Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001. January, 2021.
Synonyms: platelets, platelet count, PC, plt.
Platelets are blood cells, and their concentration is determined during a general blood test. On the CBC form, platelets are designated as platelet count or PC. Blood for studying its composition, including counting the number of platelets, is taken from a finger (capillary) or from a vein. The unit of measurement for platelets is the number (N) of cells multiplied by 109 per liter.
Platelets, like other formed elements, are formed in the red bone marrow. Their lifespan in the bloodstream is about 7–12 days. Destruction and breakdown of cells occurs in the spleen and liver tissues.
The main function of platelets is to carry out hemostasis, that is, to stop bleeding. Contact with damaged tissues causes transformation of cells, up to 10 processes are formed in them, and when they spread, the wound is closed with a platelet mass (thrombus). Thus, platelets prevent large amounts of blood from leaking out of damaged soft tissues.
Another equally important function of platelets is to protect the injured area from the penetration of pathogenic microorganisms (they secrete lysozyme and B-lysine).
Platelets also participate in the processes of hemostasis (maintaining the internal environment of the body), nutrition of the capillary endothelium (the inner layer of the walls of blood vessels) and regenerative processes of damaged tissues due to the release of growth factors that stimulate cell division.
A 2021 scientific paper provides evidence showing that in addition to the above functions, platelets also play an important role in the human immune system.
Indications
Prescription of an OAC with a study of platelet concentration is indicated for all patients who visit the clinic, undergo a routine medical examination, or receive a referral for inpatient treatment. Also, platelet determination is prescribed to all patients requiring surgery (emergency or planned). The main indications for platelet testing include:
- suspicion of disturbances in the hemostatic system (bleeding, formation of subcutaneous hematomas);
- suspicion of a malignant process;
- immunity disorders;
- bronchopulmonary pathology;
- diseases of the digestive tract and urinary system (stomach ulcer, glomerulonephritis);
- cardiovascular pathology;
- endocrine disorders (obesity, diabetes).
Symptoms that should alert you
- red, purple bruises on the skin
- frequent nosebleeds, bleeding gums
- prolonged bleeding of even small wounds or cuts
- heavy menstrual bleeding in women
Increase P-LCR
An increased number of large platelets means that there is a pathology in the body. Only in isolated cases is a high P-LCR value an individual characteristic of a person and does not require treatment.
Etiology
The reasons for an increase in P-LCR can be completely different diseases - inflammatory, oncological, hematological, infectious.
But most often, the formation of a large number of large platelets occurs in autoimmune disorders. Systemic diseases that can cause thrombocytosis include: collagenosis (scleroderma, systemic lupus erythematosus, rheumatic diseases, periarteritis nodosa), sarcoidosis, polyarthritis, ankylosing spondylitis, enteropathy. These processes are accompanied by the release of interleukin and other inflammatory mediators into the blood, which stimulate the biosynthesis of thrombopoietin and the formation of a large number of platelets.
Along with this, the P-LCR index increases if the patient has:
- infectious pathology - bacterial, viral, fungal, parasitic,
- post-traumatic and postoperative syndrome,
- oncological and hematological diseases - lymphoma, neuroblastoma and hepatoblastoma, anemia,
- spleen diseases,
- cirrhosis or polycystic liver disease,
- damage or inflammation of the spinal cord,
- alcoholism,
- intoxication with chemicals that disrupt bone marrow function,
- atherosclerosis,
- diabetes mellitus
Some scientists believe that the increase in P-LCR is due to a congenital stem cell defect. In patients, the process of platelet formation is disrupted. The large cellular elements produced are defective and inactive. They are unable to adequately interact with other structures and function fully.
A high P-LCR index leads to the fact that the patient has a tendency to thrombosis. Due to the adhesive properties of platelets, they stick together and form a blood clot, which disrupts blood circulation and prevents the free movement of blood. As the thrombus grows, it narrows the lumen of the vessel, disrupts the blood supply to the organ, and causes hypoxia and ischemia of the tissue. When the coronary arteries are damaged, this leads to myocardial infarction. With thrombosis of cerebral vessels, an ischemic stroke develops. The result of the process is often varicose veins or atherosclerotic changes in the arteries. These pathologies are deadly and often result in the death of patients.
