Types and causes of thrombocytosis
Thrombocytosis is of two types:
- Primary thrombocytosis, in which the number of megakaryocytes in the bone marrow increases. This, in turn, leads to an increase in the number of platelets with a normal life expectancy, but impaired functions and abnormal structure. These platelets tend to be large, increasing the tendency for them to bleed and form clots that can block blood vessels. Bleeding occurs because platelet aggregation is disrupted and because most of them can be used to form blood clots. This condition can provoke serious complications: myocardial infarction, stroke, gastrointestinal bleeding. At the moment, the reasons why the division of megakaryocytes in the bone marrow is disrupted are unknown, but scientists have information that patients have a mutation in the V617F gene. Primary thrombocytosis is a myeloproliferative disorder. In such diseases, the hematopoietic function of the bone marrow is disrupted, which stimulates the formation of blood cells.
- Secondary (or reactive) thrombocytosis, in which platelets function normally, but the disease itself is formed due to one of the following abnormalities:
With secondary thrombocytosis, the likelihood of bleeding and clots is usually lower than with primary thrombocytosis.- Oncological diseases (most often ovarian, lung, stomach cancer);
Response to irritation of the bone marrow by certain substances that damaged tissues release during: fractures of large bones; infectious diseases (usually bacterial, less often viral, fungal and parasitic); serious and large-scale surgical operations: Removal of the spleen (splenectomy);
- Chronic or acute bleeding;
- Chronic inflammation;
- Taking certain medications: chemotherapy drugs and glucocorticosteroids;
- Recovery from thrombocytopenia (which was caused by alcohol or vitamin B12 deficiency).
Thrombocytosis
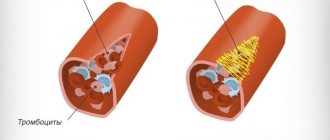
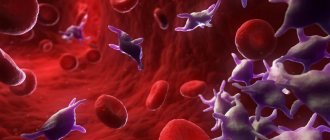
Thrombocytosis is a significant increase in the number of platelets in the blood, which disrupts the properties of the blood and increases the likelihood of thrombosis (blockage) of blood vessels. Platelets are cells that are responsible for blood clotting.
Thrombocytosis can be either an independent disease or a consequence of a number of diseases of the blood or any organs.
Primary thrombocythemia occurs most often in people over 60 years of age. The prognosis is favorable - the life expectancy of patients with primary thrombocytosis with proper observation and treatment is practically no different from that of healthy people.
Young children are more susceptible to secondary thrombocytosis. The platelet count usually returns to normal after recovery from the underlying illness.
Synonyms Russian
Essential thrombocythemia, primary thrombocythemia, secondary thrombocythemia, thrombocytophilia, chronic thrombocythemia, chronic megakaryocytic leukemia, idiopathic thrombocythemia.
English synonyms
Primary thrombocythemia, essential thrombocythemia, idiopathic thrombocythemia, primary thrombocytosis, essential thrombocytosis, secondary thrombocytosis, reactive thrombocytosis, secondary thrombocythemia.
Symptoms
Symptoms usually develop gradually and may be absent in the initial stages of the disease. The main manifestations of thrombocytosis are caused by two factors: the formation of blood clots in blood vessels and increased bleeding. With secondary thrombocythemia, the likelihood of these disorders is lower, since the number of platelets is lower than with primary thrombocythemia.
The main symptoms of thrombocytosis:
- headache,
- pain in the hands and feet, their numbness,
- weakness, irritability,
- visual impairment,
- bleeding gums,
- nosebleeds,
- blood in the stool.
General information about the disease
Platelets are small, colorless plates that do not contain a nucleus. They are formed in the bone marrow and are “fragments” of megakaryocytes - giant multinucleated cells. From the bone marrow, platelets enter the blood, and some of them are retained in the spleen. They exist for about 7-10 days and are then destroyed by liver and spleen cells. Platelets are responsible for blood clotting and stopping bleeding. Their normal amount in the blood is 150-450×109/l.
There are two types of thrombocytosis.
