Introduction
Ischemic stroke (IS) is one of the leading causes of death and disability worldwide.
The wide prevalence and severity of the consequences of this disease make it an acute medical and social problem. In March 2021, during a discussion of the project “Stroke in Focus” by the chief specialist in medical rehabilitation of the Russian Ministry of Health, Professor G.E. Ivanova identified the insufficiently frequent use of thrombolytic therapy (TLT), which in Russia is carried out only in 3.5% of cases, as one of the problems in improving the system of medical care for stroke. The immediate goal is to increase this number to 5%, and in the future, with the advent of new technologies and tools, to 40% [1].
The first experience of using thrombolytic drugs in IS was published in the USA back in 1958 [2]. A study of the effectiveness of TLT using a fibrinolysin-heparin mixture for IS, begun in the Soviet Union in the first half of the 1960s, showed its effectiveness in the first 3-6 hours from the onset of IS. At the same time, the main indications and contraindications for TLT were determined. However, “the widespread clinical implementation of TLT was delayed due to the lack of accurate diagnosis of the nature of cerebral stroke and the significant frequency of hemorrhagic complications” [2]. A new stage in the development of TLT for IS began with the introduction into clinical practice of recombinant tissue plasminogen activator (tPA) in combination with computed tomography and magnetic resonance imaging (CT/MRI diagnostics), which make it possible to accurately determine the nature of the stroke [2]. Currently, the incidence of TLT in Europe and North America is 5–15%. In the Russian Federation, the number of TLT for IS in 2021 exceeded 13,500 procedures, and, according to the Department of Health, in the first 6 months. 2021 in Moscow, 18.7% of patients with IS who were admitted to specialized vascular centers in the first 4.5 hours of the disease received TLT [2].
Researchers evaluate systemic TLT using alteplase as the most effective and safe method of reperfusion in the first 4.5 hours from the onset of IS development [3]. The non-invasive intervention that is intravenous thrombolysis is its main advantage; the disadvantage is the inability to fully control the administration of fibrinolytic [3]. The use of alteplase is called «
the gold standard" TLT (systemic and selective) AI, since this drug has moderate selective activity, has no antigenic properties and an extremely low risk of developing allergic reactions [4].
The mastery of the systemic TLT technique by Sevastopol neurologists began in 2021 and became possible, as was said, thanks to the introduction of CT and MRI into clinical practice, which make it possible to diagnose the nature of the stroke. Creation in 2021 on the basis of the 1st city hospital named after. N.I. Pirogov Regional Vascular Center (RSC) opened up the possibility of wider use of systemic TLT in acute IS, which gradually became common practice in the neurological department for patients with acute cerebrovascular accidents. So, based on the results of 8 months. In 2021, 1226 patients with a diagnosis of IS were admitted to the RSC, of which 217 (16.8%) people were in the therapeutic window. Of these, thrombolysis was performed in 127 (13.6%) patients (with a target rate of 4%). However, both at the development stage and at the present time, questions related to the safety and effectiveness of this method, as well as individual problems of patients that limit its use, remain relevant for us, medical practitioners.
Goal of the work:
Based on personal experience in the use of TLT, try to: 1) systematize the results obtained during thrombolytic procedures, assessing their safety (development/absence of hemorrhagic complications and allergic reactions) and effectiveness, taking into account the gender and age of patients; 2) identify factors limiting the use of TLT.
Own results
Below is data describing the experience of one doctor. The counting of thrombolytic procedures used began in June 2021 (Fig. 1). In total, from June to December 2021, 44 TLT procedures were performed, from January to July 2021 - 37, thus, in total, during the period under review, this procedure was performed 81 times.
An analysis of the possibilities of use and effectiveness of TLT was carried out on the basis of data obtained for the period from January to July 2021.
Note that we were able to use TLT to help patients with IS only in 30% of cases. What factors have limited the use of TLT?
According to researchers of this problem [3], such factors are:
time of initiation of therapy;
the presence and size of a brain region with potentially reversible changes;
features of systemic and local hemodynamics;
hemostasis factors;
sensitivity of the brain substance to ischemia;
the degree of damage to the blood-brain barrier [3].
