Blood flow speed is the speed of movement of blood elements along the bloodstream in a certain unit of time. In practice, experts distinguish between linear velocity and volumetric velocity of blood flow.
One of the main parameters characterizing the functionality of the body’s circulatory system. This indicator depends on the frequency of contractions of the heart muscle, the quantity and quality of blood, the size of blood vessels, blood pressure, age and genetic characteristics of the body.
Types of blood flow speed
Linear speed is the distance traveled by a blood particle through a vessel over a certain period of time. It directly depends on the sum of the cross-sectional areas of the vessels that make up a given section of the vascular bed.
Consequently, the aorta is the narrowest section of the circulatory system and has the highest blood flow speed, reaching 0.6 m/s. The “widest” place is the capillaries, since their total area is 500 times larger than the area of the aorta, the blood flow speed in them is 0.5 mm/s. , which ensures excellent exchange of substances between the capillary wall and tissues.
Volumetric blood flow velocity is the total amount of blood flowing through the cross-section of a vessel over a certain period of time.
This type of speed is determined:
- the difference in pressure at opposite ends of the vessel, which is formed by arterial and venous pressure;
- vascular resistance to blood flow, depending on the diameter of the vessel, its length, and blood viscosity.
Fundamentals of hemodynamics: factors determining the movement of blood through the vessels
From a mechanical point of view, the circulatory system represents a hydraulic network. It contains chamber pumps with valves (right and left heart) and extensible tubes through which a viscous liquid—blood—flows.
Both the heart and blood vessels are capable of changing their geometric and mechanical characteristics under the influence of physical, physiological and biochemical factors. One of the main indicators of blood movement through the vessels - volumetric blood flow velocity - Q can be calculated using the formula:
The volumetric velocity of blood flow is the same in different regions of the vascular bed and is 4-6 l/min. The linear speed of blood flow in the aorta is maximum – 50 cm/sec, in the capillaries – 0.07 cm/sec, in the vena cava – 33 cm/sec.
These formulas are taken from hydrodynamics; they do not take into account the unevenness of blood flow inside the vessel, the presence of eddy currents, heterogeneity of blood, etc. However, they are useful for a simplified assessment of blood flow. They formalize the main physiological factors that determine the movement of blood through the vessels.
- Pressure difference (the main factor without which blood movement is impossible).
- Peripheral resistance. It consists of the following components: the tone of resistive vessels, blood viscosity, hydrostatic pressure.
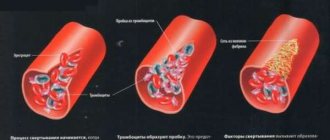
There is a term called effective blood viscosity, or the viscosity of moving blood in a vessel. It is determined by the force of friction of blood against the walls of the vessel and its layers relative to each other. Shear stress is the force of interaction between moving layers of liquid, which decreases with increasing linear speed of blood flow (Fig. 1).
At low blood flow speeds, the effective viscosity increases due to a decrease in the gradient and can increase 8-10 times in small vessels with low blood flow speeds. The latter does not apply to capillaries, in which the effective viscosity decreases due to changes in erythrocyte aggregation.
At high blood flow speeds, viscosity increases sharply due to the transition of the laminar type of fluid flow to turbulent (Fig. 2). This process is most pronounced in places of branches and sharp bends of blood vessels (aortic arch, branching of the carotid arteries, etc.).
In this case, the friction force of the liquid layers and, accordingly, viscosity increase sharply (possibly with muscular work and anemia). The value of blood pressure is an important indicator of hydrodynamics. The main factor in the movement of blood through the vessels is the pressure difference. It is actively created in the arterial system by the work of the heart. As the circulatory system progresses, the pressure decreases, being maximum in the aorta and minimum in the vena cava.
Factors that determine blood pressure.
- Work of the heart.
- Circulating blood volume.
- Vascular tone.
- Elasticity of blood vessels.
- Blood viscosity.
When assessing blood pressure, the following indicators are used:
- P max. or systolic;
- R min. or diastolic.
Blood pressure is determined by two groups of methods: direct and indirect. Indirect methods include the Korotkoff auscultatory method and the Riva-Rocci palpation method. Direct measurement of blood pressure is carried out using a pressure sensor, which can be inserted into the artery cavity or connected to it using special catheters.
Features of venous blood flow. Veins are low-pressure vessels; in relation to blood flow resistance, the resistive function is weakly expressed, but the capacitive function is strongly expressed.
Morphologically different from arteries:
- less mass of smooth muscle tissue of the vascular wall (the circulatory layer is less pronounced than the longitudinal one);
- lack of a round cross-sectional shape and the ability to collapse (collapse) at low venous pressure;
- strong dependence of elasticity on stretching;
- greater dependence of diameter on pressure;
- the presence of valves that prevent the reverse flow of blood (Fig. 3).
