Potassium is the main intracellular macronutrient. About 90% of all potassium ions in the body are located inside cells. Such a large difference between intra- and extracellular concentrations is necessary to maintain the membrane potential of cells, their ability to excite and transmit nerve impulses. Accurate data on the overall prevalence of hypokalemia are not available. It is only known that it is detected in 3-20% of patients undergoing hospital treatment. This disorder is somewhat more often observed in patients of cardiology and gastroenterology departments.
Causes of hypokalemia
A relatively physiological and benign cause of hypokalemia can be considered excessive sweating during sports, a nutritional factor, i.e., insufficient intake of potassium from food (strict diets, monotonous diet). Pathological hypokalemia has a greater number of causes, differing in the mechanism that causes a decrease in potassium content in the body:
- Losses through the gastrointestinal tract.
Gastric and intestinal juice contain large amounts of potassium, so various diseases of the gastrointestinal tract (pancreatitis, ulcerative colitis), intestinal infections accompanied by repeated vomiting or prolonged diarrhea very often become the cause of this electrolyte imbalance. - Hyperaldosteronism.
Aldosterone stimulates the excretion of potassium ions by the kidneys. There is primary (adrenal tumor producing aldosterone) and secondary hyperaldosteronism (caused by chronic heart failure, renovascular hypertension, tumor secreting renin). - Kidney diseases.
The cause of hypokalemia can be kidney disease, characterized by tubular dysfunction, which results in disruption of the transport of hydrogen and potassium in the distal tubules and collecting ducts of the nephron, which leads to increased potassium excretion. Such diseases include interstitial nephritis and renal tubular acidosis. - Redistribution between the interstitium and the cell.
Some pathological conditions cause the transition of K+ from the extracellular space into the cells, which can cause a sharp drop in its concentration in the plasma. This occurs when the pH shifts to the alkaline side (alkalosis), after administering large doses of insulin to a patient with diabetic ketoacidosis, or with familial periodic paralysis. - Endocrine diseases.
In addition to aldosteroma, other diseases of the endocrine glands can also cause hypokalemia. These are thyrotoxicosis (thyrotoxic periodic paralysis), Itsenko-Cushing's syndrome/disease, congenital dysfunction of the adrenal cortex. - Taking medications.
The drugs most often associated with hypokalemia are diuretics (loop diuretics, thiazide diuretics). The use of beta-agonists, theophylline, and antibiotics (especially penicillins, aminoglycosides) can also lead to electrolyte disturbances. - Other reasons.
Hypomagnesemia, massive burns, Barter-Gittelman syndrome.
General information
Hypokalemia means a decrease in serum potassium content to below 3.5 mmol/l, the deficiency of which can be caused by both a decrease in its reserves in the body and pathological movement into cells.
Most of the potassium (120–160 mmol/L) is normally found in the intracellular space (about 90%), and the remainder is found in the blood/bone tissue. The normal level of potassium in the body is its serum concentration from 3.5 to 5.5 mmol/l. The concentration of potassium in the blood is relatively constant, which is regulated by the processes of its entry into cells/excretion by the kidneys. The process of moving potassium from the blood through cell membranes is determined by the concentration of potassium outside the cell, the state of the membranes and cellular metabolism. The binding of potassium inside the cell occurs during the formation of protein and glycogen: it has been established that for 1 g of glycogen, 1 g of protein nitrogen and 0.3 mmol of potassium ions enter the cells. Potassium enters the body with food in an average amount of 2-3 g/day and is absorbed in the gastrointestinal tract (small intestine); excreted in urine (2-5 g), to a lesser extent in feces (less than 10 mmol). The volume/rate of potassium excretion is determined by many factors: potassium concentration in the blood, osmolarity, acid-base balance, the influence of vasopressin / aldosterone , and the rate of cell turnover.
The daily potassium requirement of an adult varies between 40–100 mmol/l. Vitamin B6 increases the efficiency of potassium absorption , while alcohol negatively affects its balance in the body. It should be taken into account that potassium from food is poorly absorbed in case of magnesium deficiency. Therefore, the lack of potassium and magnesium in the body is often interrelated. Normally, potassium balance is constantly maintained by the process of its excretion and intake with food. At the same time, the potassium content in the body is inversely proportional to the sodium content, that is, the more potassium, the less sodium, and vice versa.
Potassium takes an active part in the transmission of nerve impulses, the formation of cellular potentials, the contraction of smooth/skeletal muscle fibers, and cardiomyocytes. The macroelement increases stress resistance/physical endurance, coordinates heart rate, is responsible for normalizing blood pressure, and helps eliminate allergens/toxins from the body. Lack of potassium in the body in women and lack of potassium in men is a dangerous condition, since its functions in the body are extremely wide: potassium maintains the bioelectrical activity of cells, acid-base balance/water-salt balance; Helps stabilize heart rate, blood pressure, and maintain pH levels.
