Patent ductus arteriosus: causes, treatment, prognosis
The diagnosis of patent ductus arteriosus (PDA) is often made in premature infants. What does this diagnosis mean? Why does patent ductus arteriosus occur? Is surgery always necessary? We talked about this live on “The Right to a Miracle” with Grigory Valerievich Revunenkov
, Ph.D., Head of the Department of Innovative Diagnostic Research Methods, Ultrasound Diagnostics Physician at the Research Institute of Pediatrics and Children's Health, Central Clinical Hospital of the Russian Academy of Sciences.
What is patent ductus arteriosus?
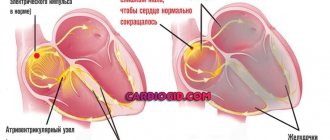
This is a defect that at one stage of the child’s intrauterine development is not a defect. This is one of the types of fetal communication: without an open ductus arteriosus (ductus arteriosus), the child does not develop in utero. Since the lungs do not participate in breathing, they are airless, high-pressure blood must be expelled somewhere. It is through this channel that it is discharged from the pulmonary trunk (which fills the lungs with blood) into the aorta - a vessel that extends from the left ventricle and is the largest vessel in our body.
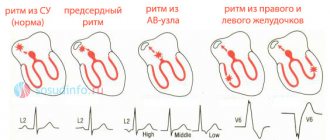
However, after the baby is born, this fetal intrauterine communication must close. Why? The lungs begin to work, and as soon as the concentration of gases in the blood changes after the first inhalation, the duct contracts (this is a kind of tube of a certain length, with walls with muscle fibers). The duct contracts and blood flow through it stops quite quickly.
However, at first, when the duct is closed, the opposite situation is also possible. For some reason, the muscles may relax and the duct may resume its activity. Why is this happening? For many reasons. Including when using certain medications. These may be very premature babies. It doesn’t make much sense to list all the factors.
What then happens to the patent ductus arteriosus?
There are medications that allow the duct to close. These are non-steroidal anti-inflammatory drugs that we use in everyday life - indomethacin, ibuclin, and so on. These drugs can close the duct in a small child. But only if the muscular apparatus, which is responsible for the spasm of this vessel, works correctly.
In cases where the duct is really large, or there is a non-drug reason why the duct remains open, sometimes it is necessary to decide on the operation directly in the incubator. But for this there must be certain conditions.
How is patent ductus arteriosus diagnosed?
Using a very popular tool now - echocardiography. This is an ultrasound examination of the heart. Abroad, it is not customary for everyone to undergo echocardiography. We also. It is done under a certain situation. When a child has pulmonary insufficiency, low saturation. At an early age, patent ductus arteriosus is very well treated. The time from birth to 1-3 months is the window of opportunity when most congenital heart pathologies can be seen. And the patent ductus arteriosus at this age is clearly visible. Unlike adults.
Where do adults with PDA come from? Echocardiography began to be used so widely relatively recently, about 15 years ago. So, those adults who were underexamined at one time may have a patent ductus arteriosus. And in children, sometimes at an older age, a PDA is discovered during medical examination.
When is patent ductus arteriosus operated on?
If he's big. If it leads to a pronounced disturbance of hemodynamics, this manifests itself in the early period, and the decision is made in the first days. If for some reason this was not required, the open ductus arteriosus is small in caliber, 1-2 mm, then such ducts are not closed immediately, but are left for later, since perhaps they will close on their own, or with medication. Surgery is not always necessary.
How complex is this intervention? How difficult is it to rehabilitate a child after this intervention?
If we consider it from the category of cardiac surgery, it is considered uncomplicated; it is one of the simplest operations. If we consider simply from medical surgical interventions, there is not a single intervention about which we could say that it is not very simple. Observing this defect, if we decide that its effect on the cardiovascular system can be considered stable, that is, it is not hemodynamically significant, we usually observe the duct until preschool age.
How is the operation performed?
