Leukoaraiosis is a brain disease that develops due to chronic processes of ischemia of the white matter, which leads to changes in tissue structure and determines the strategy for how to treat it. Due to the deterioration of blood supply to the white matter tissue, necrotic processes occur, its density decreases, and neural connections are disrupted.
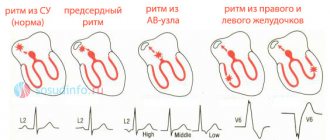
Zones of leukoaraiosis form in the brain during the development of many diseases. The pathological condition reflects destructive processes occurring in brain tissue and is a characteristic symptom of diseases of the central nervous system - discirculatory encephalopathy (malfunctions of the circulatory system), dementia (dementia), multiple sclerosis (multiple replacement of brain tissue with connective tissue), stroke, Alzheimer's disease (death of neurons) .
Definition
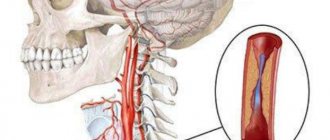
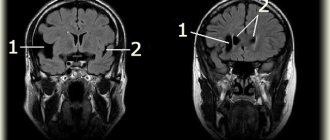
Cerebrovascular diseases are a group of brain diseases caused by pathological changes and focal dysfunction of the brain substance due to insufficient supply of tissues with oxygen and nutrients. There are acute and chronic, ischemic and hemorrhagic processes. In 1987, Khachinsky proposed the concept of leukoaraiosis (from the Greek leuko = white and araios = rarefaction) in order to define abnormalities in the white matter of the brain on CT and MRI scans. Damage can be pinpoint or wider: focal and diffuse. No clinical or pathological relationship has been proposed with this term, so it is merely a term to describe abnormal, fairly common images. That is, we are talking about a type of neuroimage that can be associated with various clinical and pathological situations, heterogeneous in the type of morphological disorders. White matter is nourished by the complex microvascular system of the brain, which consists of small threading arterioles originating from the main arteries of the brain. We are talking about the final arteries of great length and small size. Because of this, the white matter near the ventricles (in the periventricular space) becomes an area of limited vascularity, making it particularly prone to ischemia. The narrowing and reduction of blood flow in the arterioles can lead to a decrease in blood flow to a certain area and, after some time, lead to the appearance of leukoaraiosis. The development of leukoaraiosis usually follows a certain scenario. First, periventricular lesions are observed near the borders of the lateral ventricles (Fig. 1), then, depending on the severity of the problem, new lesions form around the original lesions (Fig. 2).
Fig.1
Fig.2
Degrees of leukoaraiosis at a young age
The formation of pathological foci and ischemic segments near the ventricles has different severity.
Classification of leukoaraiosis by morphology:
- 1st degree – slight loss of coordination, decreased walking speed;
- 2nd degree – development of clinical symptoms of movement disorders, loss of concentration and memory;
- Grade 3 is accompanied by a significant expansion of the ventricular spaces, increasing the manifestations of the disease. Patients require outside supervision;
- Grade 4 is characterized by uncontrolled urination, loss of balance, and suppression of psychomotor activity.
The progression of the pathology takes several years. Morphological changes are irreversible, so it is better to verify first-degree brain disorders, when supportive treatment can be selected.
The child has no clinical symptoms. Diagnosis is carried out due to the impossibility of treating speech disorders.
Degrees and symptoms
As a descriptive term, leukoaraiosis itself has no symptoms, but varying degrees of neuroimaging of these lesions are associated with corresponding symptoms. The main symptoms associated with some degrees of leukoaraiosis are ischemic stroke, cognitive impairment, gait disturbances, mood swings and sphincter disorders. There are the following degrees of leukoaraiosis from 0 to III: – 0 and I degrees are quite mild and without corresponding known specific symptoms. – II and especially III degrees are more severe, this type of leukoaraiosis affects a wider area of the white matter of the brain, damages both hemispheres, lesions are widely distributed throughout the brain, the disease becomes progressive. It is usually found in people with mental disorders that are associated with neurological damage or symptoms of dementia.
Diagnostics
As we have already mentioned, leukoaraiosis is visible on CT and MRI neuroimages of the brain , with a decreased and increased frequency, respectively. MRI of the brain , including T2 and FLAIR series, is the most common technique for detecting leukoaraiosis. The Fazekas grading scale (Fig. 3) is most often used to determine the degree of white matter lesions on MRI images: – grade 0 : no lesions; – grade 1 : isolated lesions; – degree 2 : lesions are connected to each other; – grade 3 : lesions covering specific areas of the brain.
