Definition:
Myocardial revascularization is the restoration of the patency of the arteries of the heart (coronary arteries) through surgery.
Such operations include:
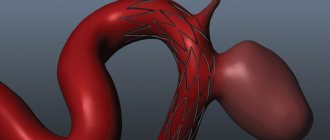
- Percutaneous coronary intervention (stenting, angioplasty). The main idea of these operations is to restore and maintain blood flow in the vessels. A stent is passed and placed into the heart arteries by first dilating the artery with a balloon. A stent is a thin metal wire tube. By expanding the artery and thereby increasing its diameter, the stent further preserves the lumen of the artery. This is a more gentle operation than coronary artery bypass grafting. It is performed under local anesthesia, without anesthesia.
- The coronary artery bypass surgery involves sewing additional vessels (shunts) to the ascending aorta, which will supply blood to the area of the heart suffering from a lack of blood and oxygen. Arteries located in the chest, veins in the legs and some other vessels are used as additional vessels. The operation is performed on a stopped heart, and the patient is connected to a heart-lung machine.
- An additional way to improve blood supply to the heart is laser revascularization of the myocardium. The operation consists of “burning” the myocardium (heart muscle) with a special laser in order to form small holes in it, which helps to increase blood supply to this area of the heart.
Direct interventions on the brachiocephalic arteries in acute stroke
CEA for small strokes and TIA
The preventive focus of CEA and the desire of surgeons to level out the risk of intra- and postoperative complications and mortality have over time ensured a certain status of this operation. CEA is a planned surgical intervention in patients with mild strokes and the absence of significant concomitant pathology. Until relatively recently, CEA was contraindicated in patients up to 6 weeks after a stroke and in patients with persistent severe neurological deficits [2]. The reason for refusing early interventions was the surgeons’ belief in the high probability of developing hyperperfusion cerebral edema, hemorrhagic complications, and the futility of surgery for severe strokes [2]. However, the risk of recurrent ischemic events is highest in the first days and weeks after the onset of stroke symptoms, amounting to 1-2% in the first 7 days and 2-4% in the first 30 days [12]. After conducting large international studies, it became clear that the preventive value of CEA decreases with increasing time before surgery. Thus, according to the NASCET study [13], repeated strokes developed in 9.5% of patients awaiting CEA [13]. Performing CEA in the early stages (1-14 days) after a stroke can prevent 1 stroke in 5 patients during 5 years of observation, and performing the operation later than 6 months prevents 1 stroke in 125 patients during the same observation period [3, 14]. It was also found that early CEA in patients with minor strokes and TIAs is not accompanied by an increased risk of ischemic and hemorrhagic complications [4, 5, 15]. There are studies proving the safety and effectiveness of CEA in the early period of non-severe stroke [3-5, 16-19]. Thus, E. Ballotta et al. [18] analyzed the results of treatment of 102 patients with acute strokes. The operation was performed in the first 14 days (median - 8 days) in patients with stable neurological deficit (no increase in symptoms within 24 hours) and a level of neurological disorders less than 2 points on the Rankin scale. The authors showed that the best treatment outcomes were in patients with mild stroke, absence or presence of small foci of ischemia on computed tomography (CT). C. Peiper et al. [19] compared the effectiveness of 26 emergency and 157 delayed (after 14 days) CEA in patients who had suffered a minor stroke. Indications for emergency surgery were the presence of symptoms of cerebrovascular insufficiency and complicated atherosclerotic plaque. The best results were obtained in patients operated on early; no cases of mortality or complications were noted. In patients operated on in the late period of acute stroke, intra- and postoperative ischemic complications were 3.8%, and mortality was 2.7%. According to S. Annambhotla et al. [17], better long-term results and fewer postoperative complications are observed in patients operated on in the first 30 days after stroke. Thus, in the group of patients operated on early, recurrent IS was noted in 2.3% of patients during 17 months of observation, mortality within 5 years was 21%, and in the group of patients operated on in the late period (more than 30 days after II), 8.3% of recurrent strokes were registered within 12 months, the mortality rate over 5 years was 30% [17].
CEA for progressive strokes (stroke in progress) and crescendo TIA[1]
The question of the possibility and necessity of CEA in patients with progressive neurological deficit (stroke in progress), disabling stroke and crescendo TIA (more than 2 episodes of TIA within 24 hours) remains poorly understood and controversial. There are no large randomized studies on this issue.
National recommendations indicate that in patients who have suffered a complete stroke, it is advisable to perform surgical treatment within 6 to 8 weeks from the onset of the acute episode, but there is no information on the tactics of managing stroke during the course and crescendo TIA [1].
