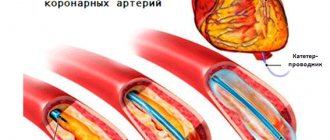
The rapid development of cardiovascular surgery, interventional cardiology, the development and implementation of new protocols for providing medical care to patients suffering from coronary heart disease (CHD), as well as the expansion of indications for myocardial revascularization have led to a change in the profile of patients undergoing coronary artery bypass grafting. The proportion of older patients with diffuse coronary artery disease and severe concomitant diseases is growing; many of them have already undergone percutaneous coronary intervention (PCI) [1, 5, 8].
Patients with this type of coronary lesion are one of the most severe groups of patients with coronary artery disease, in whom, even with the maximum possible multicomponent conservative therapy, as a rule, the prognosis remains unfavorable [2, 3]. Despite the high modern level of cardiac surgical care, the diffuse form of coronary artery disease poses great difficulties for surgical revascularization of the myocardium. The combined performance of coronary artery bypass grafting with various options of endarterectomy or bypass grafting (SHP) can help solve these problems [2, 4, 6, 7].
To date, there are no clear criteria for determining indications and contraindications for myocardial revascularization in combination with coronary endarterectomy (CE) or S.P. The principles on the basis of which the optimal volume of myocardial revascularization should be determined for diffuse damage to the coronary arteries have not been developed.
Translation into English of the names and abbreviations of the arteries of the heart
Serzhenko Nadezhda Medical translation agency "Medtran"
Translation of coronary angiography results raises many questions even for an experienced medical translator. The topic is quite difficult for a number of reasons:
- Complex anatomy of the coronary arteries
- A huge variety of anatomical options
- Abundance of terms and abbreviations
- Lack of a unified nomenclature
- Almost every artery has several synonymous names in both Russian and English
A standard situation for a medical translator is that it is necessary to translate an extract from the patient’s medical history, which contains a description of the results of coronary angiography, or, among other medical documents, there is a protocol for angiography of the coronary arteries. If the translator does not have experience in such translations, then two paragraphs of such text may take several hours.
Many translation problems arise due to synonyms (different variants of the names of the same artery). In order to correctly translate the variant name of an artery encountered in a medical history (which does not always have an unambiguous analogue in English), it is often necessary to search and compare the description of the anatomical structure in Russian with the description in English to make sure that the selected English term corresponds to the Russian name for the artery.
To avoid distortion of meaning when translating the names of anatomical formations and angiographic terms into English, we strongly recommend using analogues that are as close as possible to the Russian original. Despite the fact that the same artery may have several names in both Russian and English, the use of synonyms should be kept to a minimum, because this makes verification difficult and is a potential source of error. The translation of a medical text must convey the content of the source text as closely as possible, and the translator does not have the right to interpret the available information at his own discretion. However, for correct translation it is necessary to understand the basics of angiography and know the anatomy of the coronary arteries.
The terms and explanations below are intended to facilitate the work of the translator and help avoid errors when translating angiocoronary angiograms.
Chambers of the heart
The heart is a hollow (that is, empty from the inside) organ. It is a bag of dense muscle tissue, which has four cavities:
- Right atrium (atrium dexter);
- Right ventricle (ventriculus dexter);
- Left atrium (atrium sinister);
- Left ventricle (ventriculus sinister).
These cavities are also called the chambers of the heart. The human heart has four cavities, that is, four chambers. That is why they say that a person has a four-chambered heart .
On a heart that is cut in the frontal plane, I highlighted the boundaries of the right atrium in yellow, the left preseries in green, the right ventricle in blue, and the left ventricle in black.
Right atrium
The right atrium collects “ dirty ” (that is, rich in carbon dioxide and poor in oxygen) blood from throughout the body. The upper (brown) and lower (yellow) complete veins flow into the right atrium, which collect blood with carbon dioxide from the entire body, as well as the great vein of the heart (green), which collects blood with carbon dioxide from the heart itself. Accordingly, three openings open into the right atrium.
Between the right and left atria there is an interventricular septum. It contains an oval depression - a small oval-shaped depression, an oval fossa (fossa ovalis). In the embryonic period, in place of this depression there was an oval hole (foramen ovale cordis). Normally, the foramen ovale begins to close immediately after birth. In this picture, the oval fossa is highlighted in blue:
The right atrium communicates with the right ventricle through the right atrioventricular orifice (ostium atrioventriculare dextrum). The flow of blood through this opening is controlled by the tricuspid valve.
Right ventricle
This cavity of the heart receives “dirty” blood from the left atrium and sends it to the lungs to be cleaned of carbon dioxide and enriched with oxygen. Accordingly, the right ventricle connects to the pulmonary trunk, through which blood will be sent to the lungs.
The tricuspid valve, which must be closed during the reflux of blood into the pulmonary trunk, is fixed by tendon threads to the papillary muscles. It is the contraction and relaxation of these muscles that controls the operation of the tricuspid valve.
The papillary muscles are highlighted in green, and the tendon filaments are highlighted in yellow:
Left atrium
This part of the heart collects the “ purest ” blood. It is into the left atrium that fresh blood flows, which is first purified in the small (pulmonary) circle from carbon dioxide and saturated with oxygen.
