Pressure
40 thousand die every year due to cerebral hemorrhage due to high blood pressure. At the same time, if you follow the rules for controlling blood pressure and do not provoke its increase, you can avoid not only feeling unwell, but also more serious problems.
A persistent increase in blood pressure above 140/90 is a serious factor for concern and suspicion of the risk of cardiovascular disease.
Too rare (less than 50 beats per minute), frequent (more than 90–100 per minute) or irregular pulse should also alert you; such deviations may indicate coronary disease, a violation of the conduction system of the heart and the regulation of cardiac activity.
Methods for diagnosing coronary heart disease
When examining a patient, the doctor determines which diagnostic methods are necessary in this particular case.
Diagnosis of IHD is carried out by cardiologists. To determine the condition of the heart, the following are used:
Blood chemistry
A biochemical blood test for ischemic heart disease includes indicators such as glucose, cholesterol, AST and ALT and cardiac-specific markers (troponin I, myoglobin, etc.).
More information about the diagnostic method
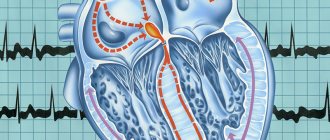
ECG
ECG is a basic diagnostic procedure in cardiology. But ECG data is often not enough. So, with angina pectoris, an ECG will show pathological changes only during an attack, and at rest such changes may be absent.
More information about the diagnostic method
Echocardiography
Echocardiography (EchoCG) for IHD is used to diagnose the disease, risk stratification and select a medical strategy in the case of already established IHD.
More information about the diagnostic method
To identify changes that cannot be detected during examination at rest (at a doctor’s appointment), Holter (24-hour) ECG monitoring can be used. Sensors are attached to the patient’s body, the information from which is sent to a portable device. The patient leads his usual lifestyle. The received data is then processed. In this way, cardiac abnormalities are detected.
Treadmill test
Exercise tests can help identify heart problems. In modern medicine, such varieties as the treadmill test (a treadmill is used) and bicycle ergometry (an exercise bike is used) are common.
More information about the diagnostic method
Coronary angiography
Coronary angiography allows you to study the patency of the coronary vessels and the degree of their changes.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Pain resembling osteochondrosis
Pain between the shoulder blades, in the neck, left arm, shoulder, wrist, even in the jaw can be a sure sign of not only osteochondrosis or myositis, but also heart problems.
Article on the topic
Stroke: risk factors, dangerous symptoms, first aid A symptom of angina pectoris may be the occurrence of such symptoms after physical activity or emotional shock. If pain occurs even during rest and after using special heart medications, this symptom may indicate an approaching heart attack.
Panic attack
A panic attack is a sudden episode of intense anxiety. It includes the following symptoms:
- chest pain;
- dizziness;
- cardiopalmus;
- shiver;
- feeling of suffocation;
- nausea;
- digestive problems;
- too hot or cold;
- sweating;
- shortness of breath;
- fear of death.
Chest pain
A feeling of burning and squeezing, obvious, dull, severe or periodic pain, spasm - all these sensations in the chest are the surest sign of heart problems. With spasm of the coronary vessels, the pain is burning and acute, which is a sign of angina pectoris, which often occurs even at rest, for example at night. An attack of angina is a harbinger of myocardial infarction and coronary heart disease (CHD).
Severe, prolonged pain in the chest, radiating to the left arm, neck and back, is characteristic of a developing myocardial infarction. Chest pain during myocardial infarction can be extremely severe, including loss of consciousness. By the way, one of the most common causes of heart attack is atherosclerosis of the coronary vessels.
Chest pain radiating to the back of the head, back, or groin area is a symptom of an aortic aneurysm or dissection.
Dull and wave-like pain in the heart area, which does not spread to other areas of the body, accompanied by an increase in temperature, indicates the development of pericarditis.
However, acute chest pain may also indicate other diseases, for example, be a symptom of intercostal neuralgia, herpes zoster, sciatica in the neck or chest, spontaneous pneumothorax, or esophageal spasm.
