurs more often in men than in women);
- genetic predisposition (parents have had a stroke or heart attack);
- psychosis, depression;
- migraine;
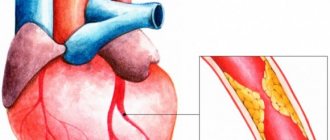
- atherosclerosis;
- vascular diseases;
- angina pectoris, heart attack, ischemic disease.
Stroke can occur at any age, even in young people suffering from a number of chronic diseases. If a girl, boy or child is at risk, they need to constantly monitor their well-being in order to recognize an approaching crisis. If pre-stroke signs appear, you should consult a doctor.
Focal symptoms of the disease
One or another part of the brain is responsible for specific processes occurring in the body. When normal blood flow ceases to be provided in one of them, specific symptoms are observed. This is what the doctor relies on when making a diagnosis. You can find out which area is affected by the nature of the clinical manifestations. Frontal cortex:
- convulsions;
- slurred speech;
- inability to make voluntary movements;
- a sudden change in habitual behavior.
Parietal lobe cortex:
- tactile sensitivity is lost;
- skills in basic arithmetic, writing and reading are lost.
Temporal lobe cortex:
- deafness develops, tinnitus is recorded, and certain hallucinations appear;
- Memory is impaired and a feeling of déjà vu develops.
Symptoms are nonspecific. Rather, for the doctor, these are additional signs that help make a diagnosis.
Symptoms
There are 2 types of transient cerebrovascular accident (TCI): transient ischemic attack (TIA) and cerebral hypertensive crisis. The symptoms of these two pre-stroke conditions are different.
TIA is the initial stage of an ischemic stroke. The reason is a narrowing or blockage of the artery that supplies the brain. The clinical picture of the condition depends on the vascular area in which the decrease in blood flow has occurred.
Acute hypertensive encephalopathy is an independent type of focal neurological disease when a pre-stroke occurs due to a sharp increase in blood pressure (BP). The blood pressure level in patients is high, it is equal to 180/120 or 200/140. In this condition, the circulatory network of the brain becomes filled with blood, and the permeability of the vessels increases and fluid passes through their walls.
Pre-stroke - main symptoms of TIA:
- numbness of the face and limbs;
- pallor;
- weakness;
- weakening of the pulse;
- facial asymmetry – one of the corners of the mouth goes down;
- speech disorder;
- stunned state;
- a person may not recognize acquaintances;
- vision problems: double vision, blurry pictures, loss of lateral vision;
- pain in the heart area;
- unilateral paresis of the limbs or individual muscle groups.
How to recognize a pre-stroke from the outside:
- the patient cannot smile;
- the mouth is curved on one side;
- it is difficult for a person to pronounce his name or repeat a phrase;
- speech is slurred and distorted;
- he cannot raise both arms up and keep them in a raised position due to weakness;
- If you ask to stick out a straight tongue, you won’t be able to do it; the organ will be curved.
Pre-stroke condition - the first symptoms of a hemorrhagic stroke:
- a sharp increase in blood pressure;
- headache bursting from the inside, which begins in the back of the head;
- nausea and vomiting;
- loss of strength, sometimes psychomotor agitation;
- difficulty breathing;
- flashing spots before the eyes;
- clouding of consciousness;
- increased sweating;
- the face becomes red or pale;
- involuntary movements;
- convulsions;
- fainting.
Pre-stroke - symptoms and first signs of the condition in women:
- dizziness;
- facial asymmetry;
- drooping lip;
- weakness of one half of the body;
- blurred vision;
- irritability and tearfulness;
- speech problems;
- clouding of consciousness.
Pre-stroke - symptoms and first signs of the condition in men:
- headache;
- numbness of the limbs and face;
- feeling of weakness;
- deterioration of health;
- impaired coordination and movement;
- stun;
- slurred speech.
Hemorrhagic stroke develops rapidly. Its main symptoms are a sharp headache, as if after a blow, and a short-term loss of consciousness. It occurs against the background of a hypertensive crisis.
Ischemic stroke develops gradually with atherosclerosis or acutely during blockage of a blood clot. The patient experiences numbness in the limbs, curvature of one side of the face, stupor, stupor and clouding of consciousness. Symptoms are precursors to a dangerous condition and must be responded to immediately, that is, call an ambulance.
Frontal lobe of the brain
Responsible for mental activity, the ability to make logical constructs, synthesis of new information from existing data, behavior, muscle tone and some other functions.