1. Primary thrombocytosis. In this case, an increased number of megakaryocytes is formed in the bone marrow, which increases the number of platelets that have a normal life expectancy, but an abnormal structure and impaired functions. Platelets are large, and there is an increased tendency to form clots that block blood vessels and cause bleeding. Bleeding occurs due to disruption of platelet adhesion, and also due to the fact that most of them can be used to form blood clots. This can lead to serious complications: stroke, myocardial infarction, gastrointestinal bleeding. The causes of impaired division of megakaryocytes in the bone marrow are not fully known, however, there is information about the presence of a mutation in the V617F gene in patients. Primary thrombocytosis refers to myeloproliferative diseases in which the hematopoietic function of the bone marrow is disrupted, which stimulates the formation of blood cells.
2. Secondary (reactive) thrombocytosis. With it, platelets function normally, and the cause of the disease itself is some other abnormality, one of the following.
- Oncological diseases, most often cancer of the stomach, lungs, ovaries. Tumor cells secrete biologically active substances that activate platelet production.
- Response to irritation of the bone marrow by substances that are released by damaged tissues during: infectious diseases, most often bacterial, less often parasitic, fungal and viral,
- fractures of large bones (femur, humerus, pelvic bones),
- extensive surgical operations.
Such thrombocytosis always does not last long and disappears when the patient’s condition normalizes.
- Splenectomy – removal of the spleen. In this case, thrombocytosis is associated with the entry into the blood of those platelets that are normally found in the spleen, as well as with a decrease in the amount of substances synthesized by the spleen and inhibiting the formation of platelets in the bone marrow.
- Acute or chronic bleeding. Acute occurs suddenly and is caused by trauma, surgery, chronic lasts a long time and can accompany a stomach or duodenal ulcer, or intestinal cancer. As a result of blood loss, iron deficiency anemia occurs, that is, a decrease in the amount of hemoglobin, red blood cells and iron included in their composition. The mechanism of development of thrombocytosis in response to iron deficiency has not been fully studied. Another factor is important in this case: during blood loss, the production of red blood cells in the bone marrow is activated. The process of more active division also involves megakaryocytes, that is, the number of platelets in the blood increases. In addition, thrombocytosis is a natural response of the body, which needs additional platelets to stop bleeding.
- Chronic inflammation (colitis - inflammation of the large intestine, vasculitis - inflammation of the walls of blood vessels, rheumatoid arthritis - inflammatory disease with joint damage), in which interleukin-6 is released - an active substance that stimulates the formation of thrombopoietin, which promotes the division of megakaryocytes and the formation of platelets.
- Taking medications: glucocorticosteroids (synthetic analogs of adrenal hormones), chemotherapy drugs (vincristine).
- Recovery from thrombocytopenia caused by vitamin B12 deficiency and alcohol. Thrombocytosis in this case occurs as a response to thrombocytopenia therapy.
The likelihood of clots and bleeding with secondary thrombocytosis is lower than with primary thrombocytosis.
Who is at risk?
- People over 60 years of age (for primary thrombocytosis).
- Children (for secondary thrombocytosis).
- Patients with iron deficiency anemia.
- Having undergone surgery, severe injuries.
- Suffering from cancer.
Diagnostics
Thrombocytosis is often asymptomatic. A doctor may suspect it during a routine checkup. An important point in diagnosis is to determine the type of thrombocytosis - primary or secondary. In the case of secondary thrombocytosis, the doctor may prescribe a number of additional studies necessary to determine its cause.
Laboratory diagnostics
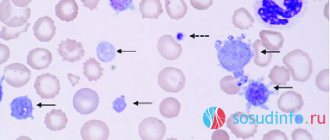
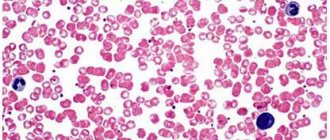
- Complete blood count with leukocyte formula. With thrombocytosis, the platelet level is elevated. In primary thrombocytosis, it can even exceed one million per microliter (1000×109/l), which is not typical for secondary thrombocytosis. In addition, with primary thrombocytosis, the number of other blood elements is sometimes increased: leukocytes, lymphocytes, erythrocytes. In secondary thrombocytosis, blood characteristics depend on the underlying disease, for example, during infection, the level of leukocytes may be increased. In primary thrombocytosis, large, irregularly shaped platelets are detected in the blood smear; fragments of megakaryocytes, as well as single immature leukocytes, can occasionally be found; in secondary thrombocytosis, platelets are usually not changed.