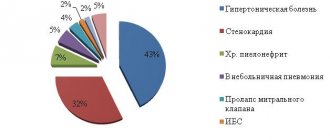
The time factor, which comes first in this list, is determined by the presence/absence of a window of therapeutic opportunity (4.5 hours from the onset of stroke). Our observations confirm its significance among all the obstacles limiting the use of TLT: out of 103 patients hospitalized by us with a diagnosis of IS, 52 (50.5%) were outside the therapeutic window (Table 1). However, in most cases, even with a window of therapeutic opportunity, we had to act under deadline conditions, since in real conditions we are often faced with the simultaneous admission of several patients requiring immediate examination and diagnostic procedures. The objective difficulties associated with this lead to inevitable losses of already strictly limited time. The speed and coherence of the actions of the medical staff involved in the TLT procedure and the uninterrupted operation of diagnostic equipment are of great, often decisive importance. Table 1 provides data illustrating the relationship between the time factor and other factors that impede TLT. Thus, the impossibility of performing thrombolysis in 17.5% of cases was associated with the presence of such contraindications in patients as uncontrolled arterial hypertension, trophic disorders in joints and limbs, and blood clotting problems. In approximately 2% of cases, we encountered patients refusing TLT.
In addition to the time factor, the presence of contraindications, the consent of the patient and his relatives when performing TLT, it is important to take into account the age of the patients. According to the instructions for use of the drug alteplase, the recommendations of the European Stroke Organization, and the Russian clinical guidelines for thrombolytic therapy for ischemic stroke [5], patients under 18 years of age should not undergo TLT, and patients over 80 years of age —
carry out with extreme caution. Most researchers agree that TLT in people over 80 years of age is not associated with an increase in complications, such as hemorrhagic transformation of the brain lesion, and, therefore, does not lead to an increase in mortality [6]. A good degree of recovery of impaired neurological functions (26–30%) serves as evidence that thrombolysis in patients aged 80–89 years and 90–99 years is equally safe and effective [6].
Regarding young patients (up to 45 years), data are provided indicating a more favorable outcome of the disease with a low incidence of symptomatic hemorrhagic transformation and a better degree of restoration of impaired neurological functions [6]. On this basis, it is concluded that TLT is effective and safe in all age groups. However, the older the patients, the higher the number of functionally unfavorable outcomes and deaths [6].
Further in our work, we tried to trace the relationship between the effectiveness and safety of TLT and the gender and age of patients. The results of TLT were assessed as follows:
positive dynamics—regression of neurological deficit with successful recanalization and reperfusion;
lack of dynamics - no changes are observed due to the lack of recanalization and/or the development of irreversible damage to the brain substance in the lesion;
negative dynamics - clinical deterioration (manifested by the development of complications, primarily hemorrhagic, reocclusion or re-embolism, or an increase in cerebral edema in case of insignificant effect of TLT).
Table 2 presents data that allows us to trace the relationship between the effectiveness of TLT and the gender and age of patients. We divided our patients into 6 age groups: 1st (20–49 years), 2nd (50–59 years), 3rd (60–69 years), 4th (70–79 years); 5th (80–89 years), 6th (90 or more years). The effectiveness and safety of TLT (positive dynamics, no dynamics, negative dynamics, absence/presence of allergic reactions) was assessed based on the results of daily observation. According to Russian clinical guidelines for thrombolytic therapy for ischemic stroke, it is necessary to monitor the dynamics of the neurological status during the day; Positive dynamics during the first 24 hours after TLT, as a rule, predict subsequent good recovery [5].
Summarizing our observations, we can provide the following data.
The total number of patients who underwent the TLT procedure was 37. There were no cases of an allergic reaction.
The number of men and women among our patients turned out to be almost equal (19 and 18 people, respectively).
The oldest age group (90–99 years) is represented by a single patient - a 92-year-old woman, who, as a result of TLT, showed positive dynamics (restoration of facial expression and speech disorders).
