Saturation is a term that is currently widely heard, because the level of oxygen in the blood is a significant diagnostic factor for coronavirus. However, doctors paid close attention to these numbers even before the pandemic.
Saturation is one of the important indicators of the body’s vital activity - along with body temperature, pressure, etc. It shows the level of oxygen saturation of capillary blood. It helps doctors understand how the respiratory system works. “Saturation is an indicator of oxygen saturation in the blood. It is measured as a percentage and allows us to determine whether our body receives the required amount of oxygen. Normally, in a healthy person it ranges from 95 to 100%. Figures of 94% and below indicate that a person has various types of respiratory failure,” says Elena Dolgikh, deputy chief physician for the medical department of the Khimki Regional Hospital, a doctor of the highest category .
What is saturation
Lung saturation is a term that is an indicator of the level of oxygen saturation in the blood.
Despite the constancy of the visible respiratory process, the intake of life-giving gas into the body can decrease and worsen the well-being and capabilities of the body.
What's important here is why exactly oxygen levels are being monitored. The substance is directly involved in obtaining about 90% of all energy generated by the body. Oxygen carries out the transfer of molecules that feed cells in order to obtain energy when processed during life. Therefore, when its level drops, the entire body suffers.
determination of saturation norm
Quantitative assessment of saturation - percentages, indicating the number of individual hemoglobin molecules compared to the total number of molecules interacting with O2 (the designation of oxygen in chemistry).
There are 2 methods of obtaining the indicator:
- in absolute value – SaO2 (analysis of a blood sample by laboratory method);
- non-invasively, without obtaining a sample - SpO2 (with a special device).
The latter method is used everywhere due to its speed and safety, as well as the absence of a time gap for research in the sometimes critical condition of the patient.
The non-invasive method (from the English invasion - immersion) involves the operation of a device called a “pulse oximeter”. It is attached to your finger and turned on - this takes just a few seconds due to its similarity to a clothespin. After collecting information and analyzing it, lasting no more than a minute, the result is shown on the screen.
pulse oximeter - measurement of blood saturation
The principle of operation is to capture the color spectrum when illuminating blood. With less oxygen content in it, the color will definitely change.
Ambulance teams must have this device in their kit. It takes up little space, weighs almost nothing and is inexpensive.
The essence of the measurements is the same for medical devices and popular electronic sports bracelets. The latter have much less accuracy, but they are also tuned to track hue.
Types of Sleep Apnea
The main manifestation of sleep apnea syndromes is stopping breathing during sleep. But these breathing disorders can be obstructive or central in nature. And this directly affects subsequent treatment.
- Obstructive apnea
occurs due to a mechanical obstruction to air flow. The chest continues to make breathing movements, but air does not enter the lungs. This occurs if the upper respiratory tract is blocked by collapsing pharyngeal walls, a recessed tongue, or hypertrophied tonsils. Depending on the severity of the disease and the cause of the obstruction, the patient may be recommended CPAP therapy, a custom dental mouthguard, surgery, or positional therapy. - Central type apnea
is the result of a malfunction of the respiratory center. Nothing disturbs the airway patency, but the patient breathes very shallowly in comparison with normal breathing or periodically stops breathing - the chest and abdomen remain motionless. In this case, maintenance therapy is most often carried out using more complex and expensive equipment - a BiPAP machine or a servoventilator.
Cardiorespiratory monitoring and, especially, polysomnography also detect other pathologies during sleep, which have a negative impact on night rest in general. These sleep disorders also require treatment and monitoring by a sleep specialist.
What is the norm of saturation in adults - table
What is the norm of saturation in adults - table
What does saturation 99 or 100 mean? In adults, the norm of saturation is in the range from 95 to 99%. There are no deviations in health, and there are no general therapeutic complaints. Individual characteristics of a person should also be taken into account:
- a healthy person without bad habits has an indicator of 95-99%;
- smoker – from 90 to 94% (and the longer the smoking experience, the worse);
- people with a chronic disease of the respiratory system – 90-95%.