The main purpose of CEA for progressive stroke or crescendo TIA is not only early prevention of recurrent ischemic episodes, but also emergency restoration of normal perfusion in the penumbra to prevent further increase in neurological deficit. In this case, CEA is both a preventive and therapeutic procedure. The main obstacle to the routine use of such operations is the existing risk of hemorrhagic complications, which is 0-2% [6, 9, 21].
In recent years, the interest of researchers and surgeons in performing early CEA for acute strokes of varying severity and course has been growing. The timing, indications, acceptable percentage of complications, surgical technique, the need to use an intraluminal shunt and an expanding patch, and the optimal types of anesthesia for this category of patients are discussed [6-10, 12, 22]. Thus, S. Bruls et al. [8] believe that the course of stroke in progress and crescendo TIA are extremely unfavorable (mortality is 14-18%, disability reaches 31-71%) and allow emergency surgical intervention in patients without impairment of consciousness. L. Capoccia et al. [9] presented their experience of treating 48 patients with progressive stroke (26 people) and crescendo TIA (23). The severity of the patients' condition upon admission averaged 5.3 points according to NIHSS; foci of ischemia on CT were detected in 4 (15.3%) patients with stroke and 8 (34.8%) with repeated TIAs. The operation was performed within the first 24 hours (median: 10 hours) from the onset of the ischemic episode. The researchers noted significant improvements in functional outcomes in most patients; the mean level of neurological impairment at discharge was 0.54 NIHSS points. Postoperative complications were observed in 1 (2%) patient in the form of hemorrhagic transformation of the ischemic lesion, not detected by CT, which led to the death of the patient.
According to R. Brandl et al. [7], the indications for emergency CEA in acute progressive stroke are: the presence of symptoms of acute stroke with unstable neurological deficit, but the absence of disorders of consciousness; the presence of significant carotid pathology; absence of hemorrhagic changes in the brain substance; stable hemodynamics and respiratory functions of the patient.
The possibility of performing emergency CEA in patients with moderate and severe neurological deficits has been demonstrated [6, 10, 11, 20]. For example, E. Sbarigia et al. [20] analyzed the results of treatment of 96 patients with acute IS and severe neurological deficit. All patients were operated on within the first 2 days from the onset of the disease (median - 1.5 days). Surgery was abstained in patients with a severity of neurological disorders of more than 22 points according to NIHSS and cerebral infarctions extending to more than ⅔ of the blood supply of the corresponding middle cerebral artery (MCA). In 85 (88.5%) patients, a decrease in neurological deficit was noted in the postoperative period. The combined mortality rate + complications was 7.3%; there were no hemorrhagic complications or an increase in the volume of the ischemic lesion.
L. Capoccia et al. [10] described 62 cases of emergency CEA (median: 34 hours). The authors noted more significant dynamics of regression of neurological deficit in the group of patients with initially more severe neurological disorders (more than 8 points according to NIHSS) compared to patients with less severe disorders (4-7 points according to NIHSS).
Along with supporters of active surgical tactics for acute severe or unstable stroke, its opponents claim that the level of postoperative complications and mortality is too high. R. Huber et al. [23] and S. Welsh et al. [13] reported 16% mortality and 21% complications in this category of patients. K. Rerkasem et al. [24] reviewed 47 literature sources on CEA in patients with ongoing stroke; According to researchers, surgery in the acute stage of stroke can be accompanied by complications in 20.2% of cases and 11.4% mortality. According to the latest recommendations of the American Stroke Association (AHA/ASA) [25], emergency CEA for severe strokes and unstable neurological deficits should be performed only to eliminate the cause of acute thrombosis or blood flow deficiency. CEA is not indicated for major stroke due to the high risk of damage to brain tissue when blood flow is restored.
H. Bazan et al. [26] studied factors influencing the outcomes of emergency CEA. Lethal outcomes and ischemic complications during emergency interventions were more common than in the group of patients who underwent planned operations: mortality - 2.0 and 0.3%, IS - 2.9 and 1.1%, respectively. The number of cardiac complications was statistically comparable in both groups and amounted to 2.2-3.0%. In patients with severe concomitant pathology, the risk of postoperative complications and mortality was significantly higher - 10.9 and 7.8% in the groups considered. The authors concluded that the risk of emergency CEA is higher in patients with high comorbidity; these patients require careful selection and treatment in large multidisciplinary centers. According to G. Leseche et al. [27], among 27 patients with acute progressive stroke, the most common somatic pathology was arterial hypertension - 77.7%, history of smoking - 70.3%, hypercholesterolemia - 63.0%, chronic obstructive pulmonary diseases - 40.7%, atrial fibrillation - 18.5%, angina - 14.8%, kidney disease - 14.8%. All patients underwent emergency CEA. A postoperative complication occurred in 1 (3.7%) patient who developed a non-fatal myocardial infarction. There were no deaths.