There are no reliable statistics on the prevalence of hypokalemia in the general population. It is important to understand that both manifest and especially subclinical hypokalemia are very common in clinical practice, but often remain unrecognized. However, potassium deficiency is detected in 3-20% of patients in gastroenterology/cardiology departments. The reason for the difficulty in recognizing hypokalemia is the variability/dynamism and variety of its clinical manifestations, and therefore hypokalemia imitates various organ/systemic pathologies.
Pathogenesis
Hypokalemia leads to hyperpolarization of cell membranes, as a result of which the threshold for the occurrence of an action potential increases (up to its complete blocking), which impairs the excitability of neurons and myocytes. The transmission of nerve impulses in neuromuscular synapses and the conduction system of the heart is disrupted. The tone of skeletal muscles, smooth muscle walls of blood vessels, and internal organs decreases. This causes most of the symptoms.
Motility of the gastrointestinal tract slows down. The sensitivity of arterioles to the vasoconstrictor effect of angiotensin II decreases. Hypokalemia contributes to the appearance of ventricular ectopic rhythms in the heart and impairment of the concentrating ability of the kidneys (increased excretion of water). The secretion of insulin in the pancreas and aldosterone in the adrenal glands is suppressed.
Depletion of K+ reserves leads to the accumulation of hydrogen in the cell and intracellular acidosis. As a result, the processes of tissue respiration and glycolysis are suppressed. A pathological examination reveals dystrophic changes in almost all internal organs (especially the heart, kidneys, and liver).
Should I Take Potassium Supplements?
Potassium supplements are not recommended. Various well-known supplement manufacturers limit themselves to producing products containing up to 99 mg of potassium per capsule. They are recommended to take up to five capsules per day - up to 495 mg of potassium. By comparison, an average banana contains 422 mg of potassium.
This limit is likely low because studies have shown that high-dose potassium supplements can damage the intestines or cause abnormal heartbeats, which can lead to death.
Taking too much potassium can cause excess potassium to accumulate in the blood, causing a condition called hyperkalemia. Hyperkalemia can cause arrhythmia (irregular heartbeat), which can cause serious heart disease.
However, if your doctor has prescribed you to take this mineral in higher doses than indicated above, this is normal.
Conclusion:
It is not recommended to take potassium supplements as they are limited to only 99 mg of this mineral per capsule (no more than 5 capsules per day). In addition, studies have linked their use to adverse conditions.
Classification
Most often in clinical practice, hypokalemia is divided into:
- light
- K+ content 3-3.5 meq/l. - severe
- K+ level below 3 mmol/l.
Separately, pseudohypokalemia is distinguished, which has no symptoms and does not require treatment. A false test result can be obtained if the patient has a very high level of leukocytes (leukocytes actively absorb K+). This happens, for example, with leukemia or severe infection. Falsely elevated readings are also possible if the K+ concentration is determined in blood stored for a long time at room temperature.
List of sources
- Nascimento L. Hyperkalemia and hypokalemia // Difficult diagnosis: In 2 volumes / Ed. R.B. Taylor, vol. 1. M., Medicine, 1992, p. 302-322.
- Manual of clinical laboratory diagnostics. Part 3: Clinical biochemistry/Ed. prof. M.A. Bazarnova, prof. V.T. Morozova. K., Vishcha school, 1986, p. 216-223.
- Sokovets T.G., Bogdanov E.I. Hypokalemic myoplegia//Kazan Medical Journal. 2013. pp.933–938.
- Molashenko N.V., Platonova N.M., Yukina M.Yu. and others. Primary aldosteronism. Collection of methodological recommendations. Ed. E.A. Troshina. Tver: Triad; 2021.
- Heitz U. Water-electrolyte and acid-base balance. Per. from English M.: Binom; 2009.
Symptoms of hypokalemia
In some patients, hypokalemia may occur without any symptoms. The clinical picture and its severity are determined to a greater extent not by the K+ concentration, but by the rate of its decrease. Muscle weakness is one of the first symptoms. Sometimes muscle twitching (fasciculations) and tetanic convulsions (spasms) occur. Inhibition of the excitability of CNS neurons leads to the development of symptoms of psychasthenia (drowsiness, apathy, poor concentration).
Due to the slow motility of the gastrointestinal tract during meals, a feeling of satiety sets in very quickly, and heaviness in the epigastrium is disturbing. Constipation is typical. The conduction system of the heart is especially sensitive to a decrease in K+ - tachycardia and interruptions in heart function appear. Due to hypotension, dizziness begins. With primary hyperaldosteronism, on the contrary, symptoms of arterial hypertension are always observed (heaviness and pain in the back of the head, tinnitus). Patients are also concerned about increased diuresis and a constant feeling of thirst.