Therefore, four pulmonary veins flow into the left atrium - two from each lung. You can see these holes in the picture - I've highlighted them in green. We remember that arterial passes veins .
The left atrium communicates with the left ventricle through the left atrioventricular orifice (ostium atrioventriculare sinistrum). The flow of blood through this opening is regulated by the mitral valve.
Left ventricle
The left ventricle begins the systemic circulation . When the left ventricle pumps blood into the aorta, it is isolated from the left atrium by the mitral valve. Just like the tricuspid valve, the mitral valve is controlled by papillary muscles (highlighted in green), which are connected to it by tendon strands.
You may notice the very strong muscular wall of the left ventricle. This is explained by the fact that the left ventricle needs to pump a powerful flow of blood, which must be sent not only in the direction of gravity (to the stomach and legs), but also against gravity - that is, upward , to the neck and head.
Can you imagine how cunningly the circulatory system of giraffes is designed, in which the heart must pump blood all the way up the neck to the head?
The aortic sinuses
The aortic sinuses, or sinuses of Valsalva, are the pockets between the semilunar valves of the aorta and its wall. The names of the sinuses correspond to the names of the coronary arteries branching from them: the right coronary artery departs from the right coronary sinus, the left coronary artery departs from the left coronary sinus, and the posterior sinus of Valsalva is called non-coronary (non-coronary sinus), since the coronary arteries do not depart from it. The aortic sinuses facing the pulmonary artery are called “facing aortic sinuses”.
The aortic valve has three leaflets, each having a cusp or cup-like configuration. These are known as the left coronary cusp, the right coronary cusp and the posterior non-coronary cusp. Just above the aortic valves there are anatomic dilations of the ascending aorta, also known as the sinus of Valsalva. The left aortic sinus gives rise to the left coronary artery. The right aortic sinus which lies anteriorly, gives rise to the right coronary artery. The non-coronary sinus is positioned on the right side.
The aortic sinuses that are adjacent to the pulmonary valve (facing the pulmonary valve) are described as the 'facing' aortic sinuses.
Right aortic sinus (1st facial sinus, right sinus of Valsalva). Right coronary sinus, right anterior sinus, right sinus of Valsalva, right-facing sinus (anat.: anterior aortic sinus).
The right coronary artery arises from the right aortic sinus.
Left aortic sinus (2nd facial sinus, left sinus of Valsalva). Left coronary sinus, left anterior sinus, left sinus of Valsalva, left-facing sinus (anat.: left posterior aortic sinus).
The left aortic sinus is the origin of the left coronary artery.
Non-coronary aortic sinus (non-facial aortic sinus, posterior sinus of Valsalva). Non-coronary aortic sinus, posterior sinus of Valsalva, non-facing aortic sinus (anat.: right posterior aortic sinus, sinus aortae posterior dexter).
Non-facing aortic sinus is that aortic sinus that does not face the pulmonary artery. The first one from it, when oriented counterclockwise, is called the “1st facial sinus”, and the next one is the “2nd facial sinus” (Terminology developed by a group of researchers from Leiden University (A. Gittenberger: de Groot et al., 1983)).
Non-coronary aortic sinus is an aortic sinus from which the coronary arteries do not arise. Typically (in most people), the posterior (non-facial) aortic sinus is also non-coronary. However, there are many variations in the anatomical structure of the coronary arteries, both normal and pathological, so it is important to understand the difference between the terms “facial” and “coronary” (see comments on the figure).
A diagram explaining the definition of terms.
a: the nonfacial sinus of the aorta (H) is darkened, 1 and 2 - the 1st and 2nd facial sinuses (light), from which the coronary arteries arise;
b: in the case of the origin of the coronary arteries from one facial sinus of the aorta, the second (shaded) may turn out to be non-coronary. Thus, the terms “facial” and “coronal”, “non-facial” and “non-coronal” are not synonymous. Source: Bokeria L. A., Berishvili I. I. Surgical anatomy of the coronary arteries. M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2003.
Septa and grooves of the heart
The left and right ventricles are separated by a thick muscular wall. This wall is called the interventricular septum (septum interventriculare).
The interventricular septum is located inside the heart. But its location corresponds to the interventricular grooves that you can see from the outside. The anterior interventricular groove is located on the sternocostal surface of the heart . I have highlighted this furrow in green in the figure.
On the diaphragmatic surface of the heart is the posterior interventricular groove (sulcus interventricularis posterior). It is highlighted in green and indicated by the number 13.
The left and right atria are separated by the interatrial septum (septum interatriale), also highlighted in green.
From the outer part of the heart, the ventricles are separated from the atria by the coronary groove (sulcus coronarius). In the figure below you can see the coronary groove on the diaphragmatic, that is, the posterior surface of the heart. This groove is an important landmark for identifying the large vessels of the heart, which we will discuss later.
Circulation circles
Big
The powerful, large left ventricle launches arterial blood into the aorta - this is where the systemic circulation begins. It looks like this: blood is ejected from the left ventricle into the aorta, which branches into organ arteries. Then the caliber of the vessels becomes smaller and smaller, down to the smallest arterioles that approach the capillaries.
Gas exchange occurs in the capillaries, and the blood, already saturated with carbon dioxide and decay products, rushes back to the heart through the veins. After the capillaries, these are small venules, then larger organ veins that flow into the inferior vena cava (if we are talking about the torso and lower extremities) and into the superior vena cava (if we are talking about the head, neck and upper extremities).