- ESR – erythrocyte sedimentation rate. May be elevated due to inflammation that causes reactive thrombocytosis.
- Ferritin is an iron-binding protein. Its level indicates the amount of iron in the body. With secondary thrombocytosis caused by iron deficiency anemia, it is reduced.
- Molecular genetic studies - identification of possible genetic disorders. With primary thrombocytosis, the structure of the gene (DNA section) JAK2V617F may be disrupted.
Additional Research
- Bone marrow biopsy is the removal of a sample of bone marrow from the breastbone or pelvis using a fine needle. It is carried out after preliminary anesthesia. In primary thrombocytosis, an increased number of megakaryocytes may be found in the bone marrow. A bone marrow biopsy is also necessary to exclude malignant blood diseases, the first sign of which may be thrombocytosis.
- Ultrasound of the abdominal organs to identify possible internal bleeding.
Treatment
Treatment of primary thrombocytosis depends on the risk of complications - thrombosis and bleeding. This is determined by age, the presence of concomitant diseases (for example, diabetes, cardiovascular diseases), and platelet levels. If the likelihood of complications is high, then use:
- drugs that suppress the production of cells in the bone marrow,
- aspirin - it thins the blood, which reduces the likelihood of blood clots,
- therapeutic thrombopheresis - in this case, using a special device, the patient’s blood is filtered to remove excess platelets.
Treatment of secondary thrombocytosis is determined by its immediate cause. As a rule, when the patient recovers from the underlying disease, the platelet level returns to normal. In addition, long-term secondary thrombocytosis can develop after splenectomy, then the patient is prescribed small doses of aspirin or drugs containing it to prevent complications.
Prevention
There is no prevention for primary thrombocytosis.
Prevention of secondary thrombocytosis consists of preventive examinations and timely identification of diseases that can lead to a secondary increase in the number of platelets.
Recommended tests
- General blood analysis
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- Coagulogram No. 1 (prothrombin (according to Quick), INR)
- Ferritin
- Cytological examination of punctates, scrapings of other organs and tissues
Symptoms of thrombocytosis
Typically, symptoms develop gradually. At the initial stages of the disease they may be completely absent. The main manifestations of thrombocytosis are provoked by two factors: increased bleeding or the occurrence of blood clots in the blood vessels. If thrombocythemia is secondary, then the likelihood of such disorders occurring is much lower: the number of platelets in this form of the disease is lower than in the primary one.
The main symptoms of thrombocytosis include:
- pain in the feet and hands, their numbness;
- headache;
- irritability and weakness;
- bleeding gums;
- visual impairment;
- blood in stool;
- nosebleeds.
Diet
Diet for essential thrombocythemia
- Efficacy: therapeutic effect after 3 weeks
- Timing: constantly
- Cost of products: 1400-1500 rubles per week
Nutrition is an auxiliary factor in this condition. Taking into account the tendency to blood clots, your diet should include foods that help thin the blood: figs, beets, lemon, prunes, garlic, raspberries, cranberries, strawberries, artichokes, oranges, olive oil, raisins, blueberries, as well as spices and herbs (chili pepper, thyme, paprika, turmeric, oregano, curry, mint, cinnamon).
The diet needs to be balanced according to the main nutrients and vitamins and microelements must be introduced. Iodine, which is rich in seaweed and seafood, iron contained in red meat and liver, magnesium in cereals, bran bread, vegetables, honey, fruits, as well as calcium, are useful.
A varied diet containing sea fish, squid, shrimp, seaweed, vegetable oils, chicken and beef liver, oatmeal, dairy products, eggs, nuts (cashews and almonds), fresh vegetables and fruits will maintain metabolic processes at a normal level.
It is important to adhere to the drinking regime - drinking fluid within 2-2.5 liters per day. This improves its fluidity. If there is no indication for taking diuretics due to the underlying disease, they should be abandoned since this group of drugs helps to thicken the blood. The same applies to diuretic herbs and laxatives that are taken uncontrolled.
In addition, there are foods that contribute to blood thickening that should be avoided. This is sugar, white bread, bananas, mangoes, potatoes, buckwheat and semolina, fatty meats, any smoked meats, rosehip infusions, alcohol, legumes, walnuts, sorrel, lettuce, chokeberry.