- Infantilism. The patient relapses into childhood. Primary reflexes, such as grasping and sucking, return. Behavior is inappropriate for age; this is a temporary phenomenon. Recovery after the end of the pre-stroke state is spontaneous. The intervention of doctors contributes to rapid correction.
- Thinking disorders. By type of productivity decline. The patient is unable to solve basic logical problems. Inferences are impossible, judgments do not have an adequate basis. Formally, intelligence is preserved. But the woman is unable to use the resources because the conduction of nerve impulses is disrupted.
- Unsteadiness of gait. The victim cannot walk in a straight line. This is due not so much to a violation of orientation in space, but to insufficient muscle tone, a partial loss of control over the muscles.
- Behavioral disorders. The woman becomes inappropriately cheerful, whiny, and aggressive. Accented personality traits are sharpened. Therefore, the pattern (model) of the disorder is determined by the individual properties of a particular person. His character.
- Paralysis, paresis. On the one hand, opposite to the localization of the lesion. The upper and lower limbs and face are affected. The notorious distortion of facial muscles occurs, which is inherent in a classic stroke.
- Epileptic seizures. Total or large with loss of consciousness and tonic-clonic convulsions. They cover all muscle groups and the body as a whole. It is necessary to distinguish the pathological process from classic true epilepsy. This can be done both due to accompanying symptoms, clinical picture, and based on the results of instrumental diagnostics.
Lack of smell on one side. A specific sign of damage to the frontal lobes. When subcortical structures and the limbic system are involved in ischemia, the absence of odor perception is complete.
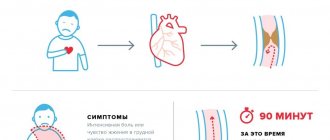
First aid
If a person has signs of a pre-stroke condition, it is necessary to urgently seek help from medical professionals. After a few minutes, the symptoms may go away on their own, but you need to wait for the doctors to arrive and undergo an examination. It is impossible to treat the victim at home with folk remedies. Before the ambulance arrives, the patient can only be given first aid.
First aid for pre-stroke:
- provide the patient with a horizontal position;
- raise your head a little, put a pillow under it;
- do not bend your neck;
- unbutton tight clothes;
- open the windows in the room to bring in fresh air;
- calm the patient;
- when vomiting, turn your head to the side;
- measure the temperature, if high, give an antipyretic (Paracetamol);
- if possible, measure blood pressure;
- if blood pressure is high, give Captopril or Nifedipine;
- if there are no medications, then to reduce the tone you need to bandage the thumb of your left hand with an elastic band, hold for 2-3 minutes, vigorously rub the hand towards the fingertips;
- Place 2 Glycine tablets under your tongue.
Doctors who arrive on call will provide the patient with the necessary assistance and give an injection. If the condition is critical, the person is hospitalized in a hospital. If not, he will be prescribed treatment at home.
Limbic system
The key symptom of damage to subcortical structures (in particular the cerebellum) is a violation of orientation in space.
The patient loses understanding of the spatial structure and her position in it. A painful manifestation. If during dizziness the sense of place is formally preserved, in this case it is also lost.
At the same time, there may be a loss of the ability to learn, absorb new information and use it.
Pre-stroke, transient ischemia of the limbic system is rare: 3-5% of the total number of cases.
Diagnostics
To identify the causes of the pre-stroke condition, a thorough examination of the patient is carried out. Based on the diagnostic results, the person is prescribed a course of therapy.
Diagnostic methods:
- blood pressure measurement;
- general blood analysis;
- blood test for cholesterol and glucose levels;
- ECG;
- Ultrasound of the carotid arteries of the neck;
- CT and MRI – for obtaining images of the brain.
A CT scan is performed to determine the presence of hemorrhage. Based on the obtained image, the patient is diagnosed with pathology. MRI allows you to see the first structural changes in the brain. If a stroke is suspected, diagnosis is carried out within the first hour after the patient is admitted to the hospital.
Occipital lobe
The functions of this part of the nervous system include color recognition and normal vision. Processing incoming visual information and converting it into understandable images.
- Complete blindness. Temporary or so-called transient. The disorder has no connection directly with the retina or the visual tract up to the brain.
- Inability to estimate the distance to an object. Understand its dimensions. Metamorphopsia occurs. Small objects appear larger than the patient herself and vice versa. The small room seems like a huge hall.
This is a direct indication of the neurogenic origin of the disorder, because the eye is not able to independently process information. This is just a source, an input for images; the processes of transformation and analysis take place in the cerebral cortex.
- Induced color blindness. Inability to recognize colors.