Fig. 3 Fazekas rating scale.
– According to the Filum System® method:
We often see images of leukoaraiosis in the white matter of the brain in horizontal MRI sections with a T2 signal, most often it is grade 1 and less often grade 2, in patients diagnosed with pathologies included in filum terminale disease or neuro-craniovertebral syndrome. Their number is about 45 % of our entire database and includes all age groups.
Stages of development
Leukoaraiosis of the head, as a disease, goes through three stages of development:
- With stage 1 of the disease, a medical examination can reveal revitalization of tendon reflexes, human instability, a reduction in step length when walking, and the ability to move only slowly. Neuropsychological examination reveals suppression of cognitive changes. The person complains of poor attention and memory deterioration, and cognitive activity is significantly reduced.
- At stage 2, the presence of clinical syndromes is clearly visible. The patient notices memory deterioration, and at the same time mental and psychomotor reactions slow down. A person cannot control his actions and notices uncertainty in his own walking. In some cases, the presence of apathy, depression, irritability and lethargy is noted. There is deterioration in the functioning of the genitourinary system - uncontrolled urination at night. A person loses social adaptation, which manifests itself in the form of deterioration in performance and the inability to care for oneself independently.
- At stage 3 , the clinical picture worsens and leads the patient to disability. Behavioral disorders are clearly noticeable (severe lethargy, inability to walk independently, which sometimes ends in a fall, chronic urinary incontinence). At this stage, doctors note pronounced signs of a disorder in the functioning of the cerebellum.
Causes
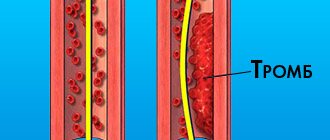
Currently, the pathogenesis of leukoaraiosis is controversial. Some authors recall that it has not yet been clarified to what extent the mechanisms that provoke small foci of ischemia coincide with those that cause extensive diffuse leukoaraiosis. In addition, it is unknown whether the pathological abnormalities associated with leukoaraiosis are the cause or consequence of lesions in the white matter. There are two main hypotheses: an abnormality in self-regulation of blood flow or a violation of the blood-brain barrier . The most recognized mechanism for the appearance of leukoaraiosis today is chronic ischemia due to damage to penetrating arteries. Hypertension and other pathologies affecting blood flow and oxygen supply to the brain appear to be closely associated with extensive leukoaraiosis. – According to the Filum System® method: Based on the observed association between leukoaraiosis and individual small foci of ischemia on images in patients diagnosed with filum terminale disease and neuro-craniovertebral syndrome , our center has developed a hypothesis for a possible pathogenesis: leukoaraiosis may also be associated with tension of the spinal cord due to too tight filum terminale. In this case, ischemia can appear in all tissues of the nervous system due to the collapse of small-diameter blood vessels.
Preventive measures
To date, there is no vaccine or medicine that could protect against the development of leukoaraiosis in the future.
For preventive purposes, doctors may advise leading a healthy lifestyle. A person should live in a mode of moderate activity and monitor nutrition. It is important to give up bad habits, because they have a detrimental effect on the functioning of the central nervous system.
If there is a cerebrovascular disease, the patient should receive timely treatment. Older people should have their functioning assessed regularly.
Risk factors
On the one hand, recognized risk factors for cerebrovascular disease relate to hereditary or individual characteristics and lifestyle . On the other hand, the main risk factors for the appearance of leukoaraiosis are: age and hypertension , although it is also associated with diseases such as diabetes mellitus, heart disease or arterial stenosis, which affect the disturbance of the microcirculation of the brain, leading to demyelization of vascular origin, which can provoke the appearance of foci of ischemia. Leukoaraiosis is also associated with older age and senile dementia , although it is often found in relatively young people (approximately 40 years of age) who use drugs such as heroin, tobacco , or are in constant contact with toxic substances . Such people are prone to the appearance of leukoaraiosis of any degree. Arteriosclerosis also considered one of the factors in its appearance. – According to the Filum System® method : Patients with leukoaraiosis in the white matter of the brain and diagnoses of filum terminale disease and neuro-craniovertebral syndrome have a common risk factor: family predisposition . Tension in the nervous system caused by filum terminale (filum terminale disease) can cause disruption of the blood supply to the spinal cord and throughout the nervous system. This is a genetic disease that is inherited.