In this figure, I have highlighted the anatomical formations that complete the systemic circulation. The superior vena cava (green, number 1) and the inferior vena cava (orange, number 3) drain into the right atrium (magenta, number 2). The place where the vena cava enters the right atrium is called the sinus vena cava (sinus venarum cavarum).
Thus, the great circle begins with the left ventricle and ends with the right atrium:
Left ventricle → Aorta → Large main arteries → Organ arteries → Small arterioles → Capillaries (gas exchange zone) → Small venules → Organ veins → Inferior vena cava/Superior vena cava → Right atrium.
When I was preparing this article, I found a diagram that I drew in my second year. It will probably show you the systemic circulation more clearly:
Small
The pulmonary (pulmonary) circulation begins with the right ventricle, which sends venous blood to the pulmonary trunk. Venous blood (be careful, this is venous blood !) is sent along the pulmonary trunk, which is divided into two pulmonary arteries. According to the lobes and segments of the lungs, the pulmonary arteries (remember that they carry venous blood) are divided into lobar, segmental and subsegmental pulmonary arteries. Ultimately, the branches of the subsegmental pulmonary arteries break up into capillaries that approach the alveoli.
Gas exchange occurs again in the capillaries . Venous blood, saturated with carbon dioxide, gets rid of this ballast and is saturated with life-giving oxygen. When the blood is saturated with oxygen, it becomes arterial . After this saturation, fresh arterial blood runs through the pulmonary venules, subsegmental and segmental veins, which drain into the large pulmonary veins. The pulmonary veins drain into the left atrium.
Here I have highlighted the beginning of the pulmonary circulation - the cavity of the right ventricle (yellow) and the pulmonary trunk (green), which leaves the heart and is divided into the right and left pulmonary arteries.
In this diagram you can see the pulmonary veins (green) flowing into the cavity of the left atrium (purple) - it is these anatomical formations that complete the pulmonary circulation.
Diagram of the pulmonary circulation:
Right ventricle → Pulmonary trunk → Pulmonary arteries (right and left) with venous blood → Lobar arteries of each lung → Segmental arteries of each lung → Subsegmental arteries of each lung → Pulmonary capillaries (entangle the alveoli, gas exchange zone) → Subsegmental/segmental/lobar veins (with arterial blood) → Pulmonary veins (with arterial blood) → Left atrium
Coronary arteries (coronary arteries)
The term “coronal” comes from the Greek “wreath, crown,” and “coronary” comes from the Latin “crown.” Both terms refer to the arteries of the heart and are absolute synonyms.
Right coronary artery and its branches
RCA - right coronary artery (RCA - right coronary artery).
Right coronary artery (RCA), right main coronary artery. The right coronary artery arises from the right aortic (1st facial) sinus, most often in the form of a trunk running posteriorly along the right atrioventricular groove, encircling the tricuspid valve, and heading towards the cross of the heart. The RCA typically arises from the right sinus of Valsalva (RSV) of the ascending aorta, passes anteriorly and to the right between the right auricle and the pulmonary artery and then descends vertically in the right atrioventricular sulcus. When the RCA reaches the acute margin of the heart, it turns to continue posteriorly in the sulcus onto the diaphragmatic surface and base of the heart.
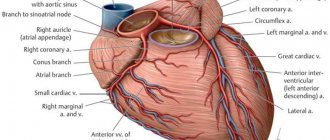
Single-plane anatomical diagram of the structure of the coronary arterial tree and the cardiac complex. A - left coronary artery (LCA) system, B: right coronary artery (RCA) system.
1 - first facial sinus of the aorta, 2 - second facial sinus of the aorta.
A - aorta, LA - pulmonary artery, ASA - right atrial appendage, LAA - left atrial appendage, LAD - anterior interventricular branch, OB - circumflex branch, DV - diagonal branch, VTK - obtuse edge branch, ASU - sinus node artery, CA - conal artery, BOK - branch of the acute edge, a.AVU - artery of the atrioventricular node, ZAMV - posterior interventricular branch. Source: Bokeria L. A., Berishvili I. I. Surgical anatomy of the coronary arteries.
M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2003. CA – conal artery (branch of the conus arteriosus). Conus branch, infundibular branch, conus arteriosus branch.
The conus artery is the first major branch of the right coronary artery, but it can arise as an independent orifice from the 1st facial sinus of the aorta. The conus artery supplies the conus arteriosus and the anterior wall of the right ventricle and may participate in the blood supply to the anterior interventricular septum.
The artery has a variable distribution, but usually supplies a region of the anterior interventricular septum and the cone of the main pulmonary artery (hence its name). Although an acute occlusion of the tiny artery has been shown to result in ST elevation, another more important role it serves in pathophysiology is that of a route of collateral circulation. The conus artery has been shown to collateralise with the more distal acute marginal branch in RCA stenosis/obstruction, and collateralise with the left anterior descending artery (LAD) in LAD stenosis/obstruction, providing a potentially vital collateral pathway.
ASU – artery of the sinus node (branch of the sinus node, artery of the sinoatrial node (a.SNA), branch of the sinoatrial node). Sinoatrial nodal artery (SANa), sinus node artery, sinoatrial nodal branch, SA nodal artery, right SA node branch.
