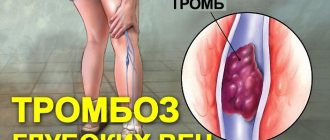
Blood clots can form not only in veins, but also in the cavities of the heart and arteries.
The formation of blood clots is a natural reaction of the body. They help restore damaged blood vessels. A thrombus is a blood clot containing fibrin (a protein necessary for blood clotting). But blood clots in the cavities of the heart are a completely different matter.
The most dangerous thing is that there are no symptoms that would suggest the presence of intracardiac blood clots. A thrombus can be detected in the cavities of the heart only through diagnostics (echocardiography, etc.). A person may experience any symptoms (shortness of breath or suffocation) only with pulmonary embolism.
Thrombi can be in the left or right cavities of the heart, located in the atria or ventricles (most often these are parietal thrombi).
What are blood clots?
- Floating. These are partially attached blood clots. The danger is that the floating part of the clot may come off;
- Parietal, when the clot is completely attached to the wall of the heart chamber;
- Clogging (occlusive). The most dangerous! These clots block blood flow.
General information about blood clots
Answering questions about thrombosis - what it is and why it occurs, it should be noted that in a healthy person this is a natural protective function of the body. It is important to promptly stop blood loss when blood vessels are damaged. When an injury occurs, platelets enter the wound and clog the resulting hole.
When the body is functioning properly, blood clots form only at the site of injury. If this mechanism is disrupted, there is a high probability that the clots will be located in the coronary vessels or in the heart.
In the initial stage of the pathology, fibrin threads form on the vessel wall, onto which thrombolytic masses are gradually applied, which increases the size of the clot.
Until the clot breaks loose or the vessel is blocked, the patient may not even be aware of its presence, feel pain, and generally feel unwell.
- Swimming with one end free.
- Parietal, when the clot is completely adjacent to the vessel.
- Centrally when it sticks to clots.
- The lining is where the clot runs along the wall, leaving a very narrow light for the blood to pass through.
- Clogging. The most dangerous is when a blood clot completely blocks the blood flow.
Why does a clot form?
Normally, thrombus formation is a physiological process that does not lead to the development of pathologies. And only under the influence of certain factors, the resulting clots do not dissolve, but attach to the vessels, clogging their lumen and disrupting blood flow.
Risk factors include the following diseases of the cardiovascular system:
- cardiac aneurysm;
- atrial fibrillation;
- myocardial infarction;
- cardiac ischemia;
- congenital and acquired valve defects;
- dilated cardiomyopathy;
- chronic heart failure (CHF).
The risk of developing thrombosis increases significantly if the patient has several of the above diseases.
The resulting thrombus in the heart is classified into right- or left-sided, atrial and ventricular (parietal). A special type of clot (spherical) occurs with mitral stenosis.
Reasons for education
Most often, problems occur in older people due to age-related changes in the heart muscle or valves. The risk group may include bedridden patients, postoperative patients, and obese people.
In addition, thrombosis develops in:
- Pathological diseases of the vascular wall or its damage.
- Reduced blood flow rate.
- Blood diseases affecting its composition.
- Violations of the quantity and volume of blood components.
Predisposing factors include:
- Stress.
- Lack of physical activity.
- Hereditary predisposition.
- Long-term use of hormonal drugs.
- Abuse of bad habits: smoking, alcoholism.
- Excess body weight.
The causes of the disease may be the presence of other pathologies, such as:
- Neoplastic diseases in which blood viscosity increases.
- Heart defects. In this case, there is often stagnation of blood due to insufficiency of the organ valves.
- Myocardial infarction. Impaired blood supply causes inflammation of the heart muscle and a decrease in the speed of blood flow.
- Cardiac aneurysm. The walls of the veins swell, slowing down the contraction of the heart muscle, which leads to the formation of blood clots.
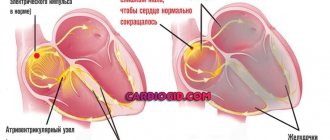
- Atrial fibrillation. Changes in rhythm cause the heart to increase in size, causing blood clots to form.
- Atrial fibrillation due to impaired blood flow.