What is cerebral leukoaraiosis
The absence of an established etiology of the disease requires the identification of provoking factors. The condition is provoked by impaired blood supply, ischemia (insufficient oxygen supply), encephalopathy, Alzheimer's disease, multiple sclerosis. It is detected accidentally after magnetic resonance imaging of the primary nosological form.
The morphological substrate of the disease is destructive changes in nerve fibers with loss of myelin. Loss of the sheath results in a “short circuit” where nerve signal transmission is disrupted. The overlapping of unprotected nerve trunks on top of each other leads to a redistribution of the transmitting impulse, like exposed electrical wires.
Morphological changes in the zone of leukoaraiosis:
- Local intracerebral edema;
- Formation of cysts;
- Expansion of spaces around blood vessels;
- Single lacunar infarctions.
Clinical symptoms of white matter changes do not form. The absence of signs excludes earlier detection of pathology.
Treatment
There are usually several effective treatments to delay the development of leukoaraiosis, which are recommended depending on the disease to which it occurs. The most appropriate treatment to delay the development of leukoaraiosis is to maintain a balanced diet, with foods rich in folic acid, folates and B vitamins. It is recommended to avoid toxic substances and an unhealthy lifestyle. – According to the Filum System® method : Given the fact that leukoaraiosis is common in patients with filum terminale disease, in our center patients who have areas of ischemia in the white matter on brain MRI are recommended to undergo a diagnosis using the Filum System® in order to determine whether there is disease of the filum terminale. If there is tension on the filum terminale, then dissection of the filum terminale is proposed with an exclusive minimally invasive technique. In several cases, a decrease in leukoaraiosis has been observed after cutting the filum terminale, further suggesting that its occurrence may be associated with abnormal tension in the nervous system.
Goals and methods of therapy
The main goal of treatment is to reduce the manifestation of symptoms that are a consequence of disruption of the human brain.
The doctor prescribes medications to the patient whose action is aimed at optimizing metabolic processes and improving blood flow to the brain. Medicines reduce spasms and improve blood circulation and cell nutrition.
For this purpose, one of the following drugs is selected: Piracetam, Oxiracetam, Nitroglycerin, Aspirin, Nimodipine, Cinnarizine, Eufillin.
Self-medication for such a serious illness is not worthwhile. Only a specialist in this matter will be able to correctly calculate the dose and choose the right drug. For this purpose, you should visit the office of a neurologist, who should additionally pay attention to all associated pathologies.
Today, there are methods for treating the disease without the use of medications.
Moderate physical activity promotes rapid recovery. To choose the right load, you should consult with a physical therapy doctor and perform therapeutic exercises yourself at home. Swimming has a positive effect on the body, so the patient is recommended to visit the pool regularly.
Therapeutic massage is used to further strengthen muscle tone. Only a qualified and experienced specialist will be able to correctly navigate the required complex and apply it correctly. To obtain the best result, it is advisable to use all methods in combination.
The patient is advised to completely stop drinking alcohol and smoking. He should eat a balanced diet and exclude fatty foods from the diet. Particular attention should be paid to the consumption of vegetables and fruits, fish. If a person loves meat, then the choice should be a low-fat variety.
A favorable outcome can be expected only if the pathology is detected in a timely manner. With the help of a properly selected integrated approach to therapy, it is possible to significantly slow down the progression of the disease. Therapeutic methods are used not only to eliminate pathology, but also to improve the flow of blood to the brain.
Bibliography
- John Conklin, Frank L. Silver, David J. Mikulis, Daniel M. Mandell. Are acute infarcts the cause of leukoaraiosis? Brain mapping for 16 consecutive weeks. Annals of Neurology, 2014; DOI: 10.1002/ana.24285.
- Hachinski VC, Potter P, Merskey H: Leuko-araiosis, Arch Neurol. 1987; 44: 21-23.
- Revista Habanera de Ciencias Médicas, versión On-line ISSN 1729-519X.Rev haban cienc méd vol.12 no.3 Ciudad de La Habana jul.-set. 2013, CIENCIAS CLÍNICAS Y PATOLÓGICAS.
- Dr. Miguel B. Royo Salvador (1996), Siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia , impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve.”