- Scotomas. Loss of areas of the visual field. They look like black spots that block your view. In the paracentral areas and along the periphery, usually from the side of the temples.
- The simplest visual disturbances. Photopsias. Flashes of light, bright dots, lines. Rings, geometric shapes. There is no objective source of irritation. The central nervous system is excited spontaneously. Restoring blood flow leads to compensation of the condition.
Treatment
Treatment of any disease, including pre-stroke, is carried out based on diagnostic results. Symptoms of TIA and hypertensive crisis may resolve on their own within a few minutes or hours. However, patients who experience pre-stroke conditions require medical care to prevent future strokes.
Main areas of treatment:
- preventing the risk of stroke;
- prescribing medications that reduce the likelihood of a stroke and prevent the formation of blood clots.
To reduce the risk of stroke, the patient needs to switch to a healthy diet, give up fatty foods, and replenish their diet with fresh fruits and vegetables. It is recommended to stop drinking alcohol and smoking, and get rid of bad habits. It is necessary to engage in moderate exercise daily and normalize your weight.
Medicines that reduce the risk of stroke:
- antiplatelet drugs are medications that prevent the formation of blood clots (Clopidogrel);
- anticoagulants - reduce the level of blood clotting, which leads to the disappearance of blood clots in the vessels (Warfarin, Dabigatran).
If during the examination a pathology is detected in the patient, he is prescribed treatment in order to normalize the function of the cardiovascular system, breathing, and reduce swelling of the brain. In case of ischemic attack, patients need to be treated with antiplatelet agents, anticoagulants, nootropics (Picamilon), neuroprotectors (Cavinton). Cerebrolysin, Actovegin, vitamin preparations, antioxidants and other medications that improve metabolism and tissue nutrition are used as therapy.
In case of a hypertensive crisis, drugs to lower blood pressure, diuretics, neuroprotectors, and vasoactive agents are prescribed. Often, in case of hemorrhagic stroke, surgery is performed in critical situations. In severe cases, the patient is sent immediately to intensive care.
Who is most likely to have a stroke?
There are certain risk factors for developing stroke. Persons with such risk factors, as well as their loved ones, must have a clear understanding of this complication, be able to recognize the first signs, be able to navigate and take the necessary measures. Stroke most often develops in people:
- With hypertension.
- With diabetes.
- Obese.
- With elevated blood cholesterol levels.
- With heart rhythm disturbance.
- In bedridden and sedentary patients.
- With blood clotting disorders.
As for gender and age, stroke is more common in men under the age of 60; at older ages it more often affects women.
Provoking moments for the development of a stroke can be:
- Exercise stress.
- Emotional stress.
- Changes in blood pressure (sharp increase or sharp decrease).
- Changes in atmospheric pressure.
- Alcohol intoxication.
- Overheating or hypothermia.
Complications
Repeated pre-stroke can lead to the development of a full-fledged stroke. The consequences of a hemorrhagic crisis are always more severe than an ischemic one. The mortality rate for this condition is much higher. Even if the patient suffered a crisis and survived, he may remain in a vegetative state for a long time.
After a TIA or crisis, the patient’s memory, mental performance, and vision are impaired. A stroke often causes coma, paralysis or paresis of certain muscle groups. A severe stroke can cause death.
Brain stem
With ischemia, life- and health-threatening manifestations develop. Like stopping breathing, cardiac activity. This is the only case when a pre-stroke in a woman can lead to death even without the death of cerebral tissue.
Additionally, it is possible to develop elevated body temperature. Thermoregulation is disrupted, the readings fluctuate, from 35 to 38 degrees Celsius or more.
The sign is also considered threatening and requires urgent correction in a hospital setting. The patient is constantly monitored for timely resuscitation.
Prevention
To avoid negative consequences, you need to engage in stroke prevention. People suffering from hypertension or other vascular diseases need to avoid physical and emotional stress, adhere to a healthy diet, and lead an active lifestyle. Medicines should be taken only as prescribed by a doctor. Be sure to undergo regular examinations in the hospital, measure blood pressure and blood glucose levels.
If a person has suffered a stroke, he will need to undergo rehabilitation. For this purpose, the patient is prescribed physiotherapeutic procedures, therapeutic exercises, and special exercises to restore facial expressions and eliminate its asymmetry. To return to the patient’s previous speech, classes with a speech therapist or speech pathologist are necessary. Impaired intellect and memory are treated using special techniques (micropolarization, Tomatis).
Risk factors
They do not directly cause the onset of a pre-stroke condition, but they increase the likelihood of it almost three times, and even more (depending on the specific moment).