Forecast
In most cases, the course of essential thrombocythemia is indolent (sluggish), with long intervals without any manifestations, which is periodically interrupted by thrombosis or hemorrhagic manifestations. With this course, the life expectancy for essential thrombocythemia is 10-15 years. The main cause of disability and decreased life expectancy is the occurrence of thrombosis and thromboembolism . The duration of the disease increases the risk of these complications. Only in some patients, with a long course of the disease, can an outcome occur in secondary bone marrow fibrosis, which was mentioned above, or the transition to acute myeloid leukemia.
With the development of blast transformation, the prognosis is unfavorable and survival is estimated at several months. In patients with normal general status, chemotherapy is attempted according to the protocols for the treatment of acute leukemia . However, it brings an effect only in some patients and this effect is temporary. When the effect of chemotherapy is achieved, allo-bone marrow transplantation is sometimes performed to increase life expectancy.
List of sources
- Moroz G.I. Reactive thrombocytosis in children / Health of Ukraine. — 2015, No. 3, p. 63.
- Gluzman D.F., Sklyarenko L.M., Nadgornaya V.A., Ivanovskaya T.S. Modern laboratory diagnosis of myeloproliferative neoplasms / Health of Ukraine 2011 No. 1-2 p.30-31.
- Clinical hematology: a guide for doctors / ed. A.N. Bogdanov and V.I. Mazurova. – St. Petersburg: Foliant Publishing House LLC. – 2008. – 488 p.
- Abdulkadyrov K.M., Martynkevich I.S., Shuvaev V.A. Modern approaches to the diagnosis and treatment of essential thrombocythemia: a review of the literature and our own data/Clinical oncohematology. Basic research and clinical practice.—2015, pp. 235-246.
- Bogdanov A.N., Tyrenko V.V., Noskov Y.A., Semelev V.N. /Differential diagnosis of thrombocytosis in clinical practice/Bulletin of the Russian Military Medical Academy - 2014.-2(46), pp. 44-49.
Consequences and complications
The most common complications are:
- Thrombosis and thromboembolism . Increased platelet aggregation significantly increases the risk of venous and arterial thrombosis and cerebral ischemia . In malignant tumors, the number of venous thromboses increases significantly when compared with other types of secondary thrombocytosis. In essential thrombocythemia, thrombosis is the second cause of mortality (in first place is transformation into acute leukemia). It is noted that in 60-70% of cases these are arterial thromboses . Patients develop myocardial and cerebral infarction and peripheral occlusions. In the case of venous thrombosis, the veins of the lungs, extremities and abdominal cavity are involved.
- Blast transformation. Prolonged growth of the tumor clone causes additional mutations and a higher degree of malignancy. The consequence of this is blast transformation and the development of blast crisis, which is regarded as the terminal stage of the disease. Progression to blast transformation occurs in 1-2% of patients within 10 years of the disease; with a longer course (20 years), this percentage increases and is already 5-8. The diagnostic criterion for blast crisis is the appearance of more than 20% blast cells in the blood or bone marrow. Risk factors are: a decrease in hemoglobin less than 110 g/l and thrombocytosis more than 1000 x 10 in 9/l. It is believed that the development of a blast crisis can be provoked by cytoreductive therapy, in particular the chemotherapy drugs busulfan and hydroxycarbamide . The duration of treatment with them does not have a significant effect on this process.
- Development of postthrombocythaemic myelofibrosis . The transition to postthrombocythaemic myelofibrosis is observed in 4-10% of patients in the first 10 years, and with a disease duration of more than 10 years - in 30%. Erythroblasts, young neutrophil granulocytes are found in the blood, the liver and spleen are enlarged, and tumor intoxication appears (fever, weight loss, night sweats). Changes in the bone marrow in the form of fibrosis significantly worsen hematopoiesis and cause the development of cytopenias (inhibition of all hematopoietic germs. Therefore, with the development of myelofibrosis, symptoms appear: bleeding due to thrombocytopenia (decreased platelet levels), anemia associated with inhibition of the erythrocyte germ and various infectious complications due to leukopenia Spontaneous bleeding from dilated veins of the esophagus is life-threatening.Due to the enlargement of the liver and spleen, the pressure in the portal vein increases and portal hypertension develops.