Phenomenal Russian tennis player Maria Sharapova instantly made a drug called meldonium famous after failing a doping test. More than a hundred other international athletes have also been caught using this new banned substance. Now that the drug has gained worldwide fame, doctors fear that meldonium will be actively used by amateurs seeking to gain an advantage in competitions. "With the drug's new fame, a lot of people are going to try it," says Dr. Paul D. Thompson, chief of cardiology at Hartford Hospital in Connecticut. "We're learning a lot about the side effects of meldonium very quickly." This is why you should think twice about whether to take it or not.
Story
Meldonium, also known as mildronate, was discovered by a Soviet chemist in the 1970s. The drug is believed to have been developed for use as a human performance enhancer and anti-ischemic agent that helps with strokes and heart attacks.
In the 1980s, Mildronate was used with great success by athletes in the Soviet Union and other countries with doping programs. Since 1988, the drug has been added to the lists of prohibited substances of various sports organizations.
The benefits of mildronate for the human body
Mildronate increases the anaerobic threshold, which is the amount of time you can exercise at high intensity. This helps athletes maintain endurance during long and grueling training sessions or competitions. The World Anti-Doping Agency, or WADA, considers Mildronate a performance-enhancing drug because the drug increases the number of red blood cells in the blood and therefore makes it easier for athletes to transport oxygen in their blood.
Harm of mildronate to the human body
The problem is that very few studies have been published demonstrating its effectiveness or safety. Most studies have been done in rodents, and the one noteworthy human study was too small and too short to provide any definitive answers. Due to lack of evidence, meldonium is not approved by either the FDA or the European Union. It is mainly used in Russia, Ukraine and Eastern Europe, where it is sold without a prescription.
While many questions remain about the drug, it appears to have a clear mechanism of action that could help both heart and athletic performance. Meldonium appears to inhibit a substance in the body called l-carnitine, according to Karen Kopacek, an assistant professor at the University of Wisconsin-Madison School of Pharmacy. Normally, l-carnitine transports fatty acids into the mitochondria, where they are burned for energy. “But by blocking the availability of l-carnitine, meldonium causes mitochondria to metabolize glucose for energy, which requires less oxygen,” she explains. This reduces oxidative stress and cell damage while increasing the body's energy efficiency."
For these reasons, Kopacek says it's possible that meldonium improves athletic performance and reduces recovery time after exercise. But again, this is all taken from animal studies and other poor quality testing, so she insists there is no guarantee.
Whether it works or not, doctors know virtually nothing about its potential side effects. In the handful of published human studies, no side effects were reported. “I have doubts that the trial can go on for 12 weeks without the researchers noticing any side effects,” says Kopacek. “Does this mean that meldonium has no side effects?” Doubtful, she says, since almost every drug has some kind of side effect. With meldonium, we just don't know yet what the side effects might be.
It is also unknown how meldonium interacts with other drugs. The published study also lacks any information on this important issue. “Patients with heart disease—for whom this drug is intended—often take multiple medications, as well as over-the-counter medications, herbs and other supplements,” Kopacek says. You always have to know how drugs interact, and with meldonium we have no idea.” Another reason why I would never recommend this drug."
Given the FDA's strict protocol for evaluating and approving drugs for sale, it is unlikely that meldonium—a drug that has languished for decades without much interest from doctors or drug companies—will ever get the green light in the United States. “This would require randomized, double-blind, placebo-controlled studies, which cost money,” Thompson says. “The trials would have to be funded by the government, and the National Institutes of Health generally have no interest in helping athletes make more money.” But this does not stop the growing demand for the drug in Russia.
USE OF MELDONIUM AND ETHYLMETHYLHYDROXYPYRIDINE SUCCINATE IN THE ELDERLY
Population aging is a global problem of modern society. The number of people over the age of 60 is approximately 15% of the total population in European countries and 20% in Russia [1, 2]. The steady aging of the population leads to an increase in the number of elderly patients in the practice of doctors of many specialties. Prescribing medications to the elderly is possible after analyzing its effect on the body of an elderly patient, taking into account the increased sensitivity of elderly and old people to drugs (especially cardiac glycosides, antihypertensive drugs, tranquilizers, antidepressants).
The purpose of the work is to analyze drug prescriptions for elderly patients and compare them with treatment standards.