The largest group (10 people) are patients aged 60–69 years, the number of men and women is the same. The results of TLT in each of the subgroups were the same: in 4 men and 4 women, complete or partial restoration of impaired functions was noted (positive dynamics); in 1 man and 1 woman there was no dynamics (no changes occurred); the TLT effectiveness rate in this group is the highest - 82%; No negative dynamics were observed among representatives of this group.
According to the effectiveness of the thrombolytic procedure, age groups can be ranked as follows:
60–69 years old - 82%;
20–49 years old - 80%;
50–59 years old - 75%;
70–79 years old - 43%;
80–89 years old - 33%.
(The group of 90–99 years old, consisting of 1 person, is not included in the rating.)
Cases of negative dynamics with a fatal outcome were noted in 2 groups (70–79 years old and 80–89 years old): a 79-year-old woman and an 84-year-old man. However, in both cases, according to the pathological and anatomical study, a direct connection between the death and the TLT procedure was not established. In the age group of 80–89 years, there was 1 case of hemorrhagic transformation (in an 88-year-old man).
The total number of women who experienced complete or partial recovery of impaired functions after TLT (14 people, 58%) exceeds the number of men with positive dynamics (10 people, 42%).
The overall effectiveness of TLT is quite high and amounts to 64.9% (24 people out of 37) against 8.1% (3 people) of cases of negative effect and 27% (10 people) of the absence of any effect of this procedure.
Thrombolytic therapy for ischemic stroke: predictors of safety and effectiveness
Systemic thrombolytic therapy with recombinant tissue plasminogen activator alteplase is currently the most optimal method of reperfusion for ischemic stroke. The article discusses the main predictors of the effectiveness and safety of this method of therapy, as well as the possibility of its use in patients with vertebrobasilar stroke.
Introduction
Ischemic stroke is a medical and social problem due to its widespread prevalence and severity of consequences (high incidence of mortality and disability). Systemic thrombolytic therapy (SLT) using recombinant tissue plasminogen activator (rt-PA) alteplase is the most effective and safe method of reperfusion for ischemic stroke in the first 4.5 hours from the onset of ischemic stroke [1, 2].
The TLT procedure became possible thanks to the introduction of computed tomography into clinical practice, which makes it possible to diagnose the nature of the stroke [3]. It should be noted that individual reports of the administration of fibrinolytics to patients, such as streptokinase and urokinase, only on the basis of the clinical picture of ischemic stroke were noted earlier [4, 5]. However, studies (MAST-I, MAST-E, AST), in which streptokinase was used for thrombolysis, were stopped early due to the high incidence of symptomatic hemorrhagic transformations [6–8].
Alteplase: pharmacokinetics, safety and efficacy study
Alteplase is rapidly cleared from circulating plasma: the rate of the process is 380–570 ml/min [9]. The pharmacokinetics of alteplase have been studied in healthy volunteers, as well as in patients with myocardial infarction [10]. The initial half-life has been shown to be less than five minutes (similar to natural plasminogen activator). Two open-label, dose-finding drug safety studies established the optimal dose of the drug for the treatment of ischemic stroke [11, 12].
The NINDS study was the first multicenter, randomized, placebo-controlled trial to demonstrate the safety and effectiveness of systemic TLT using rt-PA in the first three hours from the onset of the disease [13]. The following randomized placebo-controlled studies, ECASS I and II [14, 15], assessed the safety and effectiveness of different doses of rt-PA (ECASS I - 1.1 mg/kg, ECASS II - 0.9 mg/kg) in the first six hours from onset of stroke development. The safety results of the ECASS I and II studies were comparable to those of the NINDS study. In terms of effectiveness, no significant differences were found between the main group and the placebo group.
The two parts of the ATLANTIS study (A and B) assessed the safety and effectiveness of rt-PA at a dose of 0.9 mg/kg for up to five hours from the onset of disease. There was no significant positive effect of rt-PA compared to placebo [16].
The ECASS III trial [17] demonstrated the safety and effectiveness of systemic thrombolysis within the first 4.5 hours after symptom onset. The results of the work served as a reason to revise European and American recommendations for the treatment of ischemic stroke. It has been proposed to increase the therapeutic window for systemic TLT to 4.5 hours [1, 2]. In the Russian Federation, corresponding changes to the instructions for the drug alteplase were made on May 25, 2011.