- Dilated myocardial cardiomyopathy. This causes the chambers of the heart to stretch, which can lead to pulmonary embolism or heart failure.
- Ischemia. Impaired coronary circulation is a prerequisite for arrhythmias and heart attacks.
- Pneumonia. Increased production of fibrin, which is the basis of blood clots.
What is a blood clot and how does it form?
To start the process of thrombus formation, several conditions are necessary:
- damaged vessel wall;
- decreased blood flow speed;
- disorders of the rheological properties of blood.
These factors are the trigger for a number of biochemical reactions involved in the formation of a blood clot.
There are three main stages of the process:
- Release of the enzyme thromboplastin from destroyed platelets.
- Thromboplastin, with the help of Ca2+ ions, accelerates the conversion of inactive plasma protein prothrombin into thrombin.
- Under the influence of thrombin, insoluble fibrin is formed from fibrinogen. The threads of the latter form a mesh in which blood cells are retained. The resulting structure tightly covers the damaged area, stopping bleeding. Normally this process takes 5-10 minutes.
After healing of the affected area, the resorption of the formed blood clot is ensured by the fibrinolysis system. An imbalance between the interaction of these two systems determines the risk of the occurrence and development of thrombosis.
Features of the location of blood clots in the atria
Symptoms may indicate which side the clot is on. Location in the atrium causes fainting, dizziness, arrhythmia, tachycardia. Right heart thrombosis causes shortness of breath, shortness of breath, pale or blue skin, and cyanosis.
Depending on the composition and location, clots can be:
- Hyaline, when proteins are present but fibrin is not present. Most often found in small vessels.
- Red because they contain a lot of red blood cells. Mainly located in veins.
- White, containing fibrin, platelets, leukocytes. They are most often found in the arteries.
The heart clot is usually multi-colored as it is a mixture of all these types. The head consists of a white blob, the body is a mixed area, and the tail is a red blob.
The clot can be mobile or stationary. In the first case, it moves freely between the ventricles and atria. If the clot is immobile, it has a polyp-like stalk that is attached to the endocardium.
What is thromboembolism
Its name itself speaks about the nature of the pathology.
A thrombus is a clot of coagulated blood. If this clot forms in the lumen of the vessel and impedes blood flow, thrombosis develops. Embolism is a pathological process of circulation in the blood or lymph of particles that are not natural components of these physiological fluids. Accordingly, thromboembolism is the entry into and blockage of blood vessels by pieces of blood clots that have broken away from the site of their formation. The appearance of blood clots is a natural defense mechanism of the body associated with the physicochemical properties of blood elements. Its main participants are platelets. They are called repair cells because when any injury occurs, they are immediately activated and sent to the site of hemorrhage.
Platelets stick together and bind to fibrin, a water-insoluble protein. The resulting clot reliably protects the vessel from significant blood loss. After tissue restoration, the thrombus completely resolves without affecting blood quality.
But when the properties of blood change under the influence of various negative factors, blood clots that form on the walls of damaged vessels break off and begin free migration along the vascular beds. At any moment, their particles can completely block the blood flow, which threatens a person with serious complications, including death.
Possible consequences
In the case of mass detachment, it can move freely in the blood and then block the lumen of the vessel. This can cause unpleasant complications such as:
- Myocardial infarction. In this case, blood circulation in the coronary vessels completely stops, the cells and muscles of the heart quickly die due to oxygen starvation.
- Pulmonary embolism. The blood flow in them is disrupted, which even with timely resuscitation is very life-threatening.
- Sudden death.
- Injuries to the lower extremities that can lead to disability.
When a vessel is blocked, circulation is impaired, causing swelling with progressive tissue necrosis and oxygen deprivation. If left untreated for a long time, it can cause coma and death.
Risk factors for thrombosis
Internal:
- arterial hypertension [7];
- pregnancy, childbirth, postpartum period [3];
- biochemical changes in blood [2,3,5,7];
- vasculitis [2];
- age over 40 years [5];
- congenital thrombophilia, thrombosis, varicose veins of the lower extremities [3,5];
- congestive heart failure [5, 6];
- malignant neoplasms, radiotherapy and chemotherapy [3];
- strokes [3, 6];
- myeloproliferation [2, 5, 7];
- nephrotic syndrome and renal failure [5, 6, 7];
- obesity (BMI over 30) [3];
- myocardial infarction [6];
- diabetes mellitus [6, 7];
- systemic lupus erythematosus [2];
- chronic pulmonary diseases [3];
- enterocolitis [5].