Material and research methods. The study was conducted on the basis of the State Budgetary Medical Institution "Republican Clinical Hospital of War Veterans". For the purposes of this study, elderly patients were considered to be citizens aged 60 years and older. The study used samples from the medical records of 96 patients treated in a geriatric hospital.
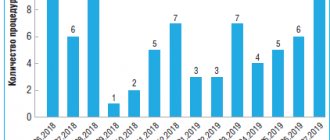
Results and discussion. The sample of prescriptions included the most frequently prescribed drugs: Meldonium under the trade name (TN) Mildronate and Ethylmethylhydroxypyridine succinate (TN Neurox).
Neurox was prescribed to 40 patients out of 96. The average age of the patients was 78.3±8.7 years. When studying the instructions for use of Neurox, it was established that the indications for its use are:
- acute cerebrovascular accident (as part of complex therapy);
- dyscirculatory encephalopathy (DEP);
- cardiopsychoneurosis;
- mild cognitive disorders of atherosclerotic origin;
- anxiety states in neurotic and neurosis-like conditions;
- withdrawal syndrome in alcoholism with a predominance of neurosis-like and vegetative-vascular disorders;
- acute intoxication with antipsychotic drugs.
When studying the main diagnoses of the elderly, it was found that in 43% of cases patients have hypertension, 32% of patients are diagnosed with angina pectoris, 2% each with ischemic heart disease and cardiomyopathy. For all these diagnoses, Neurox is indicated for use (Fig. 1).
Figure 1. Structure of main diagnoses, %
When studying concomitant pathology, it was revealed that 37.5% of patients had dyscirculatory encephalopathy (DEP), 12.5% each had hypertension and angina pectoris, 10% of patients had hepatitis or cirrhosis of the liver, which is an indication for the use of Neurox (Fig. 2 ).
Figure 2. Structure of concomitant diagnoses, %
The study showed that in 100% of cases Neurox is indicated for the treatment of the underlying or concomitant pathology. The instructions for the drug contain instructions for use in old age.
Next, we compared prescriptions with treatment standards. Neurox is recommended for use in only two standards for the treatment of diseases: Order of the Ministry of Health and Social Development of the Russian Federation dated October 9, 2006 No. 700 “Standard of medical care for patients with malignant neoplasms of the breast” and Order of the Ministry of Health and Social Development of the Russian Federation dated August 1, 2007 No. 513 “ Standard of medical care for patients with stroke." There were no patients with such diseases in our sample, and we can conclude that Neurox is not prescribed according to standards.
However, Neurox is included in the List of Vital and Essential Medicines, which explains its widespread use in hospitals.
Mildronate was prescribed to 31 patients out of 96, which is 32.3%.
The average age of patients prescribed Mildronate is 79.8.3±6.2 years.
Having studied the indications for use of Mildronate, it was found that it is indicated for:
- IHD (angina pectoris, myocardial infarction);
- chronic heart failure and dyshormonal cardiomyopathy;
- disorders of the blood supply to the brain (cerebral strokes and cerebrovascular insufficiency);
- hemophthalmos and retinal hemorrhages;
- reduced performance; physical stress;
- withdrawal syndrome in chronic alcoholism.
When studying the main diagnoses of patients receiving treatment with Mildronate, it was found that 24% of patients have coronary artery disease, 23% have hypertension, 3% have arrhythmia, 1% have hypercholesterolemia, 1% have pancreatitis (Fig. 3).
Figure 3. Structure of main diagnoses, %
When studying concomitant diagnoses, it was found that 10 patients had DEP, 6 had pyelonephritis, 4 had obesity, and only 1 patient had hypertension (Fig. 4).
Figure 4. Structure of concomitant diagnoses, %
The study showed that in 22.6% of cases there are no direct indications for the use of Mildronate in the treatment of the underlying or concomitant pathology. The instructions for the drug do NOT contain instructions on the possibility of use in old age. And Mildronate is not prescribed in any standard for the treatment of existing diseases. However, it is included in the List of Vital and Essential Drugs.
Thus, some of the most expensive drugs are Neurox and Mildronate, which belong to the list of vital and essential drugs but are not included in the standards for the treatment of major diseases of the elderly. This dictates the need for their inclusion in the formulary list of a medical organization.
BIBLIOGRAPHY
- Medical care and drug provision for elderly and senile people in the Republic of Tatarstan: Inform. Materials. Ministry of Health of the Republic of Tatarstan; Comp.: N.I. Galiullin, A.K. Rosenzweig, F.F. Yarkaeva, V.G. Sherputovsky. Kazan: Medicine, 2002. 24 p.