Medical personnel consider levels below 94% to be health threatening. If the value is less than 90%, the person receives emergency medical care.
It is characteristic that this indicator is static: the body maintains it at approximately the same level. This was revealed on the basis of statistics and verified many times.
Signs of lack of oxygen
Of course, it is extremely important to understand that there is not enough oxygen as quickly as possible. After all, this will allow you to take action in time. Elena Dolgikh notes that manifestations of a decrease in saturation will be:
- shortness of breath (a person begins to breathe more quickly to compensate for insufficient oxygen levels);
- pale skin;
- tremor of the lower extremities;
- swelling.
All this, naturally, leads to the fact that the person’s condition is disturbed. And quite seriously.
Elena Dolgikh notes that it is important to monitor the numbers on the pulse oximeter. “If the saturation is below 95%, this is already a reason for alarm and a thorough examination by specialists. If there are problems with the lungs, doctors will begin examinations and prescribe the necessary treatment. Covid can also cause a decrease in saturation from the first days. If necessary, the patient will be hospitalized,” says Elena Dolgikh.
So you should pay close attention to yourself so as not to miss the body’s warning signals. Lack of oxygen becomes a serious complication, against the background of which a lack of energy, lethargy, and weakness develop. The longer oxygen starvation, the worse a person becomes. Doctors note that the body literally begins to age before our eyes, immunity deteriorates, the rate of cell renewal decreases, and all systems and organs wear out faster.
Saturation with coronavirus
The disease coronavirus infection (colloquially referred to as “coronavirus”) is characterized by powerful and comprehensive damage to the main respiratory organ – the lungs. The alveoli are primarily affected - single cells that perform gas exchange between the air entering the lungs and the blood that carries oxygen to the cells of the body.
The alveoli and their septa are blocked by the virus and become inflamed, as a result of which their useful work is reduced to zero in a short period of time. Inflammation spreads to neighboring alveoli, and the affected area increases. As a result, the volume of oxygen entering the body per unit of time continuously decreases.
The condition gradually or quite sharply (over 3-5 days) worsens, the state of health is subjectively assessed with the epithets “tired” or “exhausted”, and cold symptoms appear.
The important thing is that the victim does not know about the fact of infection until a state is discovered in which the body is already exhausted, and the volume of lesions in the lungs can lead to disaster.
Saturation during coronavirus is a criterion for the degree of damage to the body. If the value is too low, immediate medical attention is required, including connection to a ventilator.
How to Decipher Sleep Study Report Forms
Report forms for polysomnography and cardiorespiratory monitoring are generated in accordance with accepted standards and present data in the form of graphs, tables and verbal descriptions. By analyzing this information, the specialist identifies characteristic signs of various diseases, conditions or disorders, makes a diagnosis and recommends treatment.
It is of fundamental importance that the somnologist not only considers each sleep parameter separately, but also evaluates their relationships and interdependence. This means that even if you understand the meaning of individual terms in the reporting forms, this will only give you a general idea of your condition. In other words, self-interpretation of test results cannot be considered as an alternative to a visit to the doctor.
And yet, what parameters should you pay attention to first of all in order to at least approximately understand what is happening to you during a night's rest? Let's figure it out.
Reasons for low saturation
Low oxygen saturation in the blood indicates some abnormal health condition. Most often this is:
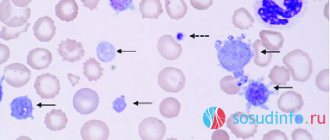
- qualitative and quantitative change in the state of the blood (expressed in a change in the number and characteristics of red blood cells, etc.);
- disease of the respiratory system (from minor pneumonia to cancer);
- excess body weight (taking into account the constitution and standard weight for height);
- diseases of the cardiovascular system (from transient infectious diseases to congenital heart defects).
Smoking is also cited as a cause.
Apnea-hypopnea index (AHI)
The apnea-hypopnea index allows you to determine the severity of the disease - sleep apnea syndrome. The term refers to the average number of complete (apnea) and partial (hypopnea) cessations of breathing for 10 seconds or more recorded per 1 hour of sleep.