The duct has a rather complex structure. The outlet is the trunk of the pulmonary artery - the effect on the state of the cardiovascular system depends on it, it calibrates it. There is an ampulla - this is the wide part on the side of the aorta. And there is its length - extension. All these three parameters force us to select one or another type of device for closing.
There are many options for devices that close the duct. Flipper is an elongated string made of metal with a memory effect, which, when entering the body, curls into a complex spiral and closes the duct. There are occluders that are specially configured - they are used to close more complex ducts.
The PDA is operated on through a small incision (traditional suturing) or endovascularly, through the femoral artery: a puncture is made, an instrument is inserted that closes this duct.
What happens if you do not close the patent ductus arteriosus?
Quite often there are small open arterial ducts, with a caliber of up to 1 mm or 1 mm or less, they are not hemodynamically significant. But there is one thing. It is customary to close them not because they play such a large role in hemodynamics, but because in the future the development of botalitis is possible.
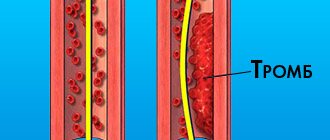
Botalitis is an inflammation of the botal duct, which can lead to certain complications. And this means thrombosis and the development of vegetation. This is the proliferation of bacterial colonies and occurs during severe bacterial infections: pneumonia of various etiologies, ENT infections, tonsillitis, periodontitis. In this case, treatment becomes quite unpleasant, because thrombosis occurs. This is no longer a simple operation to implant an occluder, but a large operation that forces us to excise the area where these vegetations have arisen, and the treatment takes on a larger scale.
That is, in those cases when we close these small ducts, we do not affect hemodynamics, but we, as it were, lay a straw for ourselves so that this difficult situation with botalitis does not arise. This is prevention.
Question from subscribers. Born at 34 weeks. Open duct 2 mm. We were monitored for up to a year and still sent for surgery. There are no other diseases. We don’t know whether we should still wait until preschool age?
We encounter this situation quite often. Each specific case must be considered separately. Sometimes children are brought in with a 3 mm patent ductus arteriosus. But we understand that there were 3 mm per month, and this is a hemodynamically significant duct. How did he get 3 mm at the age of 3-4-5? And when they deliver it, we measure it again and it turns out that they measure it in the wrong place. That is, not the part that calibrates the duct itself and influences its significance, but let’s say they measured it in the middle part. There really could be 4 or 5 mm. But the anastomosis with the pulmonary artery itself is a millimeter. Thus, this duct is hemodynamically insignificant and there is no need to rush.
The larger the caliber of the vessel through which we pass the device, the more convenient it will be not only for the operator, but also for the patient, because the vascular wall will be less injured. That's why we usually push it to 5-6 years, if possible. If it is impossible, this is a different situation, then it means we need to operate. To the point that if it is not possible to operate endovascularly, then it is necessary to use the open method. When indicated, I repeat.
What are the long-term consequences of patent ductus arteriosus? Does this manifest itself somehow in the future?
Yes, sure. One of the consequences is the development of botalitis. The second situation is when a hemodynamically significant duct is missed for some reason; this also occurs. In this case, in the future we may encounter the development of pulmonary hypertension. The excess volume of blood that will enter the pulmonary circulation will lead to an increase in pressure in it, as a result, the walls of the vessels that go to the lungs will become denser. The vessels become unable to maneuver, namely to expand or narrow. And this is the so-called pulmonary hypertension. The fourth stage of pulmonary hypertension is characterized by the fact that the person is difficult to help and is practically inoperable. Eisenmenger syndrome develops: as soon as we reduce the pressure in the pulmonary circulation, this will lead to a crisis in the pulmonary circulation. The vessels are not able to operate at a pressure lower than before. And with high blood pressure, pulmonary edema develops. Unfortunately, there is only one treatment here - a lung transplant. This is a very difficult situation.