- Guide to gerontology and geriatrics: in volume IV. Edited by V.N. Yarygina, A.S. Melentyeva. M.: GEOTAR-Media. - 2007. - Vol. III Clinical Geriatrics. 896 pp.
- Soloninina A.V., Rostova N.B., Chereshneva N.D., Yakovlev I.B. Organization of drug care for elderly people // Advances in gerontology, 2013. T.26. — No. 1. p.183-189
- Suslina Z.A., Maksimova M.Yu., Kistenev B.A., Fedorova T.N. Neuroprotection in ischemic stroke: the effectiveness of Mildronate // Pharmateka. - 2005. - No. 13 (108).
- Chereshneva N.D., Soloninina A.V., Odegova T.F., Mazanov P.E. Analysis of the structure of diseases and prescriptions of medications for elderly people undergoing treatment in a hospital // Modern problems of science and education. - 2012. - No. 3.; UR: https://www. science-education.ru/103-6104
Let's sum it up
Mildronate has a variety of effects on the human body, especially in relation to cardiovascular health and increased endurance. However, as with many drugs, there are also several side effects. For example, mildronate can cause heart rhythm disturbances, severe skin rashes, and various allergic reactions. Additionally, since the drug is not readily available on the market in many countries, it cannot be easily tested for long-term side effects. The drug is currently legally available in Russia and several neighboring countries, but is banned in most Western countries because it can lead to positive doping tests.
After the World Anti-Doping Agency banned the use of meldonium on January 1, 2021, interest in this widely used and seemingly well-studied drug has increased. One of the important mechanisms providing the positive metabolic effects of meldonium is the ability of this drug to activate the choline and catecholaminergic neurotransmitter systems of both the brain and the peripheral nervous system [1]. The huge role of mediators of the autonomic nervous system (ANS) in the pathogenesis of almost all diseases determines the special interest of researchers in the possibilities of effective intervention in the course of the disease with the help of meldonium. Disturbances in the functioning of the ANS are an integral part of the pathogenesis of acute and chronic forms of coronary heart disease, all forms of cerebrovascular disease without exception, and largely determine the development of endothelial dysfunction, disorders of motility and secretion of all organs of the digestive system, and pathology of labor. The list goes on and on. The possibility of selective and universal correction of vegetative failures opens up incredible prospects in the treatment of diseases of the cardiovascular, nervous, and digestive systems, and significantly expands the possibilities of sports medicine. To date, a lot of clinical and laboratory studies have been carried out to analyze the direction of the neurometabolic effects of meldonium. The results of such an analysis could determine the advisability of using the drug for certain pathological conditions and even predict its effectiveness. Modern advances in neuropharmacology indicate that the breadth of mechanisms of action, combined with the power of a stimulating or inhibitory effect on a particular receptor system and/or metabolic reaction, directly determines the clinical effectiveness of the drug, while the selectivity of its effect in relation to certain types of receptors and/or or specific parts of metabolic processes is associated with increased safety of the therapy [2].
The cholinergic effects of meldonium described by most cardiologists are caused mainly by its ability to increase the concentration of γ-butyrobetaine (GBB) in the brain, which has the ability to induce the biosynthesis of nitric oxide (NO) due to its structural similarity to acetylcholine. An incredibly important feature of this induction is its exceptional selectivity - the effect occurs only within the ischemic zone, without affecting undamaged areas. This feature not only eliminates the risk of developing the “steal phenomenon” when using meldonium [3], but also allows one to interfere with the mechanisms of the ANS selectively and locally. None of the classical choline or adrenergic drugs has this ability, realizing their effects on the scale of the entire organism. Meldonium for the first time makes it possible to practically implement one of the leading concepts of modern clinical pharmacology - the theory of multiple selectivity.