The sinus node artery is the main artery providing blood supply to the sinoatrial node, and its damage leads to irreversible disturbances in heart rhythm. The ASU is also involved in the blood supply to most of the interatrial septum and the anterior wall of the right atrium.
The artery of the sinus node, as a rule, arises from the dominant artery (see types of blood supply to the heart). With the right type of blood supply to the heart (in approximately 60% of cases), the ASU is the second branch of the right coronary artery and departs from the RCA opposite the origin of the conus artery, but can also arise from the 1st facial sinus independently. With the left type of blood supply to the heart, the artery of the sinus node arises from the circumflex branch of the left artery.
The sinoatrial nodal artery (SANa) supplies blood to the sinoatrial node (SAN), Bachmann's bundle, crista terminalis, and the left and right atrial free walls. The SANA most frequently originates from either the right coronary artery (RCA) or the left circumflex branch (LCX) of the left coronary artery (LCA).
Kugel's artery (great auricular artery). Kugel's artery, atrial anastomotic branch, Kugel's anastomotic branch (Lat.: arteria auricularis magna, arteria anastomotica auricularis magna, ramus atrialis anastomoticus).
Kugel's artery is an anastomosing between the systems of the right and left coronary arteries. In 66% of cases, it is a branch of the LCA or the SPU artery arising from it, in 26% - a branch of both coronary arteries or the SPU artery, arising from them simultaneously, and in 8% of cases - a branch of smaller branches arising from the right and left coronary arteries arteries to the atria.
ADVa. – adventitial artery.
The third branch of the PCA. The adventitial artery can be a branch of the conus artery or arise independently from the aorta. It goes up and to the right and lies on the anterior wall of the aorta (above the sinotubular junction), heading to the left and disappearing into the fatty sheath surrounding the great vessels.
AOK - artery of the acute edge (right marginal artery, right marginal branch, branch of the acute edge). Acute marginal artery, right marginal branch, right marginal artery.
The acute margin artery is one of the largest branches of the RCA. It descends from the RCA along the sharp right edge of the heart and forms powerful anastomoses with the LAD. Participates in nutrition of the anterior and posterior surfaces of the acute edge of the heart.
a.PVH - artery of the atrioventricular node (artery of the atrioventricular node). AV node artery, AV nodal artery (branch), AVN artery.
The artery (branch) of the atrioventricular node arises from the RCA in the area of the cross of the heart.
Posterior interventricular branch, posterior interventricular artery, posterior descending artery. Posterior descending artery (PDA), posterior interventricular artery (PIA).
The posterior interventricular branch can be a direct continuation of the RCA, but is more often a branch of it. It passes in the posterior interventricular groove, where it gives off posterior septal branches, which anastomose with the septal branches of the LAD and supply the terminal sections of the conduction system of the heart. With the left type of blood supply to the heart, the LAD receives blood from the left coronary artery, departing from the circumflex branch or LAD.
Posterior septal branches, inferior septal (septal) branches. Posterior septal perforators, posterior septal (perforating) branches.
The posterior (“lower”) septal branches arise from the LAD in the posterior interventricular groove, which anastomose with the “anterior” septal (septal) branches of the LAD and supply the terminal sections of the conduction system of the heart.
Posterolateral branch of the left ventricle (posterolateral left ventricular branch). Right posterolateral artery, posterolateral artery (PLA), posterior left ventricular (PLV) artery.
In approximately 20% of cases, the RCA forms the posterolateral branch of the left ventricle.
Left coronary artery and its branches
LCA – left coronary artery (LCA – left coronary artery, OS LCA – main trunk of the left coronary artery, trunk of the left coronary artery, main trunk of the left coronary artery).
Left coronary artery (LCA), left main coronary artery (LMCA), main stem of the left coronary artery, left main stem. As a rule, the left coronary artery arises with one trunk from the left (2nd facial) sinus of the aorta. The left artery trunk is usually short and rarely exceeds 1.0 cm, bends around the pulmonary trunk from behind, and at the level of the nonfacial sinus of the pulmonary artery is divided into branches, usually two: LAD and OB. In 40-45% of cases, the LCA, even before dividing into the LAD and OB, can give off the artery that supplies the sinus node. This artery can also arise from the OB of the LCA. The LMCA typically originates from the left sinus of Valsalva (LSV), passes between the right ventricle outflow tract and the left auricle and quickly bifurcates into the LAD and the LCX arteries. Its normal length varies from 2 mm to 4 cm.
Trunk of the left coronary artery - division into LAD and OB
Source: Coronary anatomy and anomalies.
Robin Smithuis and Tineke Willems. Radiology department of the Rijnland Hospital Leiderdorp and the University Medical Center Groningen, the Netherlands. LAD – anterior interventricular branch (anterior descending artery, left anterior descending artery, left anterior interventricular artery). Left anterior descending artery (LAD), anterior interventricular artery (AIA), anterior descending coronary artery.
The anterior interventricular branch arises from the left artery trunk and follows down along the anterior interventricular septum. In 80% of cases, it reaches the apex and, going around it, moves to the back surface of the heart.
Right ventricular branch
The right ventricular branch is a non-permanent branch of the LAD and arises from the LAD on the anterior surface of the heart.