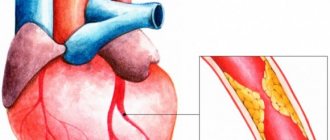
Causes of coronary heart disease
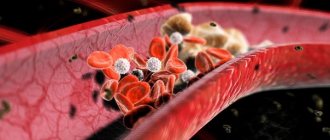
In the vast majority of cases, the cause of the development of IHD is atherosclerosis. Atherosclerosis is characterized by the formation of plaques (fatty deposits) on the walls of the arteries, which gradually block the lumen of the vessel. Such plaques can also appear on the walls of the coronary arteries. Gradually increasing disruption of blood flow in the coronary arteries leads to the development of chronic forms of coronary artery disease. Acute forms of IHD are usually caused by blockage of a vessel with a thrombus or a detached part of an atherosclerotic plaque. Other causes of IHD are:
- spasm of the coronary arteries;
- increased blood clotting. In this case, the risk of blood clots increases;
- an increase in heart size (a consequence of some diseases). At the same time, the growth of the vascular network lags behind. The result is a lack of blood supply to the enlarged heart muscle;
- persistent low or high blood pressure (hypotension or hypertension);
- diseases of the thyroid gland (thyrotoxicosis) and some others.
Factors contributing to the development of ischemic heart disease
The risk of developing coronary heart disease increases:
IHD
- smoking;
- increased cholesterol levels in the blood;
- obesity (overweight);
- arterial hypertension;
- diabetes;
- physical inactivity (low physical activity).
People over 50 years of age are at risk. Moreover, men suffer from coronary heart disease more often than women. The hereditary factor is also important: the likelihood of developing IHD increases if it was detected in one of your close relatives.
Palpitations
Palpitations can occur during intense physical activity, as a result of a person's emotional arousal, or due to overeating. But a strong heartbeat is very often an early warning sign of cardiovascular disease.
A strong heartbeat manifests itself as a feeling of disruption in the functioning of the heart; it seems that the heart is almost “jumping out” of the chest or freezing. Attacks may be accompanied by weakness, discomfort in the heart, and fainting.
Such symptoms may indicate tachycardia, angina pectoris, heart failure, or impaired blood supply to organs.
If you have at least one of the listed symptoms, it is important to immediately consult a doctor and undergo tests that will reveal the true cause of the ailment. One of the most effective methods of treating any disease is its early diagnosis and timely prevention.
Nausea
Nausea is a peculiar unpleasant sensation in the epigastric region, chest, and oral cavity, which often precedes vomiting and is often accompanied by general weakness, sweating, increased salivation, cold extremities, pale skin, and decreased blood pressure.
Causes of nausea
Possible causes not related to any disease:
1. Overeating and/or regularly eating foods that are very high in fat;
2. Side effects of medications and penetration of toxic substances into the body;
3. Psychogenic reactions: fear and anxiety, hysteria;
4. Kinetosis (seasickness), accompanied by a feeling of nausea and motion sickness;
5. Pregnancy (morning sickness normally goes away by the end of the first trimester);
6. Exposure to smoke, toxic fumes and various harmful substances;
7. Sunstroke, hyperthermia.
Diseases accompanied by nausea
Diseases that cause nausea are very diverse and can be associated with the digestive, nervous, reproductive, cardiovascular and endocrine systems.
Most often, nausea develops due to pathologies of the gastrointestinal tract, including:
1. acute surgical diseases: peritonitis, appendicitis, acute pancreatitis, acute intestinal obstruction, gastrointestinal bleeding, acute cholecystitis;
2. chronic diseases: gastroesophageal reflux disease (GERD) and hiatal hernia, gastritis, peptic ulcer of the stomach and duodenum, enterocolitis, duodenitis, cholelithiasis, inflammatory bowel disease (Crohn's disease, ulcerative colitis), irritable bowel syndrome, chronic pancreatitis ;
3. malformations of the gastrointestinal tract: narrowing of the pylorus (stenosis), fusion of a section of the gastrointestinal tract (atresia), developmental defects of the pancreas;
4. gastrointestinal tract infections: viral gastroenteritis, food toxic infections, helminthiases;
5. foreign bodies of the stomach, esophagus, intestines;
6. functional disorders accompanied by impaired motor function of the stomach and intestines;
7. liver diseases (hepatitis, cirrhosis of the liver);
8. food intolerances or food allergies.
In addition to disruption of the gastrointestinal tract, nausea can be caused by diseases of other organs and systems:
1. Diseases of the central nervous system: brain tumors and injuries, brain infections (encephalitis, meningitis), increased intracranial pressure.
2. Diseases of the cardiovascular system: hypertension, heart failure, myocardial infarction.
3. Diseases of the inner ear: Meniere's disease, labyrinthitis.
4. Diseases of the endocrine system: in diabetes mellitus – ketoacidosis; thyrotoxicosis, adrenal insufficiency, phenylketonuria.