Excessive adrenergic activity is an integral part of the pathogenesis of heart failure (HF). A direct correlation has been established between the increased content of norepinephrine in the blood plasma and the severity of heart failure. Moreover, the highest concentrations of norepinephrine were observed in severe untreated HF, which suggested its compensatory role aimed at maintaining blood pressure in progressive HF [4]. In chronic heart failure (CHF), there was an increase in the content of norepinephrine in the blood plasma and the concentration of free fatty acids (FFA), insulin and glucose, indicating the importance of adrenergic activation in the development of insulin resistance. Subsequent studies revealed that stimulation of β-adrenergic receptors increases the utilization and oxidation of glucose. Activation of protein kinase A and Ca2+-calmodulin-dependent kinase by the adrenergic receptor agonist adrenaline leads to a rapid increase in the activity of phosphofructokinase and protein kinase Akt. In addition, adrenaline also increases the uptake of calcium ions by mitochondria, activates pyruvate dehydrogenase and other enzymes of the tricarboxylic acid cycle. A prolonged increase in the content of catecholamines in the blood (often observed in patients with heart failure) counteracts the effects of insulin, promotes lipolysis and an increase in the level of circulating FFAs, and the development of insulin resistance. This action is mediated in part by negative feedback inhibition of insulin receptors [5]. The standard method of suppressing excess adrenergic activity in CHF is the use of β-blockers, which indirectly inhibit the oxidation of FFAs. Long-term therapy with β-blockers improves survival and left ventricular function. When taken, oxidative metabolism is significantly reduced and left ventricular function is improved, the processes of glucose utilization are enhanced, and the utilization of FFA by the heart is significantly reduced (by 57%).
However, to ensure the safety of CHF therapy using β-blockers, a number of conditions must be met: parallel use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, stable patient condition without the need for intravenous inotropic support and without signs of congestion, individual titration of the dosage of β-blockers, timely identifying and eliminating side effects. In addition, even selective β-blockers have a number of side effects [6].
In sports medicine, the possibilities of β-blockers are extremely limited, since the main mechanism of their action negates the adaptive mechanisms of the cardiovascular system to physical activity. Against this background, of particular interest is a metabolic drug that has the properties to regulate the function of the ANS.
Therapy with the inclusion of meldonium improves the autonomic regulation of cardiac activity by reducing sympathetic and increasing parasympathetic activity, accompanied by an increase in exercise tolerance [7, 8]. The positive effect of meldonium is determined not only by the blockade of β-oxidation of fatty acids and stimulation of glycolytic energy production, but also by the accumulation of endogenous GBB, choline-like metabolites of carnitine and its normalizing effect on the central parts of the neuroendocrine system. Due to the peculiarities of the biological action, meldonium can be used to normalize the activity of the sympathoadrenal system (SAS), increase the body’s nonspecific resistance and adapt to environmental factors, as well as to prolonged psycho-emotional stress [9].
Many researchers believe that meldonium has cholinergic activity due to its ability to block γ-butyrobetaine hydroxylase, causing GBB to undergo esterification. The structure of GBB ethyl ester is strikingly similar to that of acetylcholine (i.e., GBB ester is a potent m-acetylcholine receptor agonist). Acetylcholine interacts with the receptors of endothelial cells of blood vessels, which leads to the formation of NO radical molecules that migrate into the muscle layer and cause its relaxation. Thus, activation of acetylcholine receptors on the endothelium of blood vessels causes the induction of the biosynthesis of NO radicals. GBB esters bind to acetylcholine receptors; GBB esterase hydrolyzes receptor-bound esters similar to acetylcholinesterase. Hydrolysis of GBB esters triggers signal transduction involving second messengers. Nitric oxide turned out to be the most suitable candidate for the role of a second messenger for signal transduction after hydrolysis of GBB esters. The above results provide evidence that GBB esters are potent NO-dependent vasorelaxants and that GBB itself is a weak vasorelaxant, but is potentiated by meldonium [10].
In turn, GBB can induce the formation of NO, one of the most effective scavengers of free radicals in the body. Due to the increase in the concentration of GBB under the influence of meldonium, a very unexpected effect of the drug on peripheral resistance (which decreases), a decrease in spasms caused by norepinephrine or angiotensin, a slowdown in platelet aggregation and an improvement in the elasticity of erythrocyte membranes is explained. By increasing the amount of GBB, meldonium is able to protect cells from the effects of free radicals, but this is done through the induction of NO biosynthesis. Consequently, meldonium promotes the appearance of a physiologically regulated amount of NO, allowing the body to carry out the necessary level of protection against radicals [11].