External:
- heroin addiction [2];
- hormonal therapy [3,5];
- dehydration due to vomiting, diarrhea, increased sweating, direct lack of fluid [6];
- immobilization [3];
- travel by plane, bus or in a seated car [3];
- infectious diseases, including COVID-19 [1, 3, 5, 9];
- catheterization of central and peripheral veins [2, 5];
- smoking [6, 7];
- sedentary lifestyle [3];
- operations [3];
- fractures of large bones, other injuries [3];
- taking oral contraceptives [5];
- taking Diazepam, Amiodarone, Vancomycin [2];
- sclerotherapy and thermal ablation [2];
- condition after joint replacement [3];
- holding an awkward position [3].
Reasons for separation
The blood clot is tightly bound to the wall of the artery or vein, but breaks due to triggers. This usually happens unexpectedly and can cost you your life. What causes the clot to break off:
- High blood flow speed.
- Increased body temperature during an infectious disease.
- High blood pressure.
- Physical or mental stress.
- Vascular diseases in the area where the clot is located.
- High pressure during contraction of the heart muscle, this is characteristic of clots on the valve leaflets.
- Large clot size.
Indications and contraindications for the treatment method
- Acute arterial embolism - blockage of an artery by a blood clot brought from other places. The most common procedure is open embolectomy with a Fogarty probe through an approach below or above the blockage.
- Arterial thrombosis against the background of atherosclerotic plaques (atherothrombosis). It is dangerous to use a Fogarty probe in this case, as the artery wall may collapse. Rotarex allows you to remove thrombotic masses from an artery affected by atherosclerosis without damaging the vascular wall. In addition, soft atherosclerotic plaques are cut off. After removing the thrombus, angioplasty and stenting of the affected arteries are necessary.
- Removal of blood clots from vascular prostheses. Can be performed from open approaches using various modifications of Fogarty catheters. Most often, blood clots are removed from large vascular prostheses (aorto-femoral) as part of repeated operations.
- Removal of blood clots from previously installed stents. Stent thrombosis often requires repeated interventions. It is not possible to use a Fogarty balloon to remove blood clots from stented areas of arteries, as it will rupture against the stent or damage the arterial wall. For such thromboses, it is much more effective and safer to use Rotarex technology.
Signs of separation
When a clot breaks off and blocks a coronary vessel or artery of the heart, the patient's condition worsens significantly and it is immediately destroyed:
- Blood pressure drops to life-threatening levels.
- Cyanosis appears.
- Breathing is impaired, a feeling of suffocation appears.
If a clot breaks away from the left ventricle, a stroke occurs. If the clot passes through the right atrium, there is a risk of thromboembolism.
- If a blood clot blocks a blood vessel in the brain, it results in an ischemic stroke. The patient suffers from speech and vision impairments and paralysis.
- A blockage in the jugular vein in the neck causes severe dizziness, headache, blurred vision and loss of consciousness.
- If a clot enters a coronary artery, it causes acute myocardial infarction, shock, and severe pain.
- If the renal artery is blocked, lower back pain develops and the flow of urine becomes difficult.
- Embolism of the mesenteric vessels is manifested by peritonitis, necrosis of intestinal loops, severe pain, and flatulence.
- When the arteries of the extremities are blocked, bluish skin, pale skin, bleeding in the area, lack of response to touch, and a decrease in temperature at the site of injury are observed. Gangrene may develop with risk of amputation.
conclusions
Today, the prevention and treatment of cardiac thrombosis is an advanced area of cardiology. The process of thrombus formation itself has two sides: on the one hand, protecting the body from large blood losses, on the other, the occurrence of serious diseases with the risk of death. Therefore, it is necessary to know what diseases lead to the pathological formation of blood clots, symptoms and possible complications of cardiac thrombosis in order to receive medical help in time and have a chance for a full recovery.