The largest study, IST III [18], assessed the safety and effectiveness of systemic rt-PA TLT for ischemic stroke in the first six hours after its onset. The results of the work were considered neutral, since the primary end point was not achieved - the predominance of individuals with good recovery of impaired functions according to the Oxford scale in the TLT group.
Thus, at present, a positive evidence base for alteplase has been obtained only in two large studies - NINDS and ECASS III.
Factors influencing the effectiveness and safety of TLT
Possible options for the course of a stroke and its outcomes during reperfusion therapy are regression of neurological deficit with successful recanalization and reperfusion, the absence of any changes (due to the lack of recanalization and/or the development of irreversible damage to the brain substance in the lesion), as well as clinical deterioration. The latter is manifested by the development of complications, primarily hemorrhagic, reocclusion or re-embolism, or an increase in cerebral edema in case of insignificant effect of TLT.
The safety and clinical effectiveness (or lack thereof) of reperfusion therapy for ischemic stroke is influenced by:
- time of initiation of therapy;
- the presence and size of a brain region with potentially reversible changes;
- features of systemic and local hemodynamics;
- hemostasis factors;
- sensitivity of the brain substance to ischemia;
- degree of damage to the blood-brain barrier.
The dependence of the effectiveness and safety of fibrinolytic therapy on the time of its initiation has been demonstrated in a number of large studies. A pooled analysis of the results of the NINDS, ECASS I and II, ATLANTIS studies (n = 2775) showed that the odds ratio (OR) for a favorable outcome of the disease when thrombolysis was started in the first 90 minutes of stroke was 2.81 (95% confidence interval (CI) 1.75–4.5), from 90 to 180 minutes – 1.55 (95% CI 1.12–2.15). When starting TLT in the period from 181 to 270 minutes, the OR for a favorable outcome was already 1.40 (95% CI 1.05–1.85), after 271–360 minutes – 1.15 (95% CI 0.90–1. 47) [19]. Thus, time is the most important condition for the effectiveness of TLT [20]. That is why all recommendations for the treatment of patients with stroke emphasize the need to reduce all delays in starting therapy [1, 2].
In addition to the time factor, when performing TLT it is important to take into account the age of the patients. According to the instructions for use of the drug alteplase and the recommendations of the European Stroke Organization, patients under 18 years of age should not undergo TLT, and patients over 80 years of age –
with extreme caution [1].
While global experience with the use of rt-PA in children and adolescents with ischemic stroke is limited (there are only a few cases) [21], thrombolysis in patients in the older age group (over 80 years of age) is a routine practice both in the USA and in a number of European countries [ 22, 23]. Most researchers agree that TLT in people over 80 years of age is not associated with an increase in complications, such as hemorrhagic transformation of the brain lesion, and, therefore, does not lead to an increase in mortality [22]. It should be noted that in this age group there are higher rates of mortality and disability than among patients under 80 years of age, since age is an independent factor in increasing the risk of death due to stroke [24].
F. Mateen et al. analyzed data from the Canadian TLT registry for patients aged 80 to 89 years and from 90 to 99 years [23]. Both age groups were characterized by a predominance of females (61% in the group of 80–89 year olds and 77% in the group of 90–99 year olds) and initially severe stroke (more than 15 points on the National Institutes of Health stroke scale). of Health Stroke Scale), in 52 and 58%, respectively). Both groups had similar rates of symptomatic hemorrhagic transformation (4 and 7%, respectively), three-month mortality (33 and 52%, respectively), and a good degree of recovery of impaired neurological functions (26 and 30%, respectively). Thus, thrombolysis in patients both aged 80 to 89 years and 90 to 99 years old is equally safe and effective.
Despite the findings on the safety of TLT in people over 80 years of age, a Cochrane systematic review (26 randomized controlled trials, 7152 patients with stroke) noted a lack of convincing evidence to raise the upper age limit for fibrinolytic therapy [25]. The reason is the small number of patients over 80 years of age (approximately 1%) included in the meta-analysis.