Therefore, PDA must be observed. A month or three months of a child’s life is a window of opportunity when we can see those nuances that, for one reason or another, we will not be able to see at an older age. It’s quite difficult to watch a one-year-old child. Young children at this age are already beginning to be aware of themselves and those around them, and to make certain demands on them. They may not want to lie quietly, they will scream, struggle, and when screaming it is very difficult to explore, because the signal that we receive turns out to be so noisy that sometimes it is impossible to see anything. And at one month the children are quite calm. At least you can feed them.
What are the clinically significant dimensions of the duct?
There is no direct correlation between the diameter of the duct and the clinical situation. Depends on many factors. What period of life - newborn or later period. How mature are the child's lungs? There are a lot of factors. But if the duct is 3 mm, then it is monitored very carefully in the maternity hospital. It’s just that few people do echocardiography in the first days in the maternity hospital. Shortage of specialists, shortage of equipment. But they always call a specialist, even from another institution, if there is a clinical need. It occurs when saturation drops, when cardiopulmonary failure is diagnosed.
And so, there are different situations: at my appointment there was a girl whose diameter of the patent ductus arteriosus was 9 mm at the age of five. She had Eisenmenger syndrome and, unfortunately, we were unable to help her. There was a boy with a similar situation. But in the modern world this is casuistry and, in theory, this should not happen. With early diagnosis, children could be helped.
What are the risks of occluder placement surgery?
The risks of implanting an occluder are minimal. To do this, there must be a good diagnostician and a specialist who will install this occluder must work with it in tandem.
My son has a clip in his heart. Will anything need to be done with it in the future?
The clip is titanium and remains in the body for life. Questions arise when they are about to undergo magnetic resonance imaging. Yes, the clip is made of non-magnetic titanium material. But non-magnetic materials heat up in a high magnetic field. Therefore there are certain restrictions. In an MRI study, it is believed that if the body has various metal devices (stents, for example), one can remain in the active phase of the study for 15 minutes without harm to health.
The child has a patent ductus arteriosus, but no treatment was prescribed. We are 8 months old, born at 31 weeks weighing 1650 grams. Should I take my child to another doctor?
A second opinion is very good. But since the size of the duct was not indicated, most likely this duct is hemodynamically insignificant, and the doctor decided that it was necessary to observe. And drug treatment at this stage is not necessary. If there is even the slightest doubt, they must be resolved.
You
–
Head of the Diagnostic Research Department.
How fast is technology developing in this area? Just like computers. Development occurs in parallel. Miniaturization, complication, increase in diagnostic confidence. If earlier it was hard to see and only a diagnostician with experience could say that there should be something based on certain signs, now diagnostic confidence is greater, because it is visible better, and the angle can be more conveniently selected. Because the sensors themselves, the devices themselves, are more convenient. Experience is still important though. But in some situations, if you are not entirely sure, you can order another study.
Endovascular closure of patent ductus arteriosus using an occluder
Introduction
Patent ductus arteriosus (PDA) is a congenital heart defect (CHD) characterized by the presence of abnormal vascular communication between the aorta and the pulmonary artery
In the prenatal period, everyone has a PDA; this is a normal component of the fetal circulation. After the first breath of the born child, the pulmonary vessels open, the pressure in the right ventricle drops, the PDA gradually ceases to function and closes (obliterates). Obliteration of the duct occurs at different times. In 1/3 of children it closes by two weeks, in the rest - within eight weeks of life.
Hemodynamic disorders are associated with abnormal discharge of blood from the aorta to the pulmonary artery, since the pressure in the aorta is much higher than in the pulmonary artery.
The volume of blood discharged depends on the size of the duct. As a result of circulatory disorders, a smaller volume of blood enters the systemic circulation than it should, which affects vital organs (brain, kidneys), and skeletal muscles. Passing through the vessels of the lungs, this blood returns to the left atrium, the left ventricle, which, experiencing excessive load, increase in size (hypertrophy), then, under the influence of an ever-increasing volume of blood supersaturated with oxygen, changes occur in the vessels of the lungs and pulmonary hypertension occurs.