Treatment of potassium deficiency with drugs
Taking medications with potassium in the form of tablets and dragees helps to quickly replenish potassium reserves in the body. The most commonly prescribed drugs are:
- panangin;
- potassium orotate;
- potassium-normine;
- asparkam.
The dosage depends on the degree of development of hypokalemia and the individual characteristics of the body. Tablets and pills are taken during or after meals; they must be swallowed whole, without chewing.
In especially severe cases, potassium chloride can be used in the form of intravenous injections.
But in general, this method is not recommended: such therapy can cause rebound hypokalemia - a phenomenon when glucose in the drug not only does not restore the required potassium concentration, but also causes it to fall even further.
Complications
The most serious complication of this electrolyte disorder is considered to be cardiac arrhythmia - ventricular tachycardia, ventricular fibrillation, which without immediate treatment very often leads to death. Hypokalemia also increases sensitivity to cardiac glycosides, which increases the risk of glycoside (digitalis) intoxication.
Some patients develop respiratory failure due to severe weakness of the diaphragm and intercostal muscles. Dynamic intestinal obstruction is possible. A very rare complication of severe hypokalemia is rhabdomyolysis (destruction of muscle tissue). Long-term depletion of potassium ions can lead to the formation of cysts in the kidneys and chronic renal failure.
Muscle cramps and spasms
Potassium deficiency can manifest itself in the form of muscle cramps and spasms. Muscle cramps are sudden, uncontrollable muscle contractions. They can occur when the level of this mineral in the blood becomes too low. Inside muscle cells, potassium helps relay signals from the brain that stimulate contractions. It also helps stop these contractions by leaving the muscle cells.
When blood potassium levels are low, your brain cannot transmit these signals effectively. This leads to longer contractions, such as muscle cramps.
Conclusion:
Potassium helps start and stop muscle contractions. Low levels of potassium in the blood can affect this balance, causing uncontrollable and prolonged muscle contractions known as cramps.
Diagnostics
Patients with this electrolyte disorder are treated by doctors of different specialties, depending on what caused its development. Most often these are gastroenterologists, nephrologists, and endocrinologists. It is found out what medications the patient is taking. During examination, the most important thing is to identify symptoms such as muscle hypotension and arrhythmic pulse. An additional examination is prescribed, which includes:
- Laboratory research.
Blood CBS, magnesium, sodium, calcium content are determined. A biochemical blood test examines the concentration of creatinine, urea, and creatine phosphokinase. A urine test checks its relative density and the presence of chlorine. To differentiate between renal and extrarenal causes of hypokalemia, the transtubular potassium gradient (the ratio of serum to urine osmolarity between urine and plasma K+ levels) is calculated. - Hormonal spectrum.
To exclude aldosteroma, the levels of aldosterone and renin are measured to calculate the renin-aldosterone ratio. If there are corresponding symptoms of endocrine pathology, tests are performed for thyroid-stimulating hormone, cortisol, and 17-OH-progesterone. - Electrocardiography.
ECG is the main instrumental research method for diagnosing hypokalemia. The following changes are noted: depression of the ST segment, appearance of a U wave, prolongation of the QT interval. With severe electrolyte imbalance, paroxysmal ventricular tachycardia occurs, sometimes developing into atrial fibrillation. - Instrumental research.
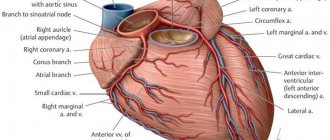
To visualize aldosteroma, ultrasound and CT scan of the adrenal glands are performed. In case of kidney diseases, an ultrasound of the kidneys with Doppler sonography is performed. If chronic heart failure is suspected, echocardiography is prescribed. To confirm renovascular hypertension, selective angiography of the renal arteries is informative.
The differential diagnosis should be primarily with hyperkalemia, since these conditions have similar clinical symptoms. Hypokalemia should also be distinguished from neuromuscular diseases (myasthenia gravis, Guillain-Barre syndrome, muscular dystrophies), diseases occurring with insipidal syndrome (diabetes mellitus, diabetes insipidus). Acute paralysis requires the exclusion of stroke.
Balance of potassium and magnesium
Magnesium is essential for heart and blood vessel health. But it is not able to perform its functions without potassium. In tandem, these nutrients restore metabolism in the myocardium and improve heart function. By consuming foods with potassium and magnesium, a person prevents the occurrence of dangerous pathologies. If you increase the proportion of food containing these nutrients in your diet, the likelihood of developing atherosclerosis and heart pathologies will decrease. Doctors recommend that patients who have had a heart attack or stroke:
- eat foods high in potassium;
- Use foods from the list that can quickly increase your nutrient levels.
Nutritionists emphasize that if you eat an increased amount of fresh vegetables and fruits, greens, this improves brain function. Thanks to them, memory increases and concentration increases. The functions of potassium are related to the activities of sodium in the body. These nutrients work in concert.