First aid
If you notice the first signs of a clot dislodging, you must urgently call an ambulance, since it is impossible to provide professional help at home. The team will immediately start you on anticoagulants such as heparin. Enoxaparin, Nadroparin, Dalteparin. You should not inject them yourself as this may cause serious bleeding.
To get rid of existing clots, the patient is prescribed fibrinolytic drugs. These are: fibrinolysin, thromboflux, streptokinase. If necessary, the clot is removed with a catheter. If the patient falls into a coma, artificial ventilation and cardiac arrest.
Chances of helping the victim
Saving a person with a violin clot is only possible with timely help. A general blockage of the vessel can cause death within minutes.
Diagnosis of a blood clot in the heart
Typically, in cases of suspected cardiac thrombosis, laboratory and instrumental tests are put into operation. Based on the results, the doctor draws conclusions and prescribes treatment.
Among the instrumental methods they are popular:
- Ultrasound examination of the heart.
- Ultrasonographic examination of the abdominal cavity.
- Echocardiography.
- Radiography. It is necessary to exclude myocardial muscle hypertrophy, aneurysm, demonstration cardiomyopathy and thrombolites.
- Scintigraphy, which helps to see vascular disorders and their location, shows the percentage of myocardial filling.
- Doppler ultrasound, which measures the direction and speed of blood flow as the heart shrinks, shows the pressure in the heart.
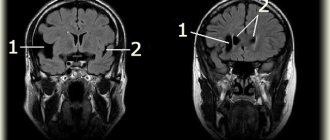
- MRI. With its help you can recognize cancer and determine the functionality of the myocardium.
Left ventricular (LV) thrombosis and thromboembolic syndrome (TES), occurring in dilated cardiomyopathy (DCM) with low cardiac performance, are registered in 10-44 and 4-18% of cases, respectively [5, 12, 14-16]. The incidence of these complications is determined by disorders of myocardial contractile function. This is why the study by E. Loh et al deserves special attention. [19], which noted that in patients with post-infarction cardiosclerosis and an ejection fraction equal to or less than 28%, the risk of ischemic stroke was almost 2 times greater than in patients with an ejection fraction of more than 28%; Moreover, every 5% decrease in this indicator was accompanied by an 18% increase in the incidence of acute cerebrovascular accident (ACVA). The presented data indicate the extreme importance of timely diagnosis of these complications and selection of optimal medical tactics.
RNTSKh them. acad. B.V. Petrovsky has experience in the surgical treatment of 70 patients with pseudotumor space-occupying lesions of the heart [2]. 26 (37.1%) of them had parietal (21 observations) or valvular (5) thrombi of the right (17) or left (9) parts of the heart. Only 3 (4.3%) patients had thrombi in the left ventricle (LV). Their dimensions in 2 patients were 1.5×3.0 cm or 2.0×3.0 cm, and in 1 patient, whose medical history is presented below, the thrombus reached gigantic sizes.
Patient A.
, 43 years old, hospitalized at the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky on 04/27/16 with a diagnosis of DCM, LV thrombus, recurrent TES.
He considers himself sick since September 26, 2005, when for the first time, due to acute pain in the lower extremities, he underwent thrombectomy from the left iliofemoral segment with autovenous grafting of the common femoral artery (CA) at the Regional Clinical Hospital of Vladimir, and on November 3 of that same year at the Military Medical Academy named after. CM. Kirov St. Petersburg - left-sided lumbar sympathectomy. After discharge on November 12, 2005, a short-term episode of loss of consciousness and dysarthria occurred; the patient was hospitalized at the Murom Central District Hospital, where he was treated for stroke in the middle cerebral artery on the left. In June 2007, he was treated at the Department Hospital at Murom station due to gastrointestinal bleeding and extensive subcutaneous hemorrhages that occurred while taking warfarin; The patient was prescribed ACC thrombosis. Due to another deterioration of the condition, on June 23, 2008, at the Road Clinical Hospital at Gorky station, an open endarterectomy was performed from the left OBA with revascularizing osteotrepanation, and on March 24, 2016, at the First Moscow State Medical University named after. THEM. Sechenov - bifurcation aortofemoral bypass with Polythese prosthesis with profundoplasty of the deep femoral arteries on both sides. It should be noted that coronary angiography (CG) revealed a left type of blood supply to the heart, 70% stenosis of the distal segment of the circumflex artery; During transthoracic echocardiography (EchoCG), a space-occupying lesion in the left ventricle was registered. For further surgical treatment, the patient was sent to the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky.