Symptoms
When the P-LCR increases, the patient develops corresponding clinical signs. They may go unnoticed behind the obvious symptoms of the causative disease. Such patients are not treated for thrombocytosis, which further aggravates the situation.
An increase in P-LCR is manifested by the following symptoms:
- hypersensitivity and pain in the fingertips,
- causeless appearance of hematomas,
- irritation and itching of the skin,
- cyanosis,
- asthenia of the body,
- rapid heartbeat,
- shortness of breath at rest,
- visual dysfunction.
These signs are optional. They can appear individually or in various combinations. But despite this, the patient needs to visit a health care facility and undergo certain tests, based on the results of which doctors will determine the cause of the P-LCR deviation and prescribe appropriate treatment.
Treatment and diagnostic procedures
To determine the cause of the disorder and make a correct diagnosis, in serious cases, a bone marrow biopsy is examined and blood is taken again. Additionally, general clinical and molecular tests and ultrasound of internal organs are performed.
To normalize the P-LCR value, the causative disease . If the pathology is not treated, the patient risks dying from thrombosis, or more precisely from its consequences - acute coronary or cerebral failure. These phenomena are very dangerous. They are often fatal. That is why this deviation needs to be corrected. Hematologists carry out diagnostic and treatment measures. Restoration of normal P-LCR levels in a blood test is a sign of adequate and effective therapy.
- Patients are prescribed a diet rich in vegetables and fruits, vegetable oils, freshly squeezed juices and other products that make the blood less viscous. For the same purpose, experts recommend optimizing your drinking regime - drinking up to 2-3 liters of water per day.
- To prevent thrombosis and its consequences, the use of antiplatelet agents and anticoagulants is indicated - Aspirin, Cardiomagnyl, Trental, Cavinton, as well as drugs that improve microcirculation - Dipyridamole, Piracetam, Vinpocetine.
- If the cause of a high level of large platelets is an infectious disease, then after intensive antibiotic therapy, the P-LCR index value returns to normal almost immediately.
- In severe cases, the use of corticosteroids - Prednisolone, Dexamethasone and cytostatics - Anagrelide, Hydroxyurea, Radioactive phosphorus 32P is indicated.
- To stimulate the immune system, Interferon and its derivatives are prescribed.
- There are folk remedies that allow you to correct (but not eliminate) existing violations. These include: mulberry poison, sweet clover infusion, ginger tea, celery juice. These plants have a beneficial effect on the condition and activity of platelets.
Preparing for the study
Before taking the OAC, you should stop drinking alcoholic beverages, fatty, spicy, excessively salty and fried foods the day before the procedure. Blood is donated on an empty stomach, the patient is advised to maintain physical and emotional peace (refrain from sudden movements, climbing stairs, avoid stressful situations) for half an hour before the test. Also, platelet testing is not recommended immediately after recovery from a long-term illness, which may distort the results due to weakened immunity.
Detailed instructions for preparing for a general blood test are here.
Platelet norms
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory. That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement.
The list shows the reference values of platelet cells adopted in the Invitro laboratory:
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| Children | boys | girls |
| less than 2 weeks | 218 — 419 | 144 — 449 |
| 2 weeks — 1 month | 248 — 586 | 279 — 571 |
| 1 - 2 months | 229 — 562 | 331 — 597 |
| 2 — 6 | 244 — 529 | 247 — 580 |
| 6 months - 2 years | 206 — 445 | 214 — 459 |
| 2 years - 6 years | 202 — 403 | 189 — 394 |
| Adults | men and women | |
| over 6 years old | 150 — 400 | |
In the Helix laboratory there is a slightly different gradation of values:
| Age | Reference values 109/l |
| Less than 10 days | 99 — 421 |
| 10 days – 1 month | 150 — 400 |
| 1-6 months | 180 — 400 |
| 6 months – 1 year | 160 — 390 |
| 1-5 years | 150 — 400 |
| 5-10 years | 180 — 450 |
| 10-15 years | 150 — 450 |
| More than 15 years | 150 — 400 |
It should be noted that the platelet count decreases slightly in women during the menstrual period, but returns to normal after bleeding stops. A slight decrease (up to 150) in platelet concentration during the gestational period is also possible, which is explained by blood dilution due to an increase in BCC (circulating blood volume) and due to insufficient nutrition of the expectant mother.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Thrombocytosis in pregnant women
The options described above also apply to pregnant women, but several more factors are added that affect the increase in platelets.