For effective interaction between minerals, you need to consume foods that contain potassium and sodium in optimal proportions of 3:1.
If a person eats foods rich in sodium, he should not add foods rich in potassium to his diet. This will maintain a balance between nutrients and prevent the development of diseases caused by an overabundance of one and a lack of another substance. High concentrations of potassium and sodium are found in seaweed, beans, potatoes, raisins, and seafood. When a person consumes tomato juice with added salt, the value of the product decreases. Although the drink contains a lot of potassium, if there is an excess of salt, the body uses it irrationally.
Treatment of hypokalemia
The department in which patients are treated is determined by the pathology that caused the decrease in K+ (nephrology, gastroenterology, etc.). Patients in serious condition must be transferred to the intensive care unit. To begin with, all medications that can lead to hypokalemia are discontinued. The main and primary task is to normalize K+ concentration and stop life-threatening rhythm disturbances.
- Correction of potassium deficiency.
In case of mild and stable condition of the patient, oral forms of potassium preparation (KCl) are prescribed as treatment. For severe hypokalemia, intravenous administration is preferable. When combined with metabolic acidosis, hydrocarbonate and citrate salts are used. To avoid hyperkalemia, the infusion rate should not exceed 10 mEq/hour. In order to reduce the renal excretion of potassium ions, potassium-sparing diuretics (spironolactone) are added to treatment. - Fighting arrhythmias.
In the vast majority of cases, replenishment of the K+ deficiency is sufficient to achieve sinus rhythm. In some situations it is necessary to use antiarrhythmic drugs (amiodarone, propafenone, flecainide). When ventricular fibrillation develops, the only treatment option is defibrillation.
Causes of potassium deficiency
Macronutrient deficiency under the influence of specific circumstances can be triggered by one or more of the following reasons:
- A woman's diet does not contain enough foods containing a lot of potassium. As soon as the body detects such a deficiency, it will begin to manage the potassium contained in the blood more rationally: it will reduce the process of excreting the macroelement through urine and sweat. However, a moment soon comes when there is nothing left to make up for the shortage;
- Diuretics and laxatives have been taken; there is a significant amount of salt and sodium-containing preservatives in the diet;
- A woman is in a state of high need for potassium - this usually occurs during pregnancy, during the lactation period, and also after surgery;
- Have thyroid disease;
- Excessive excretion of the component during urination or hormonal abnormalities caused by the treatment of this pathology;
- Excessive exercise, accompanied by increased sweating. In such cases, a significant part of K+ is washed out along with sweat.
The most common causes of potassium deficiency among women: passion for diets in order to correct their own weight.
Prognosis and prevention
Hypokalemia is a serious pathology that can be fatal without timely treatment. The most common cause of death is arrhythmias (PVT, VF). Less commonly, patients die from diaphragmatic paralysis or acute renal failure due to massive rhabdomyolysis. Prevention comes down to treating diseases that cause a decrease in the level of K+ in the blood, adding potassium-berger diuretics to regular diuretics, and consuming foods rich in potassium (bananas, dried fruits, vegetables).
Diet
There is no special diet, but adjusting the diet to include foods rich in potassium is a critical component of correcting hypokalemia. For this purpose, it is recommended to include in the diet dairy products (milk, cottage cheese and sour cream), legumes, oatmeal/buckwheat, mushrooms, potatoes, bread with bran, tomato, sea fish (mackerel, pollock, salmon, tuna, sprat), cabbage (cauliflower/white cabbage/broccoli), carrots, cucumbers, greens (parsley, spinach), seaweed, fresh fruits (peaches, bananas, kiwi, avocados, apricots), nuts, dried fruits (prunes, dried apricots, raisins), compotes, black tea, cocoa, tomato juice, freshly squeezed juices (grape, orange, carrot), chocolate.
Unnatural sugar-containing drinks (lemonade, Coca-Cola, Fanta, Pepsi) should be limited/completely excluded from the diet. The consumption of salt is also subject to restrictions, but at the same time, a salt-free diet is not allowed. It is important to consider that most of the potassium dissolves in water during heat treatment, so you need to boil foods in a minimum amount of water.
How to compensate for potassium deficiency
Pharmaceuticals offers a variety of pharmaceutical drugs, for example: Asparkam, Potassium Orotate, Panangin, Normin at an affordable price to replenish the reserves of an important macronutrient. Replenishing the body means normalizing nutrition, which is important for women during pregnancy with hypokalemia.
The macronutrient is found in large quantities in the following products:
- porridge (oatmeal, buckwheat, barley),
- bananas,
- dried fruits,
- nuts,
- pumpkin,
- melons,
- watermelons,
- mushrooms,
- meat,
- freshly squeezed carrot juice,
- apples,
- celery,
- sprouted wheat grains.