Manifestations and natural course of the defect
Children are born with normal body weight and length. Further manifestations of the disease are related to the size of the duct. The shorter and wider the PDA, the greater the volume of blood discharged through it and the more pronounced the clinical picture of the disease. With narrow and long PDAs, sick children are no different from healthy ones. The only sign indicating the presence of congenital heart disease is a murmur heard by the pediatrician over the heart area. With wide and narrow PDAs, already in the first months and even days of the child’s life, all the symptoms (manifestations) of the defect can be detected. Such children experience constant pallor; during physical activity (straining, sucking, screaming), transient cyanosis (blue skin tint) is noted, mainly on the legs. Children are lagging behind in physical development. They have a tendency to recurrent bronchitis and pneumonia.
The most difficult periods during the course of the defect are the adaptation phase during the newborn period and the phase of terminal pulmonary hypertension in older children. During these periods, children die from heart failure, cerebrovascular accidents (stroke), pneumonia, and infective endocarditis. The average life expectancy for a PDA without surgical treatment is 25 years, although many patients with a narrow and long PDA live to old age. If an adult patient with a PDA develops signs of circulatory decompensation, surgery to close the duct is also recommended.
Treatment
There are two methods of treating PDA: conservative, or medicinal, and surgical. Drug treatment of PDA is used only in the maternity hospital for newborns during the first two weeks of life; later it becomes ineffective. This method is not always effective and has many contraindications, so the main treatment is mechanical closure of the duct.
Previously, the most common intervention was ligation of the duct after thoracotomy. Nowadays, the operation of PDA ligation is performed very rarely. Endovascular occlusion of the PDA has taken on a leading role. The essence of the intervention is to occlude (close) the duct with specially made spirals and occluders. The technique has almost no complications; it is performed on young children under general anesthesia, and on teenagers and adults under local anesthesia. Access is carried out by puncture, through the femoral artery. The effectiveness of the operation is almost one hundred percent; recanalization of the PDA is occasionally observed, which is subsequently eliminated in the same way. For wide and short PDAs, when endovascular occlusion of the PDA with coils is technically impossible, the PDA is closed using specially designed occluders, which are also delivered through the femoral artery.
Description of a clinical case.
Patient S, 67 years old, was admitted to the inpatient emergency department on September 18, 2017 with a diagnosis of congenital heart disease: patent ductus arteriosus (diameter 4 mm, length 13 mm). Upon admission, he complains of weakness and shortness of breath when walking. He has a history of hypertension with a maximum increase in blood pressure up to 200/100 mmHg, adapted to 140/80 mmHg. Takes Concor, amlodipine, Torvacard. Over the course of a year, he has noticed the appearance of shortness of breath when walking. During examination, according to ECHO data, congenital heart disease was detected: patent ductus arteriosus, signs of moderate pulmonary hypertension. According to MSCT data, the diameter of the ductus arteriosus was 4 mm.
Considering the deterioration of health and the appearance of pulmonary hypertension, a decision was made to perform transcatheter closure of the PDA.
Description of the operation (09/22/2017)
The right common femoral artery and common femoral vein were punctured under local anesthesia. A diagnostic catheter was inserted into the thoracic aorta. Angiography was performed and a patent ductus arteriosus connecting the aorta and pulmonary artery was visualized. Next, through the introducer in the right OBV, a catheter is inserted through the guidewire through the ductus arteriosus into the descending aorta. The catheter was replaced with an occluder delivery device. An Amplatzer Duct Occluder was implanted with the distal occluder disk located on the side of the aorta, and the proximal one on the side of the pulmonary artery. On control angiography, the position of the occluder in the ductus arteriosus is optimal, and a reduction in blood flow through the ductus arteriosus is noted. A good angiographic result was obtained.
The next day the patient was discharged from the hospital in satisfactory condition.