5. Kidney diseases (urolithiasis, renal failure);
Nausea is associated with cancer treatment (chemotherapy and radiation therapy), imbalance of blood electrolytes, and migraines.
Nausea can be a manifestation of such emergency conditions as poisoning, diabetic ketoacidosis, intestinal obstruction, cerebral hemorrhage, acute cardiovascular pathology, renal failure, liver failure, sepsis.
Most often, nausea does not appear independently, but in combination with other symptoms: abdominal pain, belching, diarrhea, increased gas formation, dyspepsia, vomiting, muscle pain, dizziness, severe fatigue, fever and chills, headache, yellowing of the skin and sclera.
Particular attention should be paid to the combination of nausea with the following symptoms: black stools or the presence of blood in the stool, the presence of blood in the vomit, severe abdominal pain, difficulty breathing, fainting, impaired consciousness, high body temperature (more than 38.5 ° C), rapid pulse, frequent shallow breathing, severe headache, stiff neck. The appearance of these symptoms indicates the development of a life-threatening condition, if detected, you should immediately consult a doctor. You should also definitely see a doctor if you feel sick after a head injury.
Examination of a patient with nausea.
Nausea is a nonspecific symptom of many diseases; therefore, it has diagnostic value only in conjunction with other signs of the disease (for example, with signs of peritoneal irritation in acute appendicitis).
To determine the direction of the examination, it is necessary to conduct an active interview with the patient. So, if nausea is accompanied by other dyspeptic manifestations (belching, a feeling of heaviness in the epigastric region, etc.) and a relationship is identified between the occurrence of nausea and food intake, diseases of the digestive system should be assumed (gastritis, cholecystitis, pancreatitis, stomach tumor, etc.) and conduct a gastroenterological examination; when nausea is combined with headache, sensitivity or movement disorders, a neurological examination, etc. is necessary.
Determine what medications the patient took. Drugs that often cause nausea and vomiting include analgesics, cardiovascular drugs, hormonal agents, antibiotics, drugs that primarily act on the central nervous system, and antineoplastic agents. Drug use or withdrawal may also cause nausea or vomiting. If discontinuation of a drug is accompanied by the disappearance of nausea, we can assume that this disorder is associated with taking the drug, but it is necessary to ensure that there are no symptoms for a significant period of time after discontinuation of the drug.
An objective examination reveals an “acute abdomen” and other life-threatening conditions. If the cause of nausea has not been established, a laboratory examination is performed:
1. general blood test (possible anemia, leukocytosis, accelerated ESR in case of gastric ulcer, duodenal ulcer, ulcerative colitis, etc.);
2. electrolytes, urea, creatinine (studied to diagnose kidney function and assess fluid and electrolyte disorders);
3. biochemical indicators of liver function: ALT (alanine aminotransferase), AST (aspartate aminotransferase), gamma glutamyl transpeptidase, total protein level in the blood, blood albumin, bilirubin);
4. blood glucose (normal values are 3.3-5.5 mmol/l, an increase in glucose levels indicates the likelihood of diabetes mellitus);
5. biochemical indicators of pancreatic function: alpha-amylase enzyme, lipase enzyme;
6. antibodies to Helicobacter pylori (to detect gastric ulcers associated with Helicobacter pylori infection);
7. In the analysis of stool when diagnosing diseases of the digestive system, the quantity, consistency and shape, color, smell, impurities, presence of mucus, pH are assessed; at the chemical level, the content of blood, bilirubin, stercobilin, and protein is determined;
8. The study of intestinal microflora is carried out when diagnosing intestinal dysbiosis.
The plan for further examination depends on the patient’s age and clinical manifestations. It should be especially careful if nausea and vomiting occur for a long time.
Pregnancy tests should be performed in women of childbearing age.
Sometimes a general urine test, a toxicological study, cultures, and a study of the function of the endocrine glands (TSH and thyroid hormone levels, morning fasting cortisol levels) are needed.
To exclude diseases of the gastrointestinal tract, diseases of the liver and biliary tract, a survey radiography of the abdominal cavity, examination of the stomach and intestines with barium, ultrasound of the abdominal organs, CT and endoscopic examinations are performed.
FEGDS (fibrogastroduodenoscopy) is intended primarily to exclude obstruction, gastric or duodenal ulcers or other organic pathology.
Colonoscopy is necessary to identify nonspecific ulcerative colitis, Crohn's disease, chronic non-ulcerative colitis, if a tumor process is suspected.
pH-metry is carried out to study the secretory function of the stomach if gastritis or gastric ulcer is suspected.