- Smoking.
- Old age 60+. The pathology also occurs in persons slightly younger, minus 10 years.
- Being male.
- A history of cardiovascular diseases, as well as endocrine diagnoses.
- Unfavorable family history, burdened heredity.
- Alcohol abuse, drug addiction.
- Inadequate sleep.
- Unbalanced diet.
- Acclimatization, moving to another geographical region with different weather and temperature conditions.
- Menopause in women, as well as menopause in the stronger sex. Hormonal changes, attenuation of the body’s basic reproductive functions.
The patient can correct most of the factors presented on his own. Apart from age.
But in this case, it is enough to regularly consult with a neurologist and other specialists. According to indications.
Types of disease
There are quite a large number of types of stroke. The classification of the disease includes division according to the provoking causes, the mechanism of progression, and the characteristics and size of the lesion.
Usually the following types are distinguished:
- ischemic;
- extensive;
- hemorrhagic;
- lacunar;
- microstroke;
- spinal;
- repeated;
- spicy.
Ischemic stroke is considered the most common. The cause of the pathology may be a disruption in the transport of nutrients and oxygen to brain cells (usually due to narrowing of vascular channels).
Hemorrhagic stroke is a consequence of rupture of the vascular channels of the brain, as a result of which blood fills the cavities. This type entails the appearance of edema and hematoma.
A major stroke is any massive lesion. Typically, such a lesion has more severe symptoms and often leads to death or long-term disability of the patient.
Classification by severity
Based on the severity of clinical manifestations and the severity of brain damage, stroke can be divided into the following subtypes:
- transient ischemic attacks;
- micro-stroke (usually formed against the background of third-party chronic pathologies - hypertension or thrombosis, lasts from 2 to 21 days);
- moderate severity (recovery from such a lesion takes several months, swelling of the brain structures and dysfunction of consciousness do not appear);
- extensive (the most severe subtype of all, since it is formed in the beds of large vascular canals, the symptoms are the most pronounced and can lead to paralysis or death of the patient).
Rehabilitation
Elderly people who have suffered a stroke must undergo a long course of rehabilitation. This period is very important, since rehabilitation will help minimize the consequences of circulatory disorders and significantly improve your overall condition.
The list of actions to restore the patient includes both physical and psychological assistance. A person must feel important and supported; only in this case will he be able to overcome the psychological discomfort associated with the partial loss of cognitive functions.
Even if the patient’s motor function is normal, it is necessary to purchase an orthopedic mattress. When a disruption in activity does occur and a person has limited physical capabilities, it is necessary to regularly change his position (to avoid bedsores).
Often, a person who has suffered a stroke is prescribed medications to normalize blood circulation. They must be taken strictly according to the regimen prescribed by the attending physician. If signs of apathy or aggression appear, the help of a psychologist, and in some cases a psychiatrist, is necessary.
Trigger factors
They act as direct triggers.
- Consumption of alcohol in any quantity.
- Smoking. Due to a sharp spasm of cerebral vessels, basilar, carotid arteries.
- Stress, intense mental stress.
- Excessive, inappropriate physical activity. With little or insufficient training.
- Sharp tilt. Patients with possible pathologies of the cardiovascular system need to exercise extreme caution. All movements are smooth, gradual. It’s better not to bend at the waist at all, but to squat if you need to lift something.
- Acute pain syndrome.
All points are subject to evaluation. Their independent correction is possible.
How to determine pre-stroke condition
For reference. A pre-stroke condition or a stroke can be suspected if a person suddenly lost consciousness or became sharply inhibited, he developed facial asymmetry (the corner of his lips and eyelid on one side drooped), he stopped understanding speech addressed to him, or his own speech became unintelligible.
You can also do a simple test. Ask the victim:
- smile (in case of a pre-stroke condition or a stroke, the smile will be crooked);
- open your mouth and move your tongue from side to side (a patient with a pre-stroke condition will not be able to do this, the tongue will deviate to one side);
- raise your arms straight and hold them parallel to the ground (one arm will quickly drop, or the patient will not be able to lift it);
- ask him to answer a series of simple questions: name, year of birth, where he is now, today's date (a patient with a pre-stroke condition or stroke may not understand the questions or be unable to answer them).
Yes, this test is also used to determine stroke. However, here you should pay attention to the time of onset of symptoms. If an incomprehensible condition has occurred recently, then we can consider it a pre-stroke.
But if an hour, two or more has passed (they just didn’t pay attention), then the test will confirm the onset of a stroke and you need to act immediately.