A number of studies have focused on the safety and effectiveness of TLT in young stroke patients (under 45 years of age) [26, 27]. Their results are of particular interest due to the different correlation of risk factors and pathogenetic variants of ischemic stroke in this age group.
A subgroup analysis of data from the SITS-MOST registry showed that young patients after TLT have a more favorable outcome with a low incidence of symptomatic hemorrhagic transformation [26]. In a study by J. Putaala et al. a better degree of recovery of impaired neurological functions was also demonstrated in people under 45 years of age (40 versus 22% in the group of patients over 45 years of age). However, the incidence of hemorrhagic transformation between groups did not differ significantly [27]. Therefore, TLT is effective and safe in all age groups. However, the older the patients, the higher the number of functionally unfavorable outcomes and deaths.
Hemorrhagic transformation of the brain lesion during ischemic stroke is a serious complication, especially when performing TLT. M. Pessin et al., based on computed tomography data, proposed to introduce differences between hemorrhagic infarction and parenchymal hematomas [28].
Studies using computed tomography and magnetic resonance imaging have revealed that hemorrhagic transformation of the petechial hemorrhage type occurs in 15–45% of patients [29], and with the formation of a symptomatic parenchymal hematoma - in 5% [30].
The NINDS study clearly articulated the differences between types of hemorrhagic transformation. Hemorrhagic infarction is an area of hypodensity with hyperdense point inclusions with unclear contours within the ischemic zone. Parenchymal hematomas are typical homogeneous hyperdense formations with clear contours with or without mass effect [31].
The ECASS research group made its own amendments to the classification of hemorrhagic transformation. It has been proposed to distinguish between hemorrhagic infarction of the first and second types, as well as parenchymal hematomas of the first and second types [32]. Hemorrhagic infarction is defined as petechial permeation of the area of ischemic injury without a mass effect. In the first type, small petechiae are observed in the ischemic zone; in the second type, confluent petechial hemorrhages are observed. Parenchymal hematomas are defined as hemorrhages with mass effect. In the first type, hematomas account for 30% of the ischemic volume with a significant mass effect. Hemorrhages remote from the focus of ischemic damage (multifocal or single) are included in a separate group. In the NINDS study, this complication was observed in 1.3% of patients. In the ECASS I and II studies, in 23 (3.7%) of 620 and 16 (2.0%) of 800 patients, respectively.
Any factors leading to increased permeability of the blood-brain barrier can cause hemorrhagic transformation during TLT. T. Neumann-Haefelin et al. assessed the influence of the severity of leukoaraiosis on the development of hemorrhagic transformation in patients with ischemic stroke during TLT [33]. Symptomatic intracranial hemorrhages were significantly more common in patients with leukoaraiosis - 2 or 3 points on the Fazekas scale (12 (10.5%) of 114 patients) than in patients with minor leukoaraiosis - 13 (3.8%) of 335 (OR 2.9 (95% CI 1.29–6.59), p = 0.015). Logistic regression analysis showed that leukoaraiosis is an independent prognostic factor for the development of systemic hemorrhagic transformation as a result of TLT in patients with ischemic stroke.
Signs of early ischemia on a CT scan of the brain (hypodense changes in the brain substance, loss of contrast between gray and white matter in the convexital cortex, signs of swelling of the brain substance - smoothing of the sulci and compression of the cerebral ventricles) were also associated with an increased risk of developing symptomatic intracranial hemorrhages during TLT [34, 35].
The volume of hypodense changes in the brain substance is the main risk factor for the development of symptomatic intracranial hemorrhages. To assess it, it is recommended to use a scale for assessing early signs of computed tomography of cerebral ischemia (Alberta Stroke Program Early CT Score - ASPECTS) [36]. It was found that a low ASPECTS score (
Features of TLT in patients with ischemic stroke in the vertebrobasilar system
Carrying out TLT in patients with ischemic stroke in the vertebrobasilar system has its differences due to the structural features of the brainstem and cerebellum, as well as their blood supply [38–40]. Despite the large number of described cases of reperfusion therapy for vascular lesions of the vertebrobasilar system, mainly the basilar artery, not a single large randomized study has been conducted to evaluate the safety and effectiveness of this therapy depending on the affected area.