Functionally different from arteries:
- the ability to change the lumen without changing venous pressure;
- lower intravascular pressure and larger total volume;
- great influence of extravasal pressure on blood flow.
Functions of veins:
- Drain blood away from organs and tissues.
- Up to 70% of the blood is deposited for further use.
- Regulate venous return to the heart and blood pressure.
- Transcapillary exchange is regulated by changing the ratio of pre- and postcapillary pressure.
- Participate in exchange with surrounding tissues.
- Perform the function of an extensive reflexogenic zone.
- Participate in the implementation of immune control.
Auxiliary factors for the movement of blood through the veins:
- the presence of valves prevents the reverse flow of blood,
- dynamic contractions of skeletal muscles help push blood through the veins,
- suction action of the chest,
- suction effect of the heart (effect of displacement of the atrioventricular septum during ventricular systole),
- rhythmic contractions of the veins themselves.
Disturbances in venous blood flow can lead to pathological venous stasis of blood, decreased venous return to the heart and a drop in blood pressure. Venous congestion can occur with heart failure.
Microcirculation and transcapillary exchange.
The most important components of microcirculation, ensuring tissue homeostasis, are:
- blood movement in capillaries and adjacent microvessels;
- movement of lymph in the initial parts of the lymphatic system;
- movement of intercellular fluid.
The microcirculation zone includes: arterioles, precapillary arterioles, capillaries, postcapillary venules, venules and arteriolovenular anastomoses.
The basis of the microcirculation zone is the capillary. By structure they are distinguished:
- capillaries with a continuous wall (formed by a continuous endothelial layer, pores with a diameter of 4-5 nm, few large pores);
- capillaries with a fenestrated wall (in the endothelial layer there are windows with a diameter of 0.1 microns, common in the kidney, intestinal mucosa);
- capillaries with a discontinuous wall (present in the liver, spleen, red bone marrow; blood cells can pass through breaks in the endothelial layer).
The total cross-sectional area of all capillaries is 11000 cm2, the number of capillaries is 40 billion. The total exchange area of the capillary network is 1000 m2, or 1.5 m2 per 100 g of tissue. The density of the capillary network in tissues is different (in the brain – 3000 caps/mm3, in tonic muscles – 1000 caps/mm3, in phasic skeletal muscles – 300-400 caps/mm3). In actively working muscles, the density of the capillary network increases.
The movement of blood in microvessels has a number of differences associated with the small diameter of the capillary (from 4 to 20 microns, but usually 7-8 microns). The speed of blood movement (estimated by the speed of movement of red blood cells) is different, the blood flow is not stationary. When moving, blood cells line up strictly one after another; red blood cells, when moving through capillaries with a small diameter, can change their shape.
When the tissue is active under conditions of physiological rest, some of the capillaries are open. Their number increases 2-3 times with working hyperemia.
The opening of capillaries is regulated by tissue oxygenation: at high PO2 values (50-60 mm Hg), the number of functioning capillaries is reduced by 2 times, and at maximum oxygen tension in the tissues (100 mm Hg), all exchange capillaries close and blood flows through arteriovenular shunts.
Transcapillary exchange is ensured by the following processes: diffusion, filtration and reabsorption.
Diffusion. Consists of the movement of water-soluble substances of low molecular weight through water-filled pores.
Filtration and reabsorption. During the filtration process, blood intensively exchanges water and water-soluble components with tissue fluid. There is a dynamic equilibrium between the volume of fluid that passes into the intercellular medium from the plasma at the arterial end of the capillary and the volume of fluid that flows back into the blood during the process of reabsorption. Both processes are associated with hydrostatic and oncotic pressure gradients.
Importance and severity of the problem
Determining such an important parameter as blood flow velocity is extremely important for studying the hemodynamics of a specific section of the vascular bed or a specific organ. If it changes, we can talk about the presence of pathological narrowing along the vessel, obstacles to blood flow (parietal blood clots, atherosclerotic plaques), and increased blood viscosity.
Currently, non-invasive, objective assessment of blood flow through vessels of different sizes is the most pressing task of modern angiology. The success of solving it depends on the success of early diagnosis of such vascular diseases as diabetic microangiopathy, Raynaud's syndrome, various occlusions and vascular stenoses.
Why is blood velocity measured?
Measuring blood flow velocity is important for diagnostic medicine. Thanks to the analysis of data obtained as a result of measurements, it is possible to determine:
- vascular condition, blood viscosity indicator;
- level of blood supply to the brain and other organs;
- resistance to movement in both circles of blood circulation;
- microcirculation level;
- condition of the coronary vessels;
- degree of heart failure.
