- Phlebology Center
- /
- About the clinic
- /
- Helpful information
- /
- Complications of varicose veins
If varicose veins are not treated at the initial stage, the disease will begin to develop and can lead to serious complications - thrombophlebitis and trophic ulcers. These forms of varicose veins have their own symptoms, which should also be paid attention to.
Why do my legs itch with varicose veins?
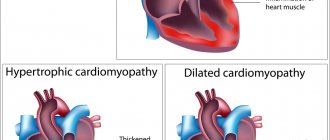
Varicose disease affects the valve apparatus of the veins and gradually leads to an increase in the diameter of the vessels. Dilated veins cease to cope with the function of transporting blood from bottom to top. Tissues and cells begin to experience oxygen starvation. Clinically, this manifests itself as pain and burning in the legs.
In this case, metabolic products are not excreted in a normal way, but accumulate in the intercellular space. Their excess leads to the development of unpleasant sensations in the lower extremities, including the appearance of itching. This is the reason why your feet itch.
If you do not influence the current situation in any way, then the itching will soon be accompanied by dryness and irritation of the skin, up to the development of trophic ulcers.
The appearance of lumps on the veins
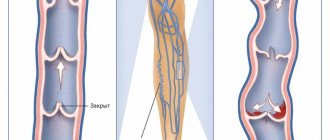
Varicose veins can progress in different ways - slowly or quickly. This process is accompanied by the appearance of new varicose veins, which look like bumps, protrusions on the skin in the area of the dilated vein. As they develop, varicose veins can be complicated by inflammation of the venous wall and the formation of a blood clot that clogs its lumen. The larger the size of the varicose vein, the higher the likelihood of a blood clot forming.
Many people imagine a blood clot as something separate, as a piece of something. It is not always so. If a blood clot forms in the lumen of the vein, then the already slow blood flow is blocked. It turns out that the vein turns into a blocked tube, and the blood above the blockage begins to clot. Thrombotic masses increase their length, the entire vein above the site of initial blockage is thrombosed.
If you do not seek professional medical help, thrombophlebitis becomes ascending. And since the saphenous veins connect to the deep veins, thrombotic masses can “grow” to them and at this stage a piece of the blood clot can break off and enter the heart and further into the pulmonary artery.
What treatment is needed if your legs itch due to varicose veins?
Modern treatment of varicose veins includes:
- Endovenous Laser Vein Coagulation or Radiofrequency Ablation. Both of these procedures are performed without anesthesia or open wounds. The patient is sent home immediately after the operation, since there is no need for round-the-clock medical supervision.
- If necessary, the above surgical treatment of varicose veins can be supplemented with Miniflebectomy, Echosclerotherapy of veins or Sclerotherapy. These are minimally invasive procedures aimed at achieving maximum effect.
- Gels and creams for temporary relief of symptoms.
- Medicines from the group of venotonics and angioprotectors.
- Compression jersey. Typically used after surgery to ensure proper blood circulation in the lower extremities.
Methods for treating itching
After a thorough examination and identification of varicose veins, a phlebologist in most cases will prescribe comprehensive treatment to the patient.
- The veins behind the knee hurt
Medications
For vein disease and if the veins in the arms and legs itch, the following medications help:
- Preventing the appearance of blood clots: Heparin, Warfarin.
- Ensuring the dissolution of blood clots: Streptokinase, Fibrinolysin.
- Relieving pain and reducing burning: Cetrin, Finistil.
- Calming character: Novopassit.
- Vitamins that improve blood circulation processes in general: Supradin.
- Normalizing the functionality of blood vessels: Detralex.
What not to do if your legs itch with varicose veins?
Let's look at the common mistakes that people with varicose veins make and complain that their legs itch with varicose veins. So, don't:
- Relieve symptoms with local therapy. Phlebologists believe that it is not advisable to use creams (antihistamines and anti-inflammatory) to relieve itching for a long time, since despite the fact that the legs itch less, the disease continues to progress.