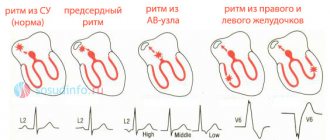
Electrocardiography (ECG) recorded sinus rhythm (SR) with a heart rate (HR) of 88 per minute, a horizontal position of the electrical axis of the heart, and a violation of intraventricular conduction.
X-ray of the chest organs demonstrated the absence of pathological changes in the lungs, the heart is not enlarged in size, the diaphragm is located normally and is mobile; there is no fluid in the pleural cavities.
Transesophageal echocardiography (TEE) (Fig. 1) revealed a hyperechoic space-occupying formation (thrombus of varying degrees of organization) measuring 2.0×7.4 cm in the LV cavity, emanating from its apex on a wide base. The neoplasm had an oblong shape, scalloped edges, located along the LV cavity, occupying 35-40% of its volume; There was moderate flotation of the thrombus in the projection of its upper part. Dense fibrous cords extended from the anterior surface of the space-occupying lesion to the interventricular septum (IVS). Its upper pole was located 1.6-1.8 cm from the cusps of the aortic valve (AV), and the anterior cusp of the mitral valve (MV) was in contact with its upper floating part in diastole. Noticed: rounding and expansion of the LV apex, pronounced diffuse hypokinesis; in the area of the IVS and the anterior wall of the LV - hypo- and akinesis. LV end-diastolic volume (EDV) was 195 ml, LV end-systolic volume (ESV) was 135 ml, LV ejection fraction (EF) was 25.8%.
Rice. 1. Transesophageal echocardiography of patient A., 43 years old. Diagnosis: space-occupying formation (thrombus) of the left ventricle.
Magnetic resonance imaging (MRI) (Fig. 2) registered a volumetric formation (thrombus) of the LV, emanating from its apex, measuring 1.8×6.6 cm. It was not fixed to the papillary muscles, was in contact with the anterior leaflet of the MV, not accumulated contrast agent. Attention was paid to intraoperative fibrous changes, hypokinesis of the IVS and the anterior wall of the LV.
Rice. 2. MRI of patient A., 43 years old. Diagnosis: space-occupying formation (thrombus) of the left ventricle.
The blood levels of carcinoembryonic antigen, α-fetoprotein, and carbohydrate antigens CA-19−9 and CA-72−4 were within normal limits.
On 05/10/16, a LV thrombus was removed from a transsternal approach under conditions of hypothermic perfusion (duration 90 min) and cold pharmacological cardioplegia with Custadiol (duration 67 min).
The following features were noted intraoperatively. After ventriculotomy performed through the apex of the LV, an oblong-shaped neoplasm measuring 2.5×7.0 cm, emanating from its apex, was revealed. It was partially fixed to the IVS and the lateral wall of the LV. The tumor was removed en bloc (Fig. 3). The left ventricle is sutured with a double-row suture on Teflon pads. The control TEE revealed a fragmented section of thrombus in the left atrium (Fig. 4). A left atriotomy was performed parallel to the interatrial groove. A fragmented section of the thrombus measuring 1.5×2.0 cm was removed. After removing the clamp from the aorta and warming the patient, ventricular fibrillation occurred; S.R. was restored with a single defibrillation. Repeated control TEE demonstrated the absence of intracavitary neoplasms, a decrease in LV EDV and LV ESV to 130 and 69 ml, respectively, and an increase in LV FI to 46.9%.
Rice. 3. Intraoperative scene of a removed left ventricular thrombus.
Rice. 4. Transesophageal echocardiography of patient A., 43 years old. Diagnosis: condition after removal of a left ventricular thrombus, a fragmented section of the thrombus in the left atrium.