The speed of blood flow in vessels, arteries and capillaries is not constant and the same value: the highest speed is in the aorta, the smallest is inside the microcapillaries.
A fascinating “walk” through the veins and arteries
I bring to your attention an article about a medical diagnostic procedure - duplex scanning of blood vessels.
Duplex scanning of blood vessels, otherwise known as vascular Doppler ultrasound (USDG), is essentially an ordinary, familiar, well-known ultrasound scan.
Many patients undergoing medical examination are prescribed an ultrasound examination of the brachiocephalic vessels. I will try to talk about the essence of this study, what information it gives to your attending physician, and why this study was included in the list of diagnostic measures for medical examination of the adult population.
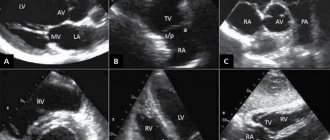
So, as a “tour guide,” I invite you to a short and, I hope, educational journey through the veins and arteries. The study is called duplex because it combines two modes - a two-dimensional image and a Doppler mode - a study based on measuring blood flow velocity. The 2D image looks like this.
This is a familiar black and white image, or rather gray, in which the manufacturers of modern ultrasound scanners promise not just 50, but as many as 256 shades! Doppler is a mode for studying blood flows, their speed and direction. It is the inclusion of the Doppler that is accompanied by the appearance of somewhat unusual sounds during the examination, sometimes slightly frightening to patients. These sounds are a kind of interpretation of the characteristics of blood flow. Each artery has its own “melody”. The external sleepy one is harsh and rough, the internal sleepy one is softer and more pleasant. And the veins generally “sound” like a light breeze.
This is what duplex scanning looks like on the monitor.
There is a color doppler that adds bright colors to a boring black and white picture. Patients, having seen the image, are usually interested in what is “red” and “blue” there?
Both “red” and “blue” are blood. The color depends only on the direction of blood flow relative to the sensor. What moves towards the sensor is colored red, what moves away from the sensor is colored blue.
This is no longer a duplex, but a triplex study. Actually, any modern ultrasound examination is triplex, but the name “duplex” has been preserved as more familiar.
Vascular examination is harmless to the patient, non-invasive (no penetration into the body) and does not require prior preparation. And now a little about the study of the brachiocephalic arteries (BCA), the same study that is included in the list of studies under the clinical examination program.
Brachiocephalic arteries is a definition that includes the carotid and vertebral arteries. The carotid arteries have nothing to do with the quality of sleep. They owe their unusual name to a small anatomical formation on the internal carotid artery. This formation, or rather the expansion of the artery, is called the carotid or carotid sinus. If you squeeze the neck in the area of this sinus, the number of heart contractions decreases, the person seems to fall asleep and may even lose consciousness. This is where the name carotid arteries comes from.
The examination is performed with the patient lying on his back, sometimes with a cushion under the neck for better vision of the arteries with the sensor.
This is what the common carotid artery looks like on an ultrasound scanner.
The carotid arteries can tell a lot of interesting things about a person. First of all, we are interested in the diameter and shape of the arteries, as well as the presence of atherosclerotic plaques that are dangerous to human health. The presence of atherosclerotic plaques or the predisposition of blood vessels to their appearance is indicated by such an indicator as the thickness of the “intima-media” complex or, in other words, the thickness of the inner layer of the vascular wall.
IMM thickness is an indicator of the severity of the atherosclerotic process in the body. Normally, it should be no more than 1.0 mm. The intima is a thin white stripe, the media is a thin black stripe following the intima, and the dark inside is the lumen of the artery.
The following image shows a vessel that is not affected by atherosclerosis. The thickness of the intima-media complex is 0.6 mm. The blue line is drawn along the inner layer of the vascular wall - the intima.
But in the next image, the intima-media complex, in other words, the vessel wall, is already thickened (1.4 mm) - these are already manifestations of atherosclerosis.
As atherosclerosis progresses, the intima-media complex not only thickens, but atherosclerotic plaques form, which cause narrowing (stenosis) of the vessel. The degree of stenosis is expressed as a percentage. Atherosclerotic plaques look something like this. This is the site of bifurcation (branching) of the common carotid artery (CCA) into its two branches - the internal carotid artery (ICA) and the external carotid artery (ECA). Arterial branching sites are favorite sites for the appearance of atherosclerotic plaques. I outlined the contours of the vessel itself in blue, and the atherosclerotic plaque in red. The degree of vasoconstriction in this patient is about 30%.
And in the next two pictures the process is already more advanced, the degree of narrowing of the vessel is 68%. The blue outline shows the vessel itself, and the red outline shows what the lumen of the vessel has become, changed due to atherosclerosis.