Currently, the question remains open about the tactics of reperfusion therapy for damage to the basilar artery (systemic thrombolysis or endovascular interventions). The largest prospective study comparing different reperfusion regimens for basilar artery disease is BASICS [41]. The study evaluated three treatment options in different combinations: antiplatelet and anticoagulant, systemic and intra-arterial, thromboembolectomy and stenting. The number of participants was 592. For 402 (67%) patients, a poor outcome was recorded: 4–5 points on the Modified Rankin Scale or death. In patients with mild to moderate symptoms treated with antiplatelet drugs and anticoagulants, the risk of adverse outcome was comparable to that of patients receiving systemic TLT and intra-arterial therapy. While in patients with severe stroke, the risk of an unfavorable outcome was lower when using reperfusion therapy than when taking antiplatelet drugs and anticoagulants. However, no significant differences in outcomes were obtained between different options of reperfusion therapy.
Since there were no significant differences in outcomes during systemic and selective TLT in patients with basilar artery occlusion, the question of the advisability of increasing the time from the onset of stroke to therapy remains relevant.
The most optimal option in this case seems to be combined reperfusion therapy. This approach would allow treatment to begin in a shorter period of time and take advantage of both reperfusion methods. Intravenous thrombolysis, as the fastest and technically simplest method, can be carried out at the first stage of therapy in clinics that do not have an x-ray surgery service, with subsequent transportation of the patient to a specialized center for endovascular intervention if there is no effect from the first intravenous administration of thrombolytic.
Considering the availability of studies demonstrating the feasibility and safety of such a scheme (drip, ship, retrieve) in patients with ischemic stroke [39, 42], and the possibility of conducting reperfusion therapy in patients with vertebrobasilar stroke in a wider therapeutic window, such multi-stage therapy could become preferable for patients with such pathology.
T. Pfefferkorn et al. analyzed various schemes for transporting patients for reperfusion therapy for basilar artery occlusion [43, 44]. One scheme involved transportation from a primary stroke center to a specialized one for the purpose of further selective TLT. The second - to a specialized center after systemic TLT with rt-PA at a dose of 0.9 mg/kg. In a specialized center, after emergency computed tomography angiography was performed in case of persistent occlusion of the main artery, mechanical thromboembolectomy was performed using MERCI Retriever, AngioJet and Penumbra devices. In the intra-arterial thrombolysis group, the rate of basilar artery recanalization was 92% (24 of 26), in the group of intravenous TLT and mechanical thromboembolectomy - 85% (22 of 26). Moreover, in 38% of cases, recanalization was achieved after intravenous administration of rt-PA; further mechanical thromboembolectomy was not required. And in the case of ineffective systemic TLT, the main artery was recanalized using mechanical thromboembolectomy. The effectiveness of different mechanical thromboembolectomy devices for basilar artery occlusion did not differ. It is important to emphasize that significant differences were obtained between the groups in the functional outcome by the third month from the onset of the disease: 4.7 points on the modified Rankin scale in the group of intra-arterial TLT and 3.4 points when using systemic TLT followed by mechanical thromboembolectomy.
The combination of intravenous thrombolysis and thromboembolectomy has been shown in small studies to be the most promising reperfusion therapy regimen for basilar artery occlusion. It is possible that the use of third-generation fibrinolytics (recombinant prourokinase, tenecteplase) with a long half-life in the “intravenous thrombolysis - thromboembolectomy” scheme will simplify the first stage of reperfusion therapy to a single bolus administration of the drug without the need for further infusion, which will reduce the time before the start of intervention.
Conclusion
Carrying out TLT taking into account the clinical and pathogenetic features of the disease, the localization of the lesion, data from additional research methods (primarily neuroimaging), and identifying predictors of hemorrhagic complications will contribute to a higher safety and effectiveness of this method of treatment for ischemic stroke.