Patients with hypokalemia should avoid consuming strong coffee, sweets, and alcohol. It is recommended to steam dishes made from foods high in potassium in the oven for the purpose. However, during treatment and prevention, one should not overdo it and forget that an excess of potassium is just as harmful as its lack. May cause increased stress on the kidneys.
If patients have to take long-term courses of laxatives and diuretics, then it may be worth discussing with their doctor the selection of a replacement for potassium-sparing diuretics. It is important for athletes to consume foods containing natural minerals every day.
Electrolyte imbalance and its role in the development of cardiovascular diseases
The article discusses the role of magnesium and potassium deficiency in the development of cardiovascular diseases and their complications. Risk factors for the development and symptoms of potassium and magnesium deficiency are described. The results of studies on the effectiveness of magnesium and potassium preparations used in cardiological practice are presented. The importance of potassium and magnesium preparations in preventing the progression of atherosclerosis, arterial hypertension, endothelial dysfunction, and disorders of carbohydrate and lipid metabolism has been shown. The advantages of magnesium and potassium aspartate preparations in order to eliminate the deficiency of these cations have been demonstrated.
Table 1. Foods high in magnesium and potassium
Table 2. Symptoms of potassium and magnesium deficiency
SHEP study: relative risk of cardiovascular events during treatment with chlorthalidone depending on plasma potassium levels (relative risk of cardiovascular events in the placebo group is set to 1)
Table 3. Positive effect on the prognosis of additional daily magnesium intake in patients at high cardiovascular risk in the PREDIMED study
Introduction
In recent years, a special role in the development and progression of cardiovascular diseases (CVD) has been assigned to electrolyte imbalances, in particular the balance of magnesium and potassium [1, 2]. Potassium is the main intracellular cation. Normally, the cell contains 150–160 mmol/l of potassium, and the blood plasma contains 3.5–5.5 mmol/l. Potassium is involved in the bioelectrical activity of cells, the formation of cellular action potentials and the maintenance of neuromuscular excitability and conductivity. The second most important intracellular cation is magnesium. Magnesium is a universal regulator of biochemical and physiological processes in the body, a cofactor for over 300 enzymes involved in biochemical reactions. Magnesium ensures the hydrolysis of adenosine triphosphate (ATP), reduces the separation of oxidation and phosphorylation, regulates the polarization of cell membranes, controls the spontaneous electrical activity of nervous tissue and the conduction system of the heart, the normal functioning of the cardiomyocyte, and is involved in the metabolism of carbohydrates, lipids, nucleic acids and proteins. Magnesium is a natural physiological calcium antagonist. It reduces the release of calcium from the sarcoplasmic reticulum and protects cells from calcium overload under ischemic conditions, reduces platelet aggregation ability, and maintains normal transmembrane potential in electrically excitable tissues [3, 4]. Mg2+ deficiency is associated with increased levels of total cholesterol, low-density lipoproteins, triglycerides, decreased activity of lecithin-cholesterol aminotransferase and lipoprotein lipase, and increased activity of HMG-CoA reductase. Magnesium has an antiatherogenic effect [5, 6]. Data have emerged on the decisive role of magnesium in the synthesis and metabolism of vitamin D, the deficiency of which is considered an independent risk factor for the development of CVD [7].
Potassium enters the body with food, magnesium - with food and water, excess potassium and magnesium is excreted in the urine. The daily requirement for potassium is 2500 mg. The magnesium requirement of an adult is 300–400 mg/day (increases during the period of growth, as well as in persons engaged in physical labor, athletes, and pregnant women). Potassium is found in bananas, potatoes, dried fruits, apricots, spinach, broccoli, and legumes. Dried apricots, prunes, nuts, dark chocolate, and seaweed are characterized by a high content of potassium and magnesium (Table 1). However, digestibility from food products does not exceed 30–35%.
Hypokalemia is a persistent decrease in serum potassium concentration less than 3.5 mmol/l, hypomagnesemia is a decrease in serum magnesium concentration less than 0.8 mmol/l. The normal intracellular potassium content is 150–160 mmol/l, magnesium – 1.65–2.55 mmol/l. It should be taken into account that with normal levels of potassium and magnesium in the blood serum, an intracellular deficiency of these cations may occur.
In many regions, the concentration of magnesium in drinking water and soil, as well as in plant foods grown in these regions, is low. Daily magnesium intake is significantly lower than recommended.
In industrialized countries, the number of people with magnesium deficiency is increasing [7, 8]. In the United States, almost 75% of the population has a magnesium deficiency or its level corresponds to the lower limit of normal [9].