A study of the possibility of correcting the adrenergic mechanism in the development of experimental cardiomyopathies and gastric damage with the help of meldonium revealed the inhibitory effect of the drug on the functional activity of the sympathetic nerve centers. This allowed us to conclude that it is advisable to use meldonium to correct disturbances in the functional activity of stress-releasing and stress-limiting systems in diseases in the pathogenesis of which stress and toxic influences play a role [12]. An experimental study of the effect of meldonium on the functional activity of the SAS and nonspecific resistance of the body under conditions of emotional pain stress on intact animals also confirmed the corrective and protective properties of the drug due to the accumulation of endogenous GBB, choline-like metabolites of carnitine and its normalizing effect on the central parts of the neuroendocrine system. Thus, the possibility of using meldonium to normalize the activity of the SAS, increase the body’s nonspecific resistance and adapt to environmental factors, as well as to prolonged psycho-emotional stress, has been proven [13].
At the same time, a number of researchers have identified adrenosensitizing properties in meldonium. In experiments with smooth muscle objects, it was shown that meldonium increases the ability of adrenaline to have a relaxing effect, realized through the activation of β2-adrenergic receptors [14]. The direction of the sensitizing effect is confirmed by the presence of this effect in cases with the smooth muscles of those organs where β2-adrenergic receptors are present (trachea, myometrium, coronary arteries) and the lack of effect in experiments with the myocardium on β1-adrenergic receptors. Taking into account the data on the presence in the human and animal body of an endogenous direct-acting adrenergic receptor sensitizer, the most likely components of which are histidine, tryptophan and tyrosine, the results of the study made it possible to consider meldonium as an exogenous direct-acting β-adrenosensitizer. The basis of the β-sensitizing effect of meldonium is its ability to increase the effectiveness of the interaction of adrenaline and norepinephrine with β-adrenergic receptors. This ability is realized through one of three possible processes: 1) an allosteric change in the conformational state of β-adrenergic receptors, as a result of which the affinity of the receptor for the agonist increases; 2) inhibition of the activity of a number of enzymes involved in the phosphorylation of β-adrenergic receptors (β-adrenergic receptor kinase, protein kinase α- and β-arrestin), due to which the receptors lose their affinity for the agonist; 3) by increasing the activity of phosphatase, which is involved in the dephosphorylation of β-adrenergic receptors and thereby restoring their affinity for the agonist. First, the β-adrenosensitizing effect of meldonium was proven in experimental studies on animals [15–17], then in laboratory studies of pregnant women, when the method of adrenodependent osmotic resistance of erythrocytes showed that meldonium increased the efficiency of activation of β-adrenergic receptors of erythrocytes by adrenaline or hexoprenaline [18 , 19]. In obstetric practice, this drug has already found use in the treatment of labor anomalies and placental insufficiency. The use of meldonium in practice as an exogenous β-adrenosensitizer made it possible to enhance the effect of β-adrenergic agonists and thereby reduce the dose of hexoprenaline by half (when stimulating labor) and ultimately reduce the number of side effects [20].
A study of the possibility of correcting the β-blocking effect of ozone revealed this possibility in meldonium (along with histidine, tryptophan, tyrosine and trimetazidine). This effect was explained as a result of restoration of the affinity of β-adrenergic receptors for agonists (due to activation of phosphatase, which dephosphorylates β-adrenergic receptors). The results of the study made it possible to regard meldonium as an exogenous selective β-adrenosensitizer [21].
The effectiveness of meldonium in the treatment of CHF is largely explained by the autonomic effects of the drug. According to the working hypothesis of I.Ya. Kalvins, the acetylcholine-like effect of meldonium on blood vessels is associated with an increase in the concentration of GBB in them due to inhibition of the enzymatic conversion of the latter into carnitine. The blockade of carnitine synthesis determines the classic cytoprotective effect of the drug, which consists in blocking the transport of FFA into the mitochondria. Due to the peculiarities of its molecular structure, GBB is capable of activating muscarinic receptors that mediate the formation of NO [22]. The stimulating effect on acetylcholine receptors, which the drug has under conditions of ischemia, causes the induction of endothelial NO synthase, due to which the synthesis of NO increases and the content of intracellular calcium decreases. This leads to relaxation of smooth muscle cells of microvasculature and muscular arteries, causing mild receptor-induced vasodilation, which is extremely important in conditions of tissue ischemia in patients with pathology of the cardiovascular system. The use of meldonium in addition to basic therapy, incl. persons with coronary bypass surgery and endovascular interventions on the coronary arteries, contributed to a decrease in intramyocardial tension, normalization of the state of endothelial and humoral regulation, a decrease in the content of lipid peroxidation and an increase in the activity of antioxidant systems [23].