Histological examination confirmed the diagnosis of a massive partially organized fibrinous thrombus with foci of calcification.
The subsequent immediate postoperative period proceeded without complications. The patient was discharged from the Center in satisfactory condition on the 8th day after surgery.
Analysis of the literature indicates that intracardiac thrombosis, in particular LV thrombus, and thromboembolic syndrome can occur with DCM, acute myocardial infarction (AMI) or LV aneurysm, acute myocarditis, antiphospholipid or hypereosinophilic syndromes, amyloidosis, Behcet's disease, Chagas disease [ 4, 7, 11, 13, 18, 21, 27]. The pathophysiological mechanism that explains the occurrence of the pathology in question is Virchow’s triad, represented by damage/dysfunction of the bloodstream wall, blood stasis, systemic or local hypercoagulation [1]. Considering the life-threatening nature of thrombosis of various chambers of the heart and subsequent thromboembolic complications, the clinical significance of its early diagnosis and selection of optimal medical tactics is obvious.
EchoCG is a highly effective non-invasive method for diagnosing space-occupying cardiac lesions. Its sensitivity and specificity in detecting LV thrombus are 92–95 and 86–88%, respectively [24, 28]. It should be noted that registration of false negative or false positive results with this research method may occur with small tumors not exceeding 0.5-1.0 cm in diameter, or due to the difficulty of differential diagnosis with anatomical and topographical features (papillary muscles, trabecular and tendon structures) of the left ventricle. In this regard, in such situations, it is recommended to use TEE, the sensitivity and specificity of which in diagnosing intracardiac thrombosis reaches 92-100 and 98-100%, respectively, or EchoCG using echo contrast agents, providing 100% diagnosis and differential diagnosis between thrombosis and neoplasms [3 , 6, 20]. An alternative research method in such cases may be contrast-enhanced MRI, the sensitivity and specificity of which are 88 and 99%, respectively [23]. As for angiocardiography, given its sensitivity and specificity, which are 63 and 67%, respectively, as well as the risk of thrombus fragmentation and thromboembolic syndrome, this research method is currently abstained [25].
Medical tactics for intracardiac thrombosis can be represented by anticoagulant therapy, thrombolysis or surgical treatment. Each of these methods has its own advantages and disadvantages. As for the surgical treatment of patients with LV thrombosis, the indications for its implementation are the large size of the thrombus and its mobility, the thin “leg” of the thrombus, the presence of an aneurysm in the area of its origin, a history of systemic embolism [5, 8, 10, 18, 26 , thirty]. In these clinical situations, thrombectomy should be performed without delay. Moreover, in order to radically remove the thrombus and ensure simplicity of its technical implementation, it is advisable to perform the operation from the left ventriculotomy. At the same time, with low cardiac performance, it is necessary to take into account that this access to the thrombus can cause further deterioration in the contractile function of the LV. In such situations, it is advisable to use left atrial or transaortic approaches [9, 17, 22, 27, 29].
Thus, recurrent acute circulatory failure of the lower extremities, presented in this clinical observation, indicates the need to initially exclude cardiogenic embolism. That is why in such situations it is recommended to conduct TEE and/or MRI with contrast; After confirming the diagnosis of LV thrombosis and embolectomy from the affected vessel, immediate thrombectomy from the LV is necessary, most optimally performed by access from the left ventriculotomy under conditions of artificial circulation and cold cardioplegia.
The authors declare no conflict of interest.
Treatment of thrombosis
The choice of treatment depends on the patient's condition, location, size and coagulation. The doctor may recommend:
- Pharmacological treatment.
- Dieting.
- Normalized physical activity.
- Traditional drug agents.
- Surgical intervention.
Drug therapy
Conservative treatment can be used:
- Anti-aggregates. They reduce the density of the clot. These include acetylsalicylic acid, plavix, yolks, diparidamole.
- Anticoagulants: Rivoroxaban, Warfarin. It helps to break up the blood, effective in fighting huge thrombosis, in case of stroke and myocardial infarction.
- Thrombotic urgent clots: urokinase, prorokinase, altenePlase.
- Measures that improve fluid drainage.