Causes of potassium and magnesium deficiency
The most common causes of potassium and magnesium deficiency include:
- insufficient intake of potassium and magnesium into the body from food (with poor nutrition, deficiency in the diet of foods containing potassium and magnesium) or malabsorption (malabsorption syndrome, chronic gastroduodenitis, condition after intestinal resection);
- loss of potassium and magnesium due to vomiting and chronic diarrhea (intestinal secretions contain a large amount of potassium), sauna abuse, alcohol abuse, endocrine pathology (diabetes mellitus, hyperthyroidism, hyperparathyroidism, hyperaldosteronism);
- increased excretion of potassium and magnesium due to improper use of diuretics, primary and secondary hyperaldosteronism, renal tubular defects (Barter syndrome, Gitelman syndrome).
Manifestations of potassium and magnesium deficiency
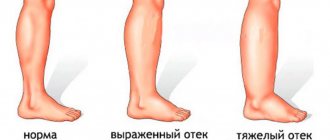
The variety of manifestations of potassium and magnesium deficiency is due to the numerous functions of these cations in the body (Table 2). One of the most common manifestations of potassium deficiency is a disorder of neuromuscular transmission (muscle weakness, leg muscle spasms, paresthesia, extinction of tendon reflexes) [10]. Hypokalemia is also manifested by disorders of the cardiovascular system (decreased myocardial contractile function, dilatation of the heart cavities, decreased blood pressure) [11]. Damage to smooth muscles leads to intestinal paresis, vomiting, flatulence, constipation, and bladder atony [12].
Chronic hypokalemia can manifest itself as dysfunction of the central and peripheral nervous system (mild paresthesia of the face and extremities, decreased pain and tactile sensitivity, muscle weakness, tremor, hyperhidrosis).
Hypomagnesemia is characterized by increased fatigue, irritability, chronic fatigue, depression, apathy, dizziness, decreased memory and the ability to concentrate and maintain attention. The initial signs of magnesium deficiency include hair loss, brittle nails, caries, weather sensitivity, sleep disturbances (insomnia, nightmares, difficulty waking up even after a normal amount of sleep).
Both hypokalemia and hypomagnesemia are characterized by fluctuations in blood pressure (BP), the appearance of heart rhythm disturbances, and certain changes in the electrocardiogram (widening of the QRS complex, decreased ST segment, depression or inversion of the T wave, pronounced U wave) [13, 14].
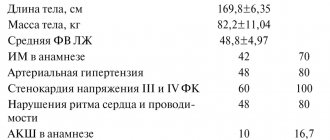
Studies on the effectiveness of potassium and magnesium preparations
The SHEP study established an inverse statistically significant relationship between the level of potassium in the blood plasma and the incidence of cardiovascular complications: when the potassium level decreased to less than 3.5 mmol/l during chlorthalidone therapy, the risk of myocardial infarction, stroke, and cardiovascular events increased (Figure) [15]. In other words, when the potassium level decreases to less than 3.5 mmol/l during long-term therapy with thiazide diuretics, their positive effect on the prognosis is neutralized. It should be noted that in the first year of chlorthalidone therapy, hypokalemia was detected in 7.2% of patients.
Numerous data indicate that increasing the intake of both potassium and magnesium is accompanied by a decrease in the incidence of cardiovascular complications, improvement in the course of heart failure, and a decrease in the severity of left ventricular hypertrophy, arrhythmias, and new cases of diabetes mellitus.
A meta-analysis of a number of prospective studies showed that supplementation with 42 mmol potassium per day significantly reduced the relative risk of stroke (by 21%; p = 0.0007) with a trend towards a lower risk of coronary events (by 7%; p = 0.03) and CVD in general (by 26%; p = 0.0037) [16].
The randomized clinical trial PREDIMED [17] included 7216 patients with high and very high cardiovascular risk (mean age 67 years). At the time of inclusion in the study, patients did not have a diagnosed CVD, but were at high risk of developing it (type 2 diabetes mellitus, family history of CVD, overweight or obesity, smoking, arterial hypertension, hypercholesterolemia, low high-density lipoprotein cholesterol) . All patients were on a Mediterranean diet. Study participants were divided into three groups—three tertiles—depending on the amount of magnesium consumed daily (patients with the highest magnesium intake (tertile 3) also had higher plasma magnesium concentrations). The study lasted about five years. An inverse relationship was found between magnesium intake and the incidence of cardiovascular events, cardiovascular mortality, cancer mortality and total mortality (Table 3). According to the researchers, the distinct hypotensive, hypolipidemic and antiplatelet effects of magnesium, its ability to improve endothelial function and modulate inflammation, and reduce insulin resistance could have a positive effect on outcomes.