- Resort to traditional medicine methods. If your veins itch, then homemade remedies can be not only ineffective, but also dangerous.
- Ignore the process and let it take its course. Scratching with varicose veins can become an open gate for infections and lead to inflammation of the skin of the legs.
- Wearing clothes that are too tight. If the trousers are too tight or touch the inflamed skin, then the legs itch even more.
- Resort to bloodletting and hirudotherapy. These methods have their place, but in case of varicose veins, you should treat them with caution and consult with a phlebologist before performing them.
If your legs constantly itch with varicose veins and this interferes with your life, then you should no longer delay treatment of the disease. Therapy will help you forget about itching and improve your quality of life. Moreover, varicose veins are treated painlessly, effectively and take virtually no time.
Causes of allergic reactions on hands
The main triggering factor for the development of allergic dermatoses is single or regular contact with the pathogen. In this case, treatment is aimed at completely eliminating the allergen to which the body is hypersensitive. It is quite difficult to determine, but among the most common causes of hypersensitivity are antigens from plants, animals, fungi, insects, foods, chemical compounds and drugs.
Also, allergic reactions on the fingers and other parts of the upper extremities occur due to:
- Gastrointestinal diseases. Diseases such as biliary dyskinesia, chronic gastritis and pancreatic dysfunction can trigger the development of allergic dermatitis and contribute to its transition to a chronic form.[3]
- Violation of the barrier function of the skin under the influence of mechanical, chemical and infectious agents. A broken epidermal barrier facilitates the penetration of allergens through the skin, the development of infection, and causes mild skin irritation.[7]
- Unfavorable environmental conditions. High levels of environmental pollution lead to an increased susceptibility of the population to allergic dermatoses.[8]
- Genetically determined factors. If both parents are prone to allergic diseases, the likelihood of developing neurodermatitis and other allergic dermatoses in the child is 70%.[9]
Causes of varicose veins
Blood circulates continuously in the human body; the heart, veins and arteries take a direct and constant part in this movement. Through arteries, blood moves from top to bottom, through veins, on the contrary, from bottom to top, to the heart. The blood moves upward in spurts, fixing itself in the places where the valves are located, and the valves, in turn, prevent the blood from returning back down. Thus, blood moves freely from one valve to another.
This movement of blood occurs with proper and complete functioning of the muscles of the lower extremities. But if the valve does not contract enough, then some of the blood returns down, which leads to an increase in venous pressure and subsequent dilation of the veins. The result is stagnation of blood in the veins.
What could cause valve malfunction?
The reasons may be both external factors and genetic disposition. The veins contract with the help of the muscles located around them. If a person has a sedentary lifestyle or a job that requires constant sitting, such as driving a car or office work, then the muscles become inactive and weak, which leads to poor circulation and, accordingly, to venous diseases.
External factors and causes of varicose veins can be:
- excess weight
- pregnancy
- taking hormonal medications
- menopause
- loads on the lower limbs
- sedentary lifestyle
- work that requires constant sitting (driving a car, office work)
- work that requires constant standing without the possibility of rest or change of body position (surgeons, teachers, salespeople)
- frequent wearing of high-heeled shoes
- wearing tight underwear
- Frequent carrying of heavy bags
- chronic digestive disorders (constipation)
— various concomitant chronic diseases (diabetes, cardiovascular diseases, kidney diseases)
Useful tips - what to do
To stop pathological processes in the body, to get rid of unpleasant, painful symptoms, you need to lead an active lifestyle and eat right. It is necessary to exclude spicy, fatty, salty foods, sweets, and alcohol. Eat more fruits, vegetables, greens. You should also follow the recommendations:
- maintain your weight in a normal range;
- wear comfortable (wide, without heels) shoes and loose, non-constrictive clothing;
- do not scratch the skin on the veins;
- regularly arrange contrasting douches and foot baths with herbs;
- walk every day for normal blood circulation;
- to be treated in sanatorium-resort institutions;
- use compression garments and elastic bandages to reduce pressure on the veins.