Selective intraluminal shunting for acute stroke is the subject of debate in the literature; There are studies indicating the need for mandatory intraluminal shunting during CEA. The use of this technique provides additional protection of brain tissue from ischemia and hemodynamic shock after the start of blood flow [28]. The use of an expanding patch when closing an arteriotomy defect in emergency patients is preferred by most surgeons, citing better prevention of narrowing and thrombosis of the artery [14, 28, 29]. In order to reduce the risk of intra- and postoperative complications, the following technical actions are also proposed: a wider soft tissue incision; availability of a ready-to-use intraluminal shunt; preliminary clamping of the common (CA) and external carotid arteries before dissection of the carotid bulb to exclude thromboembolism; a wide arteriotomy sufficient to visualize the entire surface of the endarterectomy; starting retrograde blood flow from the internal carotid artery (ICA) before applying a clamp if the stenosis is accompanied by the presence of a floating thrombus [27].
Emergency thrombinthymectomy (TIE) for non-occlusive thrombosis of the ICA
Parietal, non-occlusive, incomplete thrombosis of the extracranial sections of the ICA and CCA is a rare pathology that occurs in 0.5 - 0.9% of patients with stroke and damage to the brachiocephalic arteries [16, 30, 31]. As a rule, young and middle-aged patients suffer. The causes of non-occlusive thrombosis can be atherosclerosis, damage to the vascular wall, activation of platelets and coagulation factors. Among the diseases that promote thrombus formation are various vasculopathies, antiphospholipid syndrome, systemic connective tissue diseases, and blood diseases [16]. Despite its rare occurrence, parietal thrombosis, especially in the presence of a floating fragment of a thrombus, is a dangerous condition, since in 87.5-100% it leads to thromboembolism and ischemic disorders in the brain [16, 30, 31]. The use of duplex scanning makes it possible to diagnose incomplete thrombosis in 62.5 - 100% of cases, and digital subtraction angiography - in 100% [16, 30]. Computed tomography and magnetic resonance angiography are unable to detect thrombosis in 33.4 and 66.7% of patients, respectively [30].
There is still no common point of view on the treatment tactics of this disease [16, 30, 31]. There are opinions about the need for conservative management of such patients [16, 31]. Thus, Y. Inatomi et al. [31] observed 14 patients with IS and parietal thrombosis of the ICA; patients were treated conservatively with good results. A.O. Chechetkin and O.V. Lagoda [16] analyzed the treatment outcomes of 6 patients; 4 patients received anticoagulant and antiplatelet therapy, 2 received surgical treatment. Repeated thrombosis was noted in 1 (50%) patient after CEA. The authors consider hyperhomocysteinemia detected in the patient to be a possible cause of the complication. In the conservative treatment group, 3 (75%) patients achieved a positive effect and regression of thrombosis within 1 month of treatment. E. Ferrero et al. [30], on the contrary, used surgical tactics in 16 patients with floating thrombosis of the ICA bifurcation. All patients underwent emergency CEA. Improvement in neurological symptoms was noted in 75% of patients; postoperative mortality was 6.25%.
The question of the safety of performing CEA after thrombolysis in the presence of residual significant stenosis of the ICA by thrombotic masses also remains unresolved [27, 29, 31].
M. Rubiera et al. [32] found that residual severe stenosis of the carotid artery is an independent predictor of early reocclusion of the precerebral and intracranial arteries.
G. Leseche et al. [27] operated on 7 patients after thrombolysis, 4 of whom had floating ICA thrombosis. The level of neurological disorders before surgery averaged 9 points according to NHINSS. Patients with floating thrombosis received preliminary therapy with anticoagulants and were operated on under anesthesia. There were no postoperative complications; all patients experienced partial or complete regression of neurological symptoms (up to 2 points or less on the Rankin scale during 3 months of observation). J. Crozier et al. [29] also confirm the safety of performing CEA within 1 to 22 days after thrombolysis. In their series of observations, the authors noted the absence of mortality and serious complications.