Septal branches of the LAD (septal branches of the LAD, “anterior” septal branches). Septal perforators, the septal branches (arteries), the septal perforator branches, perforator branches.
The septal branches of the LAD vary greatly in size, number, and distribution. The large first septal branch of the LAD (also known as the anterior septal branch, anterior septal artery, 1st SV) supplies the anterior part of the interventricular septum and participates in the blood supply to the conduction system of the heart. The remaining septal branches of the LAD (“anterior”) are usually smaller in size. They communicate with similar septal branches of the cervical vein (“lower” septal branches).
Diagonal branch of the LAD (DV - diagonal branches, diagonal arteries). Diagonal arteries (DB - diagonal branches), the diagonals.
Diagonal branches arise from the LAD and follow along the anterolateral surface of the left ventricle. There are several of them, designated by numbers from top to bottom: 1st, 2nd, 3rd diagonal arteries (branches). They supply blood to the anterior part of the left ventricle. The first diagonal branch is usually one of those branches that feeds the apex.
Median artery (intermediate branch) Intermediate artery, intermediate branch, ramus intermedius (RI), median (intermedian) branch.
In approximately 20-40% of cases, the LMCA trunk is divided not into two, but into three branches: the “diagonal branch” departs from the LMCA trunk along with the OB and LAD, and in this case it is called the median artery. The median artery is the equivalent of the diagonal branch and supplies the free wall of the left ventricle.
The ramus intermedius (RI) is an artery arising between the left anterior descending artery (LAD) and the CX. Some call it a high diagonal (D) or a high obtuse marginal (OM) artery.
In this normal variant, the LMCA can trifurcate into a LAD, a LCX and a ramus intermedius. The ramus intermedius typically supplies the lateral and inferior walls, acting as a diagonal or obtuse marginal branch, while the arteries that usually supply this territory are small or absent.
Median artery
Source: Coronary anatomy and anomalies.
Robin Smithuis and Tineke Willems. Radiology department of the Rijnland Hospital Leiderdorp and the University Medical Center Groningen, the Netherlands. OB – circumflex branch of the left coronary artery, circumflex artery. Left circumflex coronary artery (LCX), circumflex artery (CX, CA).
The circumflex branch is a large branch of the LMCA; in some cases it can branch off from the left aortic sinus independently. It follows along the left atrioventricular groove, goes around the mitral valve, the left (obtuse) edge of the heart, and passes to its diaphragmatic surface. Typically, the OB gives off the left fragment of the Kugel artery, and although more often it does not reach the sinus node, in 10-12% of cases the artery of the sinus node can be formed by this branch.
VTK - branch of the obtuse edge (left marginal (marginal) branch, artery of the obtuse edge). Obtuse marginal artery, the obtuse marginals, the obtuse marginal (OM) branch, the left marginal arteries.
The obtuse margin branch is the largest branch of the OB and can arise both from the beginning of the OB and at the level of the obtuse margin. This is a very important branch involved in feeding the free wall (its anterior and posterior surfaces) of the LV along its lateral edge. Very often, the OM system is generally represented by a large VTK and unexpressed OM. There can be several branches of the obtuse edge, then they are designated by numbers as they extend from left to right: 1st, 2nd, 3rd.
Left atrial branch.
The left atrial branch may arise from the OB. It nourishes the lateral and posterior surface of the left atrium.
Posterolateral branch (left ventricular branch). Posterolateral branch (PLB).
The posterolateral branch is most often the terminal branch of the OB, but the origin of this branch, as well as the LMVA and the artery of the atrioventricular node from the OB LCA, is determined by the dominance of the right or left coronary artery.
External structure of the heart
The heart (cor) has the shape of a truncated cone, which is located in the anterior mediastinum with the apex to the left and down. The apex of this cone has the anatomical name "apex cordis", so you won't get confused. Look at the illustration and remember - the top of the heart is at the bottom, not at the top.
The top of the heart is called the base of the heart (basis cordis). You can show the base of the heart on the specimen if you simply circle the area into which all the major vessels of the heart enter and exit. This line is quite conventional - as a rule, it is drawn through the opening for the inferior vena cava.
The heart has four surfaces:
- Diaphragmatic surface (facies diaphragmatica). Located below, it is this surface of the heart that is directed towards the diaphragm;
- The sternocostal surface (facies sternocostalis). This is the anterior surface of the heart, it faces the sternum and ribs;
- Pulmonary surface (facies pulmonalis). The heart has two pulmonary surfaces - right and left.
In this picture we see the heart in combination with the lungs. Here is the sternocostal, that is, the anterior surface of the heart.
There are small projections at the base of the sternocostal surface. These are the right and left appendages (auricula dextra / auricula sinistra). I highlighted the right ear in green, and the left ear in blue.
Types of blood supply to the heart Type of dominance (Coronary dominance)
The myocardial distribution of the coronary arteries is somewhat variable, but the right coronary artery (RCA) almost always supplies the right ventricle (RV), and the left coronary artery (LCA) supplies the anterior portion of the ventricular septum and anterior wall of the left ventricle (LV). The vessels that supply the remainder of the LV vary depending on the coronary dominance. Read More: https://www.ajronline.org/doi/10.2214/AJR.06.1295
The posterior descending artery (PDA) runs in the posterior interventricular groove and supplies the inferior wall and inferior third of the interventricular septum. The artery that supplies the PDA and a posterolateral branch determines the coronary dominance, so there can be three situations:
Right type of blood supply to the heart. Right dominant heart, RCA dominance, right-dominance, right dominant circulation.