According to a meta-analysis of 19 studies, when using potassium supplements, blood pressure decreased by an average of 5.9/3.4 mm Hg. Art. [18]. The Canadian Guidelines for the Diagnosis, Risk Assessment, Prevention and Treatment of Hypertension (2021 Revision) emphasize the need to increase potassium intake to lower BP (in patients not at high risk for hyperkalemia) [19]. The hypotensive effect of potassium is provided by:
- increased natriuresis;
- changes in baroreceptor sensitivity;
- decreased sensitivity to catecholamines and angiotensin II;
- increase in Na+-K+-ATPase in vascular smooth muscle cells;
- improving the function of the sympathetic nervous system;
- increased sensitivity to insulin;
- decrease in intracellular Na+ and decrease in the formation of transforming growth factor beta [20].
Magnesium, being a natural physiological calcium antagonist, reduces systemic and pulmonary vascular resistance with a subsequent decrease in systemic blood pressure and a slight increase in cardiac index [4]. Reliable data have also been obtained (meta-analysis of 22 clinical studies) on the clinically significant antihypertensive effect of magnesium preparations.
Magnesium has been shown to suppress platelet activation by inhibiting thromboxane A2 or potentiating the synthesis of antiplatelet factors such as prostacyclin (prostaglandin I2). An increase in serum magnesium levels may interfere with the binding of fibrinogen to glycoprotein IIb–IIIa receptors by changing the structure of the receptors [8]. Intravenous administration of magnesium sulfate to healthy volunteers suppressed adenosine diphosphate-induced platelet aggregation by 40% [21].
A double-blind, placebo-controlled clinical study in patients with coronary heart disease (CHD) revealed a significant improvement in endothelial function and increased exercise tolerance with the use of magnesium supplements at a dose of 30 mmol/day [22]. According to a meta-analysis of 16 prospective studies (included over 310,000 patients), plasma magnesium levels are inversely proportional to the risk of developing cardiac arrhythmias and complications of coronary artery disease, including fatal myocardial infarction [23].
Magnesium deficiency is associated with impaired glucose tolerance [24]. With magnesium deficiency, insulin resistance can develop, which interferes with both the uptake of glucose into the cell and the transport of magnesium into the cell. It has been shown that the administration of magnesium as a dietary supplement to persons with arterial hypertension and/or type 2 diabetes mellitus helps reduce insulin resistance, the severity of dyslipidemia, and lower blood pressure levels [25–27]. Hypomagnesemia increases with decompensation of diabetes mellitus (additional losses of magnesium during polyuria).
Treatment and prevention of hypokalemia and hypomagnesemia
Even severe hypokalemia and hypomagnesemia often remain unrecognized in clinical practice. A doctor of any specialty must remember the clinical manifestations of potassium and magnesium deficiency in the body in order to promptly eliminate or prevent their development in risk groups with the help of adequate therapy. It must also be remembered that magnesium promotes the fixation of potassium in the cell. Without eliminating magnesium deficiency, it is impossible to solve the problem of intracellular potassium deficiency.
In many characteristics, potassium and magnesium complement each other and represent a kind of metabolic tandem [28]. The fairly high frequency and severity of combined deficiency of these macroelements justifies the advisability of using combined K+ and Mg2+ preparations for a number of conditions associated with a high risk of developing hypokalemia and hypomagnesemia.
Taking into account the role of potassium and magnesium ions in the development of pathology in the body, the need to correct the deficiency of these cations is obvious. Methods for correcting potassium and magnesium deficiency include dietary measures and pharmacotherapy. Typically, the intake of the required amount of potassium and magnesium into the body is ensured by a balanced diet. If there are clear clinical or subclinical signs of potassium and magnesium deficiency, replacement therapy is carried out, and subsequently in risk groups - preventive therapy. As already noted, a combination of potassium and magnesium ions in one preparation is preferable, since due to the common risk factors for development, potassium deficiency is often accompanied by magnesium deficiency, which requires simultaneous correction of the level of both ions [29–30]. The role of magnesium in maintaining intracellular potassium concentrations is especially important in cardiomyocytes, since magnesium reduces their sensitivity to the arrhythmogenic effects of cardiac glycosides [31].
The results of the randomized, multicenter, placebo-controlled, double-blind study MAGICA allowed us to consider magnesium and potassium preparations as the generally accepted European standard for the treatment of patients with arrhythmia while taking cardiac glycosides, diuretics, and antiarrhythmic drugs [32].
As an antiarrhythmic agent, magnesium salts are often used for ventricular tachycardia of the torsades de pointes type due to their ability to inhibit the development of trace depolarizations and thereby reduce the duration of the QT interval [33].
National guidelines for determining the risk and prevention of sudden cardiac death [34] consider electrolyte disturbances as a possible cause of sudden death in patients with a structurally normal heart. It is recommended to use potassium and magnesium salts for the treatment and prevention of ventricular arrhythmias when using thiazide diuretics, intoxication with cardiac glycosides, acute and chronic alcohol and drug intoxication, and anorexia. Moreover, in patients with verified life-threatening ventricular arrhythmias, it is advisable to maintain the serum potassium level in the range of 4.5–5.5 mmol/l, although a potassium level from 3.5 to 5.5 mmol/l is considered normal.