In a study of the effect of meldonium on the central and autonomic nervous systems of students with attention deficit disorder, it was found that taking the drug in a dose of 250 mg increases the lability of the central nervous system, the level of concentration, mental performance, the ability to develop differential inhibition and, in general, to form labor dominant. At the same time, meldonium did not significantly affect the state of the ANS and cardiovascular system.
This effect of the drug is based on two mechanisms. The first is that meldonium, as an exogenous sensitizer of β- and α-adrenergic receptors, increases the efficiency of activation of the corresponding receptors of brain neurons, which is carried out with the participation of noradrenergic neurons of the monoaminergic system. The second mechanism is that meldonium, acting as a sensitizer of α-adrenergic receptors of cerebral vessels, promotes the redistribution of blood flow in the cerebral cortex to working neurons and thereby contributes to the formation and maintenance of a dominant focus in the cerebral cortex [24].
A study of the effect of meldonium on the state of autonomic regulation of the cardiovascular system (according to cardiointervalography) in children and adolescents with vegetative dystonia syndrome showed its ability, when taken as a course, to normalize the state of the ANS in hypersympathicotonia in 50.8%, and in parasympathicotonia in 23.1% cases. This universal ability to correct multidirectional disturbances in ANS reactivity is explained by the complex of cholinergic, adrenosensitizing, vasodilating and cytoprotective effects of the drug [25]. A similar normalizing effect of meldonium on autonomic disorders was also detected in alcohol withdrawal syndrome [26].
The advantages of the cardiocytoprotective effect of meldonium in the correction of adrenergic pathological influences were noted in a number of other clinical cardioneurological studies [27, 28], as well as in chronic cerebral ischemia [29], in patients with discirculatory encephalopathy of atherosclerotic origin [30]. Meldonium has also found its niche in the correction of autonomic disorders in various types and stages of diabetic neuropathy [31]. The special role of meldonium should be noted in the treatment of autonomic cardiac vegetoneuropathy, characterized by hypersympathicotonic disorders already in the initial phase of its development [32]. The predominant effectiveness of the drug in the correction of adrenergic disorders has been shown in numerous patients with diabetes mellitus [33].
Analysis of the results of the above studies allows us to arrange the mechanisms of meldonium’s effect on the ANS into the following groups:
1. Cholinergic effect resulting from the ability to accumulate the acetylcholine agonist GBB mainly in areas of hypoxia and ischemia. This opens up great opportunities for correcting the pathogenesis of a number of diseases and pathological conditions. Firstly, it is an opportunity to balance pathological adrenergic influences in coronary heart disease, arterial hypertension, CHF and hypersympathicotonia of any origin. Secondly, this effect will compensate for the weakening of parasympathetic influences that occurs in many neuropathies and other neurological diseases. Such intervention in the mechanisms of diseases involving the conduction system of the heart seems especially valuable. There are many diseases whose treatment requires strengthening of neuromuscular transmission. Strengthening cholinergic effects allows you to increase the tone and contractility of skeletal muscles and myocardium; strengthen the tone and motility of the smooth muscle muscles of the intestines, bladder, gallbladder, bronchi; increase the secretion of exocrine glands. The choice of cholinomimetic agents used for these purposes is quite limited. But the main limitation on the possibilities of their effective use is the lack of selective influences. The ability of meldonium to concentrate a choline-like metabolite in organs suffering from hypoxia opens up completely new possibilities in the treatment of cardiac, neurological, urological, gastroenterological and pulmonological diseases. The opportunity to stimulate secretion and gastric motility in atrophic gastritis, without interfering with the regulation of other organs and systems, seems very attractive. As well as the ability to eliminate tachycardia in case of autonomic cardiac vegetoneuropathy without resorting to β-blockers with their side effects. The list of examples can be very long.