Most hearts (approximately 70% of cases) are right dominant where the posterior descending artery (PDA) and the posterolateral branch are supplied by the right coronary artery (RCA). In this instance, the RCA supplies the inferoseptal and inferior segments of the left ventricle.
Left type of blood supply to the heart. Left dominant heart, LCA dominance, left dominant circulation.
In 10% of cases the PDA is supplied by the LAD or LCx.
Mixed type of blood supply to the heart. Codominant heart, codominance.
In 20% of cases a single or duplicated PDA and posterolateral branches are supplied by branches of both the RCA and LAD/LCx.
Dominant right coronary artery and its branches.
Right type of blood supply to the heart. Schematic structure of the right coronary artery (antero-posterior projection). AV = atrioventricular, PDA = posterior descending artery, RCA = right coronary artery, RV = right ventricular, SA = sinoatrial.
Dominant left coronary artery and its branches.
Schematic structure of the left coronary artery with the left type of blood supply to the heart (left anterior oblique projection).
AVGA = atrioventricular groove artery, PDA = posterior descending artery. Source: Sunil Kini, Kostaki G. Bis, and Leroy Weaver. Normal and Variant Coronary Arterial and Venous Anatomy on High-Resolution CT Angiography. American Journal of Roentgenology 2007 188:6, 1665-1674.
Literature and Internet resources:
- Bokeria L. A., Berishvili I. I. Surgical anatomy of the coronary arteries. M.: Publishing house NTsSSKh im. A. N. Bakuleva RAMS, 2003. + 297 pp., illustration.
- Nerantzis, C. E., Marianou, S. K., Koulouris, S. N., Agapitos, E. B., Papaioannou, J. A., & Vlahos, L. J. (2004). Kugel's artery: an anatomical and angiographic study using a new technique. Texas Heart Institute journal, 31(3), 267–270.
- Vikse, J., Henry, B. M., Roy, J., Ramakrishnan, P. K., Hsieh, W. C., Walocha, J. A., & Tomaszewski, K. A. (2016). Anatomical Variations in the Sinoatrial Nodal Artery: A Meta-Analysis and Clinical Considerations. PloS one, 11(2), e0148331. doi:10.1371/journal.pone.0148331.
- Rahalkar, A. M., & Rahalkar, M. D. (2009). Pictorial essay: Coronary artery variants and anomalies. The Indian journal of radiology & imaging, 19(1), 49–53. doi:10.4103/0971-3026.45345.
- Villa, A. D., Sammut, E., Nair, A., Rajani, R., Bonamini, R., & Chiribiri, A. (2016). Coronary artery anomalies overview: The normal and the abnormal. World journal of radiology, 8(6), 537–555. doi:10.4329/wjr.v8.i6.537.
- Sunil Kini, Kostaki G. Bis, and Leroy Weaver. Normal and Variant Coronary Arterial and Venous Anatomy on High-Resolution CT Angiography. American Journal of Roentgenology 2007 188:6, 1665-1674
- Siew Yen Ho. Structure and anatomy of the aortic root. European Journal of Echocardiography, Volume 10, Issue 1, January 2009, Pages i3–i10.
- radiopaedia.org
- Robin Smithuis and Tineke Willems. Coronary anatomy and anomalies. Radiology department of the Rijnland Hospital Leiderdorp and the University Medical Center Groningen, the Netherlands. www.radiologyassistant.nl
Copyright © 2008-2019 Medtran.ru. All rights reserved.
Heart valves
The right atrium from the left, as well as the right ventricle from the left, are separated by septa. Normally, in an adult, the partitions should be solid, there should be no holes between them.
But there must be a hole between the ventricle and the atrium on each side. If we are talking about the left half of the heart, then this is the left atrioventricular opening (ostium atrioventriculare sinistrum). On the right, the ventricle and atrium are separated by the right atrioventricular orifice (ostium atrioventriculare dextrum).
Valves are located at the edges of the holes. These are clever devices that prevent the blood from flowing back. When the atrium needs to send blood to the ventricle, the valve is open. After the ejection of blood from the atrium into the ventricle has occurred, the valve must close tightly to prevent blood from flowing back into the atrium.
The valve is formed by leaflets, which are double layers of endothelium - the inner lining of the heart. Tendon threads extend from the valves, which are attached to the papillary muscles. It is these muscles that control the opening and closing of the valves.
Tricuspid valve (valva tricispidalis)
This valve is located between the right ventricle and the right atrium. It is formed by three plates to which tendon threads are attached. The tendon threads themselves connect to the papillary muscles located in the right ventricle.
On a section in the frontal plane, we cannot see three plasties, but we can clearly see the papillary muscles (outlined in black) and tendon threads attached to the valve plates. The cavities that the valve separates are also clearly visible - the right atrium and the right ventricle.
On a section in a horizontal plane, the three leaflets of the tricuspid valve appear before us in all their glory:
Mitral valve (valva atrioventricularis sinistra)
The mitral valve regulates blood flow between the left atrium and the left ventricle. The valve consists of two plates, which, as in the previous case, are controlled by the papillary muscles through tendon threads. Please note - the mitral valve is the only heart valve that consists of two leaflets.