High clinical effectiveness is observed when potassium and magnesium are combined with aspartic acid. It has been established that aspartic acid, when included in the Krebs cycle, actively participates in the synthesis of ATP, promotes the entry of K+ and Mg2+ ions into the cell, restores the adequate functioning of ion pumps under hypoxic conditions, normalizes the processes of excitation and inhibition in nerve cells, and stimulates the immune system. In addition, aspartic acid promotes the conversion of carbohydrates into glucose and supplies myocytes with an energy substrate for oxidative phosphorylation [35]. Salts of aspartic acid have an adaptogenic effect, increasing the body's endurance and resistance to various stress factors.
Since 1960, K-Mg aspartate has been actively used in clinical practice. One of the most well-known preparations of K-Mg-aspartate is the drug Panangin, containing potassium and magnesium in an easily digestible form, produced in film-coated tablets containing 158 mg of potassium aspartate (36.2 mg of potassium) and 140 mg of magnesium aspartate ( 11.8 mg magnesium), as well as in the form of an injection solution in 10 ml ampoules containing 452 mg of potassium aspartate (103.3 mg of potassium) and 0.40 mg of magnesium aspartate (33.7 mg of magnesium). Recently, the drug Panangin Forte appeared on the pharmaceutical market, containing 316 mg of potassium aspartate (72.4 mg of potassium) and 280 mg of magnesium aspartate (23.6 mg of magnesium).
Panangin is the drug of choice for the complex treatment and prevention of hypokalemia and hypomagnesemia. The presence of a cardioprotective effect, a positive effect on liver function and blood pressure levels, and a reduced risk of arrhythmias significantly expand the range of clinical applications of Panangin [30, 36].
To eliminate severe deficiency of potassium and magnesium, Panangin Forte is prescribed (one tablet three times a day), to prevent the development of hypokalemia and hypomagnesemia - Panangin (one tablet three times a day after meals). The duration of treatment is determined individually and is usually three to four weeks, due to the gradual saturation of tissue depots.
The drug is indicated as an adjuvant therapy in patients with chronic heart disease (heart failure, post-myocardial infarction), cardiac arrhythmia (primarily ventricular arrhythmia), and during therapy with cardiac glycosides. The usual daily dose for adults is one or two tablets three times a day.
The use of the drug Panangin is pathogenetically justified for a number of conditions and diseases associated with the risk of developing hypokalemia and hypomagnesemia. The experience of clinical use of the drug Panangin confirms its high effectiveness in the correction and prevention of potassium-magnesium deficiency.
According to a number of randomized controlled trials [37–39], the addition of Panangin to standard therapy for coronary artery disease and chronic heart failure can reduce the number of angina attacks by 20% (p
The clinical effectiveness of the drug Panangin is due to the following pharmacological properties: improvement of vascular endothelial function and anti-atherosclerotic effect, antihypertensive effect and reduction of blood viscosity and thrombus formation [40].
Sometimes doctors are afraid to prescribe potassium and magnesium supplements because of the possible development of hyperkalemia and hypermagnesemia, but the risk of developing these conditions increases mainly in chronic kidney disease, in the case of severe (
A meta-analysis of 20 randomized clinical trials demonstrated the effect of oral potassium supplementation on serum potassium concentrations. Consumption of potassium supplements in doses up to 5460 mg/day for six months leads to a small but significant increase in circulating potassium concentration by 0.14 mmol/l, but does not contribute to the development of hyperkalemia or deterioration of renal function. Thus, the use of potassium supplements is safe for patients receiving blockers of the renin-angiotensin-aldosterone system (RAAS) [41]. Since RAAS inhibition is currently a key strategy in the treatment of hypertension and cardiovascular disease [42], the simultaneous administration of potassium and magnesium supplements and RAAS blockers is being considered in some situations. According to a meta-analysis of 39 studies, when RAAS blockers were prescribed to patients without chronic kidney disease, the incidence of hyperkalemia did not exceed 2% [43].
Panangin can be called the drug of first choice for relieving identified potassium deficiency (decreased K+ concentration in serum
Conclusion
An important component of modern clinical practice should be monitoring of electrolyte, primarily potassium-magnesium balance. If there is a high risk of developing hypokalemia and hypomagnesemia, both correction (if detected) and prevention of the development of potassium and magnesium deficiency should be carried out. Maintaining the potassium-magnesium balance provides an additional therapeutic effect in patients with arterial hypertension, diabetes mellitus, congestive heart failure, as well as in patients with a high risk of developing cerebral stroke and heart rhythm disturbances. The optimal option in the pharmacological correction and prevention of hypokalemia and hypomagnesemia is the use of K-Mg aspartate (Panangin and Panangina Forte), many years of clinical experience of which have confirmed its high therapeutic efficacy and safety.