2. Alpha- and β2-adrenosensitizing effect provided by the ability of meldonium metabolites to activate phosphatase, which dephosphorylates β2-adrenergic receptors. The ability to selectively stimulate the adrenergic system of the trachea, uterus, and coronary arteries (localization of β2-adrenergic receptors) without affecting the myocardium (β1-adrenergic receptors) also seems very valuable in a number of pathological conditions. The prospects for using sensitizers in clinical practice have already been established [18]. For example, in cardiology as substances that restore the efficiency of β-adrenergic receptor activation, which is important for CHF [34], as well as in obstetrics for women with the threat of premature birth, because at the same time, the efficiency of activation of β-adrenergic receptors decreases. This possibility for meldonium has already been realized in practice in the treatment of labor, and the drug has already shown its effectiveness in the treatment of CHF [35]. The autonomic effects of meldonium have been successfully implemented in the clinic to stabilize heart rate in patients with ischemic stroke [36, 37], to correct asthenic conditions in patients with arterial hypertension [38] and to restore normal ANS reactivity in comorbid pathology [39].
The α-adrenosensitizing effect of meldonium has been studied to a lesser extent. Its presumable presence explains the improvement in cognitive functions while taking the drug. However, this effect currently raises a number of questions. As is known, stimulation of α-adrenergic receptors leads to contraction of smooth muscles of blood vessels, bronchi, bladder sphincter and relaxation of intestinal smooth muscles. In addition, selective stimulation of α1-adrenergic receptors (leading to typical α-adrenergic effects, including vasoconstriction) or α2-adrenergic receptors (leading to presynaptic inhibition of the release of norepinephrine from sympathetic endings, as well as many other reactions - inhibition) is possible release of acetylcholine from cholinergic endings, suppression of lipolysis in lipocytes, inhibition of insulin secretion, stimulation of platelet aggregation and vasoconstriction of some organs). Theoretically, one can assume different selective concentrations of meldonium or its metabolites in different organs. Although the presence of simultaneous α- and β-adrenosensitizing effects of equal severity in each individual organ (for example, in the uterus) seems doubtful, the extreme complexity and insufficient knowledge of the effects on different types of adrenergic receptors should be taken into account. Literature data suggest that activation of all three major β-adrenergic receptor subtypes promotes vasodilation, which may be partially mediated by endothelial vasodilatory factors, primarily NO. However, the role of each of these subtypes and the contribution of the endothelium to the mechanisms of action due to their activation differ significantly in different areas of the vascular bed. Moreover, the contribution of endothelial NO to the mechanism of vasodilation caused by β-adrenergic antagonists may vary within the same organ depending on the diameter of the vessels [40].
It has already been established that stimulation of cardiac adrenergic receptors with adrenaline while taking adrenergic blockers gives a negative inotropic effect, and not a positive one, as usual, which leads to a decrease in the pumping function of the heart. This effect is stopped by exogenous β-adrenergic receptor sensitizers (including meldonium), which increase the efficiency of activation of β1- and β2-adrenergic receptors. In humans, α2-adrenergic receptors of the myocardium may be involved in the manifestation of the negative inotropic effect of catecholamines against the background of blockade of β2- and/or β1-adrenergic receptors, because their activation reduces the force of heart contractions (by blocking the release of norepinephrine from the terminals of the sympathetic nerves). This means that reversing the negative inotropic effect of catecholamines in patients taking β1- and β2-adrenergic receptor antagonists may be effective with the use of a selective α2-adrenergic receptor antagonist [41].
The question of the relationship between the cholinergic and adrenosensitizing properties of meldonium has not yet been studied in detail. The combination of these effects explains the universal “stabilizing” effect of the drug on undifferentiated or multidirectional ANS disorders. Against the background of the main metabolic effects of the drug, such a universal normalizing effect on vegetation greatly expands its use, which is observed in practice. Practicing physicians of all specialties are increasingly including meldonium in complex therapy based on the versatility of its action [42], especially often in comorbid pathology [43]. Such an indiscriminate approach does not have a sufficient evidence base and can lead to a decrease in the effectiveness of both monotherapy and complex treatment. And if the place of meldonium in the series of metabolic cytoprotective agents has already been quite clearly defined [44, 45], then this cannot yet be stated regarding its position in the group of vegetative-stabilizing drugs. Numerous studies indicating the relationship between disorders of autonomic regulation and the immune response in the pathogenesis of diseases such as bronchial asthma, obesity [46], gastroduodenitis, eczema, urological and ENT pathology, justify the use of vegetative drugs [47] and open up tempting prospects for the effective use of autonomic the effects of meldonium in the treatment of these diseases. Further study of the autonomic effects of meldonium would make it possible to develop differentiated indications for its use as a corrector of autonomic disorders, which would ensure high and stable effectiveness of the therapy.