Atherosclerotic plaques can be extremely dangerous. Increasing in size, the plaque impairs blood flow in the vessel, up to its complete blockage. In addition, sometimes a fragment of atherosclerotic plaque can break off and block a smaller blood vessel, thus causing a stroke or heart attack.
If complicated plaques are detected and with a pronounced degree of narrowing of the vessel, a consultation with a vascular surgeon is indicated to decide on surgical treatment. If the process is moderate, the doctor prescribes treatment with statins - drugs that strengthen the surface of the plaque and prevent its destruction. It is also necessary to control your blood cholesterol levels, correct your diet and get rid of bad habits.
It is generally accepted that if atherosclerotic plaques are detected in the carotid arteries, then in the coronary arteries - those that feed the heart, there is almost one hundred percent probability that they are also present. We cannot easily and simply look into the arteries of the heart. Coronary angiography, the study of the blood vessels of the heart, is a complex study performed in a hospital setting. Therefore, ultrasound examination of brachiocephalic vessels (neck vessels) is a simple and informative method for diagnosing atherosclerosis. It is believed that atherosclerosis develops if a person has elevated levels of “bad” cholesterol - low-density lipoproteins.
To paraphrase popular wisdom, we can say that by the age of 50 every man should plant a tree, raise a son, build a house and... check his cholesterol level. It is advisable for a man who smokes to pay attention to his cholesterol by the age of forty. The same recommendations apply to representatives of the fair sex. In addition to the carotid arteries, vertebral arteries are also available for study. At the level of the sixth cervical vertebra, the vertebral arteries enter the bony canal formed by the transverse processes of the cervical vertebrae. Sometimes the artery enters the bone canal higher, at the level of the fourth or even third cervical vertebra.
The vertebral artery with a diameter of 3 mm is shown in the following image. Its walls are highlighted with blue lines. Dark vertical formations that interrupt the course of the artery are transverse processes of the cervical vertebrae. Ultrasound does not penetrate bone tissue, so the artery wall is not visible in these areas.
The vertebral arteries (VA) are smaller in diameter than the carotid arteries. The normal size is considered to be a diameter of 3 mm, if less than 3 but more than 2, this is called a “small” diameter, and less than 2 mm is already hypoplasia (underdevelopment) of the artery. This is a congenital condition, and it is impossible to influence the diameter of the arteries. When hypoplasia of the vertebral artery is detected on one side, the vertebral artery on the other side is usually increased in diameter. This ensures balance and ensures adequate blood supply to the brain. In addition to the diameter, we evaluate the shape of the arteries and the presence of tortuosity. The photo below shows an artery with a deformed course. It can be seen that the artery is curved, and this arc is painted in different colors.
Sometimes there are simply arteries curled into a ring! How can you avoid getting sick or dizzy with these? The vertebral vein runs parallel to the vertebral artery and above it in the bone canal. Blood in veins and arteries moves in different directions, so the vessels are painted in different colors.
Typically, the vertebral vein does not appear so bright and deep blue on an ultrasound. As a rule, it is slightly stained. Such brightness and expressiveness is already a bit of a pathology, which in conclusion is reflected in the phrase “difficulty of venous outflow.” This is not a disease yet, but rather a feature of the patient’s venous tone. But this condition already requires treatment, since it often manifests itself as tedious headaches and heaviness in the head. Remember what the doctor said from the movie “Formula of Love”? “The head is a dark object and cannot be examined.” A hundred years ago, maybe it was like that. Well, now it is very possible, and ultrasound examination of the brachiocephalic vessels (neck vessels) is an informative and safe diagnostic method that allows one to obtain important information about the blood supply to the brain.
It is enough just to do the research during medical examination. An ultrasound examination of the carotid and vertebral arteries at the second stage of clinical examination is prescribed to everyone who has elevated cholesterol levels or has complaints as prescribed by a neurologist.
Davidenko Yulia Gennadievna, head of the functional diagnostics office of the polyclinic of OKB No. 3.
Why is blood flow velocity measured in the vessels of the nail bed?
The speed of blood flow in the vessels of the nail bed is one of the clear indicators of the quality of blood microcirculation in the human body. The vessels of the nail bed have a small cross-section and consist not only of capillaries, but also of microscopic arterioles.
When there are problems related to the circulatory system, these capillaries and arterioles are the first to suffer. Of course, it is impossible to judge the state of the entire system solely on the basis of a study of blood circulation in the nail bed area, but it is worth paying attention if the blood flow in this area is too low or high.
In medicine, to obtain the most reliable information, measurements of blood circulation parameters are carried out over large areas of the blood circulation.