The mitral valve is outlined in green, and the papillary muscles are outlined in black:
Let's look at the mitral valve in the horizontal plane. Let me note again that only this valve consists of two plates:
Pulmonary valve (valva trunci pulmonalis)
The pulmonary valve is also often called the pulmonary valve or pulmonary valve. These are synonyms. The valve is formed by three flaps that are attached to the pulmonary trunk at its origin from the right ventricle.
You can easily find the pulmonary valve if you know that the pulmonary trunk starts from the right ventricle:
On a horizontal section, you can also easily detect the pulmonary valve if you know that it is always located anterior to the aortic valve. The pulmonary valve generally occupies the most anterior position of all the heart valves. We can easily find the pulmonary valve itself and the three valves that form it:
Aortic valve (valva aortae)
We have already said that the powerful left ventricle sends a portion of fresh, oxygenated blood to the aorta and further in a large circle. The aortic valve separates the left ventricle and the aorta. It is formed by three plates that are attached to the annulus fibrosus. This ring is located at the junction of the aorta and the left ventricle.
When examining the heart in a slice in a horizontal plane, do not forget that the pulmonary valve is in front, and the aortic valve is behind it. The aortic valve is surrounded by all the other valves from this angle:
Topography of the heart
Remember in the last lesson on basic chest topography I said that without knowing topographic lines you will not be able to learn anything related to the chest cavity? Have you learned them? Great, arm yourself with your knowledge, now we will use it.
So, the boundaries of absolute cardiac dullness and relative cardiac dullness are distinguished.
This strange name comes from the fact that if you tap (in medicine this is called “percussion”) the chest, in the place where the heart is located, you will hear a dull sound. When percussed, the lungs are more sonorous than the heart, which is where this term comes from.
Relative dullness is the anatomical ( true ) boundaries of the heart. We can establish the limits of relative dullness during the autopsy. Normally, the heart is covered by the lungs, so the boundaries of relative cardiac dullness are visible only on the preparation.
Absolute cardiac dullness is the boundaries of the part of the heart that is not covered by the lungs. As you understand, the limits of absolute cardiac dullness will be less than the limits of relative cardiac dullness in the same patient.
Since we are now examining anatomy, I decided to talk only about the relative, that is, the true boundaries of the heart. After the article about the anatomy of the hematopoietic system, I generally try to keep track of the size of the articles.
Boundaries of relative cardiac dullness (true boundaries of the heart)
- Apex of the heart (1): 5th intercostal space, 1-1.5 centimeters medial to the left midclavicular line (highlighted in green);
- Left border of the heart (2): a line drawn from the intersection of the third rib with the parasternal line (yellow) to the apex of the heart. The left border of the heart is formed by the left ventricle. In general, I advise you to remember the third rib - you will constantly encounter it as a landmark for various anatomical formations;
- The upper bound (3) is the simplest. It runs along the upper edge of the third ribs (we see the third rib again) from the left to the right parasternal lines (both yellow);
- Right border of the heart (4): from the upper edge of the 3rd (again) to the upper edge of the 5th rib along the right parasternal line. This border of the heart is formed by the right ventricle;
- Inferior border of the heart (5): a horizontal line drawn from the cartilage of the fifth rib along the right parasternal line to the apex of the heart. As you can see, the number 5 is also very magical in terms of determining the boundaries of the heart.
Conduction system of the heart. Pacemakers.
The heart has amazing properties. This organ is capable of independently generating an electrical impulse and conducting it through the entire myocardium. Moreover, the heart can independently organize the correct rhythm of contraction, which is ideal for delivering blood throughout the body.
Once again, all skeletal muscles and all muscular organs are capable of contracting only after receiving an impulse from the central nervous system. The heart is capable of generating an impulse on its own .
The conduction system of the heart is responsible for this - a special type of cardiac tissue that can perform the functions of nervous tissue. The conduction system of the heart is represented by atypical cardiomyocytes (literally translated - “atypical cardiomuscular cells”), which are grouped into separate formations - nodes, bundles and fibers. Let's look at them.
1. Sinatrial node (nodus sinatrialis) . The author's name is the Kissa-Fleck knot. It is also often called the sinus node. The sinatrial node is located between the junction of the superior vena cava into the right ventricle (this place is called the sinus) and the appendage of the right atrium. "Sin" means "sine"; “atrium,” as you know, means “atrium.” We get - “sinatrial node”.
By the way, many who begin to study ECG often wonder what is sinus rhythm and why is it so important to be able to confirm its presence or absence? The answer is quite simple.
The sinus node is the first order pacemaker. This means that normally it is this node that generates excitation and transmits it further along the conduction system. As you know, in a healthy person at rest, the synatrial node generates from 60 to 90 impulses, which coincides with the pulse rate. Such ri, since it is generated exclusively by the synatrial node.
You can find it on any anatomical tablet - this node is located above all other elements of the conduction system of the heart.
2. Atrioventricular node (nodus atrioventricularis) . The author's name is the Ashshof-Tavara knot. It is located in the interprestrial septum just above the tricuspid valve. If you translate the name of this node from Latin, you will get the term “atrioventricular node,” which exactly corresponds to its location.