- Antiphospholipid syndrome is an autoimmune abnormality associated with intense thrombus formation, and during pregnancy this risk increases many times over.
- Toxicosis in pregnant women is characterized by nausea, vomiting, and bloating. Dehydration and insufficient fluid intake against the background of dyspeptic symptoms provoke thrombocythemia.
A significant increase in the level of blood platelets worsens the course of pregnancy until it fails. The deadline does not matter at all.
Drugs that affect platelet levels
Long-term use of these drugs may change platelet levels:
- aspirin
- pain relievers such as ibuprofen and naproxen
- antihistamines
- asthma medicine
- sildenafil (Viagra)
- drugs used to prevent blood clots, such as clopidogrel
- antibiotics
- antidepressants and antipsychotic drugs
- Cholesterol-lowering drugs (statins)
- calcium channel blockers (verapamil).
Platelets are reduced (thrombocytopenia)
When the concentration of platelets in the CBC decreases, they speak of the development of thrombocytopenia, which is accompanied by a blood clotting disorder and a tendency to bleed (gums bleed, nosebleeds or intestinal bleeding often occur, menstruation becomes long and heavy). Thrombocytopenia develops in a number of serious diseases due to the loss of elasticity of the vascular wall, their fragility and fragility and the risk of internal bleeding.
Reasons that provoke a decrease in platelet levels include:
- hemolytic-uremic syndrome or Gasser's disease (a combination of hemolytic anemia, thrombocytopenia and acute kidney failure);
- thrombocytopenic purpura or Werlhof's disease (one of the widows of hemorrhagic diathesis);
- allergic thrombocytopenia (taking a number of medications: procainamide, heparin, co-trimoxazole);
- DIC syndrome (second stage);
- severe liver damage (hepatitis, cirrhosis);
- alcoholism;
- malaria;
- enlarged spleen;
- bone marrow diseases, some leukemias;
- megaloblastic anemia;
- pathology of the thyroid gland (hypothyroidism, thyrotoxicosis).
It is important to note that a decrease in platelet concentration (75 – 150) is observed in pregnant women, which is not regarded as a pathology.
Causes of the secondary form
Secondary thrombocytosis
- increased platelet levels caused by high levels of these substances in the blood.
Most often, such changes in the body are characterized by a chronic course. Among the most common causes of thrombocytosis in women are injuries, internal inflammation, and hematological abnormalities in functioning. In addition, secondary thrombocytosis can be caused by:
Advertising:
- Infections
- most often the disease occurs due to the influence of any bacteria or virus on the body. The influence of such substances can be recognized by changes in certain indicators: white blood cells and leukocytes increase. This indicates the presence of an inflammatory process. - Hematological disorders
- Low iron levels can cause a high platelet count in the blood. Such changes are characteristic of acute blood loss, anemia, and the consequences of chemotherapy. - Removal of the spleen
- 30% of all platelets are constantly located in this organ. During the removal of this organ, the blood cells contained in it enter the general channel, which is why the platelet count begins to grow rapidly. - Injury or surgery
- in this case, the body is affected by post-traumatic stress and the consequences of the operation. Also, the number of platelets in women increases due to pancreatitis, enterocolitis, and tissue necrosis. - Inflammatory processes
- due to increased levels of interleukin - an anti-inflammatory protein - the level of the hormone thrombopoepin increases. This substance promotes accelerated maturation, division and release of platelets. - Malignant tumors
- lymphomas, hepatoblastomas, neuroblastomas. - Taking certain medications
.
[media=
https://youtu.be/arLn-Z53ib0
]
Platelets are increased (thrombocytosis)
An increase in platelet count (thrombocytosis) is observed when:
- excessive physical stress
- chronic inflammatory processes (rheumatoid arthritis, tuberculosis, sarcoidosis);
- myeloproliferative diseases (primary erythrosis, chronic myeloid leukemia, myelofibrosis, myelosclerosis);
- some hemolytic anemias;
- hemolysis or severe blood loss;
- carcinoma, lymphoma;
- after removal of the spleen.