The only way to prevent such dangerous diseases and their relapses is to change your lifestyle - you need to get off the couch, engage in active physical exercise and sports, eat healthy, fortified foods, say “no” to all bad habits and breathe more fresh air.
Myth 14. In summer, treatment of varicose veins should be postponed until autumn.
For some reason, it is in Russia that there is an opinion that you should not undergo treatment in the summer. In hot countries, they are of the opinion that if a problem has appeared, there is no point in delaying its treatment.
Indeed, some people decide to have surgery during a more comfortable cool period. But here everyone makes a choice for themselves - to postpone solving a problem that is dangerous due to possible complications, or to get rid of the disease in a few days and enjoy the summer without varicose veins. In fact, modern phlebology does not depend on the seasons.
Useful tips - what to do
To stop pathological processes in the body, to get rid of unpleasant, painful symptoms, you need to lead an active lifestyle and eat right. It is necessary to exclude spicy, fatty, salty foods, sweets, and alcohol. Eat more fruits, vegetables, greens. You should also follow the recommendations:
- maintain your weight in a normal range;
- wear comfortable (wide, without heels) shoes and loose, non-constrictive clothing;
- do not scratch the skin on the veins;
- regularly arrange contrasting douches and foot baths with herbs;
- walk every day for normal blood circulation;
- to be treated in sanatorium-resort institutions;
- use compression garments and elastic bandages to reduce pressure on the veins.
The only way to prevent such dangerous diseases and their relapses is to change your lifestyle - you need to get off the couch, engage in active physical exercise and sports, eat healthy, fortified foods, say “no” to all bad habits and breathe more fresh air.
How to identify consequences after coronavirus
Not all patients need to go for a full examination of the body in order to identify what complications remain after Covid and whether they remain at all? Then clinics will have no time to treat patients. But some people after COVID-19 really need rehabilitation measures to eliminate the consequences. When should you seek help after you have had coronavirus?
First of all, this is poor health, a deterioration in the quality of life, and certain complaints that prevent a return to normal activities. Then you need to consult a therapist if the cause of your poor health is not clear, or go to a specialist in a narrow field with a specific complaint. The doctor must determine the direction of the study, identify the cause of the disease and take measures for rehabilitation.
What are the consequences of coronavirus for the lungs?
The most common symptom of coronavirus, as well as a complaint after illness, is shortness of breath. COVID-19 is not a simple respiratory infection. Coronavirus causes primary primary damage to the respiratory organs. That is, the main effect of the disease is on the lungs, but besides this, the infection affects almost all organs and systems to varying degrees.
The disease is more complex and longer, even compared to the severe form of influenza. If the flu is characterized by several days of high temperature, then several days of slightly elevated temperature, and then there is a period of convalescence and complete recovery, then coronavirus is treated within several weeks, and the course of the disease is often unpredictable. It may take months of therapy to restore the lungs after the disease.
The most common complication after COVID-19 is a pronounced change in the lungs, even if the virus is no longer in the body and the patient has recovered. This consequence of coronavirus is detected using tomography. In such cases, patients need supplemental oxygen, which they receive at rehabilitation centers or rent an oxygen concentrator and recover at home.
What happens when there is a complication on the lungs after Covid? Scars form on healthy tissue, which prevent the supply of the required amount of oxygen and contribute to the appearance of excess carbon dioxide. Depending on the degree of damage to the lungs, a person experiences difficulty breathing. Restoring the function of the respiratory system is a primary task, since fibrotic changes can cause the development of thrombosis and other pathologies.
If the affected area is large, the doctor selects a suitable drug treatment program, prescribes breathing exercises to stimulate lung function and accelerate tissue regeneration, supporting the functioning of organs with additional oxygen if necessary.