- Anti-Turkish drugs: amiodarone, allopin. This helps reduce the risk of new blood clots.
Drugs that dissolve blood clots
Unfortunately, there is no medical evidence that blood clots can dissolve themselves. On the contrary, if the victim is not treated quickly, it can worsen his condition.
Thrombolytic therapy is recommended only in cases where the person is at high risk. The effectiveness is visible only in the initial phase of use for 3-6 hours. If therapy is started later, it will not be effective and may have a negative impact on the patient's health.
Thrombolic drugs are divided into several groups:
- Blood plasma therapeutics include plasmin.
- Plasminogen activators: streptokinase, urokinase.
- Related medications.
If the blood clot is in the artery, the drug will be discontinued; it must be continuously delivered to the body for 2-3 days.
Basic thrombolytic drugs:
- Streptokinase. Cheap drug, but often causes side effects and allergic reactions and has a low half-life.
- Urokinase. In this case, heparin must be given. The effectiveness of the drug is no less than the previous one.
- AnistrePlase. It is more expensive, but does not require heparin. This medication is given by nozzle and is often used in pre-hospital treatment.
- Alteneplase. An expensive drug, but more effective than streptokinase. Heparin is needed for 7 days. May cause brain hemorrhage.
Although thrombolysis helps dissolve the clot, this therapy causes many side effects, such as:
- Bleeding.
- Disruption of myocardial systolic function, which can lead to organ failure.
- The course of the hemorrhagic brain.
- Allergic reactions.
- Reperfusion array.
- Fever, chills, rash.
- Army hypotension.
- Close the coronary artery.
Thrombolism can be carried out in two ways:
- The drug is injected into the veins; if you do not know where the clot is, the drug is distributed throughout the bloodstream. The disadvantage is that the dose is too high for the patient, which increases the load on the entire body.
- This method involves giving the drug through a catheter. Professional personnel are required to perform the operation as this method is quite dangerous. The movement of the catheter is monitored by x-rays.
To prevent platelet aggregation, acetylsalicylic acid or ticlopidine is prescribed, which reduce fibrinogen levels.
Diet
To make treatment more effective, patients are advised to adhere to certain dietary restrictions. In addition, it is important to monitor your fluid intake throughout the day (should be at least 2 liters). Among vegetables and fruits, those that contain large amounts of fiber and vitamins are preferred.
The following should be excluded from the menu:
- Animal fats such as lard, butter, fatty meat.
- Smoked meats, sausages and frankfurters.
- Cream, sour cream, ice cream.
- Coffee, strong tea, carbonated drinks.
- Cookies, all confectionery products.
- Sauces and spices.
- Anything fried or fatty.
Change your diet:
- Fish, seafood.
- Low-fat dairy products.
- Grapes, dates.
- Beef liver.
- Soy.
- Seeds.
- Legumes, nuts.
- Citrus.
- Greenery.
- Berries.
Exercises
Very often, circulatory disorders caused by a long-term sedentary lifestyle lead to the formation of blood clots. To prevent this from happening, you should do a few simple exercises every day.
It is important that you can do gymnastics at any time of the day. Activation of proper blood circulation in the lower extremities and improvement of general blood supply.
- While standing, roll from your heels to your toes and back.
- Standing, we rise to a place and sharply lower ourselves onto our heels.
- We walk by bending our knees and lifting them high.
- Lightly pat each foot from bottom to top and massage gently in a circular motion. Avoid varicose veins.
- The legs should also be rubbed from bottom to top and then gently stroked to relax.
Traditional methods of treatment
Home medicine can be used during the period of remission, stopping an exacerbation and consolidating the effect; it does not replace drug treatment. Herbal teas, compresses and decoctions are commonly used.
- Chop chestnut fruits (100 g) and pour half a liter of vodka, set aside for 2 weeks in a dark place and take 20 drops 3 times a day for at least 1 month.
- Make a mixture of tinctures of hawthorn, valerian, thyme and peony in a volume of 125 ml, also add 40 ml of eucalyptus, mint and 10 ml of tincture of Corvalol and echinacea. Pour 8 crushed clove buds into this mixture and leave for 7 days. Take a teaspoon three times a day for a month.