Sources:
- Eugenio D. Hottz. Platelets in Immune Response to Virus and Immunopathology of Viral Infections. — Front Med (Lausanne). Apr 2018.
- Data from the independent laboratory Invitro.
- Data from Helix laboratory.
- Steven Kim, MD. Acquired Platelet Function Disorder. — Healthline, Jan 2021
- Douglas B. Cines. Thrombocytopenia in pregnancy. - Blood. 2017 Nov 23; 130(21): 2271–2277
- Danilova L.A., Doctor of Medical Sciences, Prof. Analyzes of human blood, urine and other biological fluids at different age periods, SpetsLit, 2014.
Diagnostics
Thrombocytosis is detected in a clinical blood test. Although very high platelet counts are more common in hematologic diseases, platelet levels alone cannot determine the cause of thrombocytosis. Therefore, if it is detected, you should visit a therapist. The doctor carefully asks about the patient’s complaints, how long ago the symptoms occurred, and conducts a general examination of the patient. Then, based on the data obtained, an additional examination is prescribed, including:
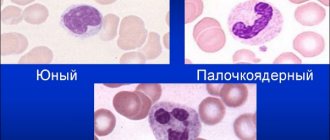
- Blood tests
. In a general blood test, the content of other formed elements (erythrocytes, leukocytes) is determined, and the leukocyte formula is calculated. The concentration of inflammatory markers (ESR, CRP) is measured. The indicators of serum iron, TBC, ferritin are assessed. The presence of autoantibodies (RF, ACCP, antibodies to the cytoplasm of neutrophils) is checked. In case of endocarditis and sepsis, an analysis for procalcitonin and presepsin is performed. - Pathogen identification
. To identify the pathogen, microscopy, bacterial culture of urine and sputum are performed. If tuberculosis is suspected, an intradermal test with tuberculin is prescribed. Using an enzyme immunoassay, antibodies to viruses, parasites, and fungi are detected, and using the polymerase chain reaction method, their DNA and RNA are detected. To diagnose meningitis, a cerebrospinal fluid analysis is informative. - Genetic research
. In patients with myeloproliferative pathologies, mutations of Janus kinase (JAK2V617F), thrombopoietin receptors (MPL), and erythropoietin are determined using fluorescent hybridization (FISH) and PCR. Sometimes chromosomal abnormalities are detected - trisomies, deletions. In chronic myeloid leukemia, cytogenetic analysis reveals the Philadelphia chromosome (Ph). - X-ray
. On an X-ray of the lungs, in case of pneumonia, foci of darkening and infiltrates are noted, in case of tuberculosis - enlargement of the mediastinal lymph nodes, expansion of the roots of the lungs, rounded shadows (cavities) of the upper lobes of the lungs. In patients with arthritis, x-rays of the joints show a narrowing of the joint space, areas of erosion, and marginal osteoporosis. - Ultrasound
. Ultrasound of the abdominal organs in case of pyelonephritis determines compaction and expansion of the pyelocaliceal system, and in case of blood diseases - splenomegaly. In bacterial endocarditis, cardiac echocardiography reveals vegetations of the valves and sometimes effusion into the pericardial cavity. - Endoscopy
. In patients with inflammatory bowel pathologies, fibrocolonoscopy is performed, which reveals hyperemia of the mucous membrane, lack of vascular pattern, erosion, and ulcerative defects. Crohn's disease is characterized by the "cobblestone pavement" symptom - alternating deep ulcers with unchanged mucous membrane. - Histological studies
. In bone marrow aspirate for malignant hematological pathologies, hyperplasia of the megakaryocyte lineage of hematopoiesis is noted (in polycythemia vera - all three lineages), a large number of blast cells (in myeloid leukemia), proliferation of reticulin and collagen fibers (fibrosis). In case of vasculitis, a biopsy of a vessel reveals pronounced perivascular infiltration with lymphocytes and plasma cells.
Platelet count according to Fonio