Emergency TIE for occlusive thrombosis of the ICA
The etiology of acute occlusive and non-occlusive thrombosis of the ICA is similar, but there are also differences. The incidence of occlusive thrombosis of the ICA reaches 1.9% among patients with IS; middle-aged and elderly patients are more susceptible to it, and the main causes are atherosclerotic lesions, intimal dissection of the artery, and cardioembolism [16, 33, 34]. Acute occlusion of the ICA can be asymptomatic, or can cause a brain catastrophe [2, 16]. According to a German multicenter study [35], among 4157 stroke patients, 366 (8.8%) had acute ICA occlusion. Of these, 7.4% experienced repeated ischemic episodes during the first 72 hours of observation. Mortality was 21.2% in the first 3 months of the disease.
In recent years, due to the development of neuroimaging and interventional techniques using endovascular thrombus extraction, it has become possible to achieve restoration of the arterial lumen in 53-63% of patients. Existing limitations of the methods used leave the problem of common extra-intracranial thrombosis, in which mortality reaches 30-79%, unresolved [33, 34, 36].
There are no randomized studies on open TIE for acute ICA occlusions yet. A series of separate works propose the following criteria for selecting patients for surgical treatment: the presence of acute occlusion of the extracranial part of the ICA; detection of perfusion-diffusion deficiency according to MRI data; the first 3 days from the onset of the disease. Contraindications for surgery are: deep neurological deficit, impaired consciousness, severe somatic condition, foci of hemorrhagic transformation, acute perfusion deficiency in more than ⅓ of the MCA basin according to MRI, infarction more than 1 cm according to CT data, occlusion of the intracranial ICA, occlusion of the MCA [ 33, 34].
G. Kasper et al. [33] in a series of 29 observations showed successful results of TIE in the first 39 hours from the development of an ischemic episode. Restoration of antegrade blood flow along the ICA was achieved in 83% of patients. Partial or complete regression of neurological symptoms was noted in 48% of patients; increase in neurological deficit - in 7%; hemorrhagic transformation of stroke, which was the cause of death, developed in 3.6%.
B. Weis-Müller et al. [34] indicate the need to determine the diffusion-perfusion difference and patency of the supraclinoid sections of the ICA in patients with acute stroke (35 observations). In this series of observations, in 27 (77%) patients, the severity of neurological deficit corresponded to 3-5 points on the Rankin scale. The operation was performed within the first 72 hours from the development of symptoms of cerebral ischemia. In the preoperative period, 6 (17%) patients underwent thrombolysis with tissue plasminogen activator. TIE was performed from a wide arteriotomy, using a Fogarty catheter and intraoperative angiography as indicated. Restoration of antegrade blood flow through the carotid arteries was achieved in 30 (86%) patients; in 4 (11.4%) patients, due to the absence of retrograde blood flow from the distal parts of the ICA, its ligation was performed. In the postoperative period, improvement was noted in 57% of cases, and in 6% there was an increase in neurological deficit. Mortality was 6%, hemorrhagic complications were observed in 2 (6%) patients.
J. Berthet et al. [28] recommend performing TIE in the first 6 hours from the development of ICA occlusion, using intraluminal shunting and dilating artery plasty in all patients. T. Murata et al. [37] presented experience in the treatment of 3 cardioembolic thromboses of the ICA, which accounted for 0.47% of the total sample of patients with stroke (640 patients). All patients had severe neurological deficit and atrial fibrillation. Surgical recanalization was achieved in 100% of cases; regression of neurological symptoms was noted in 2 (66.7%) patients.
Indications for revascularization
Restoring the blood supply to the heart surgically is performed if there is no effect (or insufficient effect) from taking drug therapy. The choice of myocardial revascularization technique is a complex, integrated approach based on an assessment of the patient’s condition, the characteristics of coronary artery lesions, concomitant diseases, the complexity of the postoperative period, etc.
To determine the indications for a particular treatment method, it is recommended to undergo a full cardiac examination. We use modern equipment techniques, which allows us to minimize the risk of complications after operations.
If you have discovered some, even minor, signs of cardiovascular disease, do not put off visiting a doctor until later. If you need to see a cardiologist, you can do this online on our website.
conclusions
The widespread prevalence of coronary heart disease and the high risk of complications and death of patients contributes to the use of radical treatment methods. Methods of revascularization of coronary vessels make it possible to restore normal blood supply to the myocardium. The “gold standard” for providing care for acute coronary syndrome with ischemia of the heart muscle is placing a stent into the lumen of the affected area. All interventions are performed exclusively by cardiac surgeons, taking into account the patient’s indications and contraindications.