- Add a finely chopped head of garlic and a glass of cold water to two crushed lemons. Refrigerate for three days, strain and drink 1 tablespoon 3 times a day.
- The collection consists of equal parts of hawthorn flowers and fruits, horsetail grass and knotweed. Pour 1 tablespoon of the mixture into a glass of hot water and let it brew for about an hour. Drink 70 ml 3 times a day for at least 1 month.
Surgery
If the clot breaks off or there is a high risk of its movement, elective surgery is performed.
Most often it is used:
- Coronary bypass surgery. This improves blood flow in the heart muscle by creating a new path around the blocked vessel. The patient's arteries are used as a shunt. Manipulations are carried out with an open heart.
- Stenting. A surgical stent is used to widen the heart vessels at the site of the blood clot.
Bibliography
- Consensus position of experts of the Eurasian Association of Therapists on some new mechanisms of the pathogenesis of COVID-19: focus on hemostasis, issues of blood transfusion and the blood gas transport system / G.P. Arutyunov, N.A. Koziolova, E.I. Tarlovskaya, A.G. Arutyunov, N.Yu Grigorieva, etc. // Cardiology. 2020;60(6). DOI: 10.18087/cardio.2020.5.n1132.
- Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev, B.V. Boldin, O.V. Jenina, V.N. Lobanov//Hospital-substituting technologies: Outpatient surgery. 2016.- 3-4 (63-64)- P.16-23.
- Modern problems of thrombosis of arteries and veins / I.N. Bokarev, L.V. Popova // Practical Medicine, 2014. - No. 6 (82) – P13-17.
- Treatment of thrombophlebitis. Current recommendations and clinical practice / P.F. Kravtsov, K.V. Mazaishvili, S.M. Markin, H.M. Kurginyan // Thrombosis, hemostasis and rheology, 2020 No. 2 – P 68-72.
- Venous thrombosis: modern treatment / P.S. Laguta // Atherothrombosis, 2015 - No. 2 - P. 7-16.
- Deep vein thrombosis of the lower extremities / A.K. Lebedev, O.Yu. Kuznetsova // Russian family doctor, 2015.
- National recommendations for the diagnosis and treatment of diseases of the arteries of the lower extremities, Association of Cardiovascular Surgeons of Russia, Russian Society of Angiologists and Vascular Surgeons, Russian Society of Surgeons, Russian Society of Cardiology, Russian Association of Endocrinologists, M, 2021.
- Diagnosis and pharmacotherapy of acute venous thrombosis / N.V. Sturov, G.N. Kobylyanu// Difficult Patient, 2013., No. 12., T. 11. –P.19-22.
- Principles of management of patients with venous thromboembolism during the COVID-19 pandemic // V.Ya. Khryshchanovich // Surgery News, 2021.- t28 No. 3 – P329-338.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Prevention of thrombosis
To prevent this disease, doctors recommend:
- Lead an active lifestyle.
- Eat a healthy diet.
- Avoid stress and physical activity.
- Give up bad habits.
- Get regular medical checkups.
- Do exercises daily.
- Drink at least 2-2.5 liters of fluid per day.
If the patient has already had intracardiac thrombosis, it is recommended:
- Visit your doctor every six months.
- Acetylsalicylic acid should be taken constantly.
- Wear compression garments to prevent varicose veins.
A blood clot in the heart is a serious pathology, since complete blockage of the vessel can cause instant death.
To prevent the development of the disease, you should control your diet, lead an active lifestyle, avoid stress and overload, and undergo preventive examinations with a cardiologist once every six months.
Rehabilitation after surgery
After thrombectomy, the patient will be able to return to a full life only after a couple of days. Next, drug treatment is carried out. The attending physician prescribes the following medications to the patient:
- blood thinner tablets,
- drugs that restore veins, blood vessels,
- ointments that prevent the formation of clots,
- vitamin and mineral complexes.
To avoid the development of complications after surgery, you should follow the advice of your doctor:
- maintain an active lifestyle,
- wear elastic clothes,
- maintain proper nutrition,
- carry out physiotherapeutic procedures,
- Avoid visiting bathhouses and saunas for a while.