Rectomanoscopy is used for diseases of the rectum.
If a neurological disorder is suspected (migraine, increased intracranial pressure, pathology of the inner ear), which can cause constant or periodic nausea, a clinical neurological examination should be performed, to exclude increased intracranial pressure by examining the fundus of the eye or conducting magnetic resonance imaging of the brain.
Sometimes esophageal manometry, 24-hour esophageal pH-metry, a study of gastric motility and evacuation function, and sometimes electrogastrography and a study of small intestinal motility are required to make a diagnosis.
If psychiatric illnesses that cause constant or recurrent nausea, anxiety disorders, depression, or eating disorders are suspected, a consultation with a psychiatrist is prescribed.
Treatment of nausea
Since nausea is a symptom, its treatment method depends on the cause or underlying disease. If you suspect a disease, it is important not to self-medicate, since nausea may be associated with emergency conditions or the initial manifestation of severe pathology, which require immediate consultation with a doctor and the initiation of specific treatment under medical supervision.
If the cause is not related to the disease, it is necessary to eliminate the harmful factor (sun, smoke, excess food) as quickly as possible.
For seasickness, it is possible to use scopalamine in the form of a skin patch 5-6 hours before the start of the trip.
During pregnancy, rest and rest are recommended; it is possible to use meclozine orally 25 mg 2 times a day or in suppositories 50 mg.
To eliminate nausea in such cases, it is possible to use folk remedies:
• For nausea and vomiting in pregnant women, it is recommended to eat little and often. In the morning, drink only water with lemon or slightly sweetened juice, and eat crackers.
• A proven remedy for nausea is green tea.
• Grate ginger root and add to dishes.
• Before meals, drink 0.25-0.5 tablespoons of fresh potato juice.
• Pour a glass of boiling water over a tablespoon of peppermint leaf. Let it brew for two hours. Take the tincture one tablespoon three times a day.
• Boil a teaspoon of dill seeds in 200 ml of water. Take in case of poisoning or stomach upsets.
• Pour a glass of boiling water into 4 teaspoons of dry crushed lemon balm herb. Leave for several hours. Drink ½ cup four times a day before meals.
• Pour 400 ml of cold water into two teaspoons of three-leaf watch, leave for eight hours. Use within 24 hours. Used for nausea to stimulate digestion.
Possible complications
In some cases, if left untreated, nausea can lead to complications such as dehydration (impaired water and electrolyte balance in the body) and nutritional deficiencies in the body. As a rule, this is due to the inability to retain water or food in the body, as well as a lack of appetite.
Which doctor should I contact if I have nausea?
Depending on the accompanying symptoms, you may need to consult a therapist, gastroenterologist, neurologist, psychiatrist, toxicologist, endocrinologist, or allergist.
Food poisoning
Food poisoning occurs when you eat food contaminated with harmful bacteria. This may lead to:
- stomach cramps;
- pain due to gas that may spread to the chest;
- diarrhea;
- vomit;
- fever;
- nausea.
Important! If you have a fever or are dehydrated, you may feel dizzy.
Diagnosis of the root cause
Your doctor will use several tests to determine the cause of your symptoms. This will include:
- Physical examination. The doctor will examine your chest, neck, and head. It will also listen to your heartbeat and measure your blood pressure.
- Disease history. This helps the doctor understand the risk for certain diseases.
- Visual tests. You may have a chest x-ray and a CT scan. These tests take detailed photographs of your heart, lungs and arteries.
- Blood tests. Some heart diseases increase levels of proteins or enzymes in the blood. Your doctor may order blood tests to measure these levels.
- Electrocardiogram (ECG). An ECG measures the electrical activity of your heart. The results can help the cardiologist determine whether part of the heart muscle is damaged.
- EchoCG. Echocardiography uses sound waves to capture videos of your heart, which can help identify heart muscle problems.
- Stress test. A stress test checks how exercise affects your heart and blood vessels. A common example is walking on a treadmill while it is connected to a heart monitor.
- Arteriogram. Helps the doctor find damaged arteries. The dye is injected into the blood vessels of your heart, making them easier to see under X-rays.
Intestinal gases
Anyone can experience bloating (air in the digestive tract). If gases build up, you may experience:
- abdominal pain;
- belching;
- flatulence;
- feeling of fullness (bloating).
Important! If you have pain in your upper abdomen, you may feel it in your chest. The pain can also lead to nausea or dizziness.