The atrioventricular node is a second- order pacemaker. If the atrioventricular node has to start the heart, then the sinatrial node is turned off. This is always a sign of serious pathology. The atrioventricular node is capable of generating excitation with a frequency of 40-50 impulses. Normally, it should not generate excitement; in a healthy person, it only works as a conductor.
The antrioventricular node is the second node from above after the sinatrial node. Identify the sinatrial node - it is the highest - and immediately below it you will see the atrioventricular node.
How are the sinus and atrioventricular nodes connected? There are studies that suggest the presence of three bundles of atypical cardiac tissue between these nodes. Officially, these three bundles are not recognized in all sources, so I did not separate them into a separate element. However, in the picture below I have drawn three green tufts - front, middle and back. This is approximately how these internodal bundles are described by the authors who acknowledge their existence.
3. Bundle of His, often called the atrioventricular bundle (fasciculus atrioventricularis) .
After the impulse has passed through the atrioventricular node, it diverges into two sides, that is, into two ventricles. The fibers of the conduction system of the heart, which are located between the atrioventricular node and the point of division into two parts, are called the bundle of His.
If, due to some serious illness, both the synatrial and atrioventricular nodes are switched off, then the His bundle has to generate excitation. third pacemaker . It is capable of generating 30 to 40 pulses per minute.
For some reason I depicted the His bundle in the previous step. But in this one I’ll highlight it and sign it so that you remember it better:
4. Legs of the bundle of His, right and left (crus dextrum et crus sinistrum) . As I already said, the bundle of His is divided into right and left branches, each of which goes to the corresponding ventricles. The ventricles are very powerful chambers, so they require separate branches of innervation.
5. Purkinje fibers . These are small fibers into which the bundle branches crumble. They entwine the entire ventricular myocardium in a fine network, ensuring complete conduction of excitation. If all other pacemakers are turned off, then Purkinje fibers will try to save the heart and the entire body - they are capable of generating a critically dangerous 20 impulses per minute. A patient with such a pulse requires emergency medical attention.
Let's consolidate our knowledge of the conduction system of the heart with another illustration:
Layers of the Heart
1. Pericardium . This is a dense connective tissue membrane that reliably covers the heart.
The pericardium is a two-layer membrane; it consists of fibrous (outer) and serous (inner) layers. The serous layer is also split into two plates - parietal and visceral. The visceral plate has a special name - epicardium .
In many authoritative sources you can see that the epicardium is the first lining of the heart.
2. Myocardium (myocardium). The actual muscle tissue of the heart. This is the most powerful layer of the heart. The most developed and thick myocardium forms the wall of the left ventricle, as we already discussed at the beginning of the article.
See how the thickness of the myocardium differs in the atria (using the example of the left atrium) and in the ventricles (using the example of the left ventricle).
3. Endocardium (endocardium). This is a thin plate that lines the entire internal space of the heart. The endocardium is formed by endothelium - a special tissue consisting of epithelial cells tightly adjacent to each other. The development of atherosclerosis, hypertension, myocardial infarction and other serious cardiovascular diseases is associated with endothelial pathology.
Heart fixation device
The heart is a critical organ. The heart should not move freely in the chest cavity, so it has its own fixation apparatus. Here's what it consists of:
- The large vessels of the heart are the aorta, pulmonary trunk and superior vena cava. In thin people with an asthenic body type, the heart is located almost vertically. It is literally suspended on these large vessels, in which case they are directly involved in fixing the heart;
- Uniform pressure from the lungs;
- The upper pericardial ligament (ligamentun sternopericardiaca superior) and the lower pericardial ligament (ligamentun sternopericardiaca inferior). These ligaments attach the pericardium to the posterior surface of the manubrium of the sternum (superior ligament) and the body of the sternum (inferior ligament);
- A powerful ligament that connects the pericardium to the diaphragm. I did not find a Latin name for this ligament, but I did find a drawing from my favorite atlas of topographic anatomy. Of course, this is the atlas of Yu.L. Zolotko. I have outlined the link in this illustration with a green dotted line:
Venous drainage from the heart
The venous system of the heart begins with tiny venules that collect into larger veins. These veins in turn empty into the coronary sinus , which opens into the right atrium. As you remember, all venous blood of the entire body collects in the right atrium, and blood from the heart muscle is no exception.
Let's look at the heart from the diaphragmatic surface. The opening of the coronary sinus is clearly visible here - it is highlighted in green and is indicated by the number 5.
The great vein of the heart lies in the anterior interventricular groove . It begins on the anterior surface of the apex of the heart, then lies in the anterior interventricular groove, then in the coronary groove. In the coronary sulcus, the large vein bends around the heart backward and to the left, flowing on the posterior surface of the heart into the right atrium through the coronary sinus.
Please note - unlike the arteries, the great vein of the heart is located both in the anterior interventricular sulcus and in the coronary sulcus. This is still a large vein of the heart:
The middle cardiac vein passes from the apex of the heart along the posterior interventricular groove and flows into the right end of the coronary sinus.
The small vein of the heart (vena cordis parva) lies in the right coronary sulcus. In the direction to the right and back, it goes around the heart, flowing into the right atrium through the coronary sinus. In this picture, I highlighted the middle vein in green, and the small vein in yellow.