Both apnea and hypopnea are periodically observed even in healthy people. And if the number of respiratory events per hour of night rest does not exceed 5, then everything is in order. But a higher AHI indicates breathing pathologies during sleep. The higher the index, the more severe the disease and the more serious consequences it can have for health.
- Normal variant: AHI <5;
- Mild apnea: 5≤ AHI <15;
- Moderate to severe apnea: 15≤ AHI <30;
- Severe apnea: AHI ≥30.
In relation to the most common obstructive variant of sleep apnea, this means the following. A mild degree does not seriously threaten anyone or anything. It's practically the same snoring. Moderate apnea often affects well-being, but usually does not cause serious damage to health. The question of the need and treatment option in this case is decided individually. But severe sleep apnea not only significantly worsens the quality of life, but also significantly increases the likelihood of serious cardiovascular complications - severe arterial hypertension, cardiac arrhythmias, myocardial infarction and stroke. In this case, treatment is mandatory, and CPAP therapy is the most correct and effective option.
What to do with low saturation
At critical levels, life-sustaining drugs and equipment should be used. This is done by the medical staff.
If it is low, it is recommended to do the following:
- breathe fresh and clean air, do breathing exercises;
- drink water in small sips and take blood thinning medications (as prescribed by your doctor);
- consume foods high in iron (buckwheat, meat, apples).
Regular breathing training, combined with physical exercise, will strengthen the body and make it easier to endure any disease due to the improved function of oxygen supply to all tissues in need.
Body position during sleep
Sleeping on your back often leads to increased snoring and more frequent episodes of apnea. But if body position is the main factor causing the problem (i.e. you hardly snore on your side or stomach), you may well be able to influence this with positional therapy. The easiest way is to sew a tennis ball into a T-shirt, which will prevent you from lying on your back. Perhaps this method will help you sleep at least a little better until you and your doctor decide on a more effective and comfortable treatment.
Results and discussion
The average BMI in those examined in the main group was 33.1±6.4 kg/m2. A BMI above 25 kg/m2 was detected in 253 (97.3%) patients: overweight was present in 30.4% of cases, class I obesity in 31.9% of patients, class II obesity in 21.5%, class III obesity in 13.5% (see Table 1).
In the control group, BMI was 26.8±3.6 kg/m2. BMI above 25 kg/m2 was detected in 29 (55.7%) of the examined: overweight in 21 (40.4%), class I obesity in 6 (11.5%), obesity class II and III in 1.9 % of cases respectively.
Pathology of the ENT organs was detected in the majority of patients of the main group: chemotherapy in 165 (63.5%), CAR in 152 (58.5%), INP in 53 (20.4%). Features of the structure of the facial skeleton in the form of retro- and micrognathia were identified in 71 (27.3%) examined.
In the control group, chronic chemotherapy was present in 26 (50%) patients; CAR in 23 (44.2%), IPI in 9 (17.3%). Retro- and micrognathia was found in 23 (44.2%).
According to computer monitoring pulse oximetry, the average saturation values (hemoglobin oxygen saturation in peripheral blood - SPO2) during night sleep in the main group subjects were 92.31±4.73%, which is slightly lower than normal (≥94%). Chronic nocturnal hypoxemia of varying severity was detected in 137 (52.7%). On average, the ID was 25.7±18.7 per hour, while in 105 (40.4%) cases the ID corresponded to mild disorders (5-15 per hour), in 108 (41.5%) it was within 15- 30 per hour (moderate disorders), in 47 (18.1%) the ID was >30 per hour (severe disorders).
In the control group, average saturation values were within normal limits - 96.88±0.9%. On average, ID is also within acceptable values - 1.9±1.4 per hour.
An analysis of the relationship between ID and saturation level (SL) during night sleep showed that an increase in ID is accompanied by a decrease in average saturation levels during night sleep, i.e., the higher the ID during night sleep, the lower the SS ( F
=70.6;
p
<0.001). Accordingly, the more severe the manifestations of OSA (ID), the more the SV decreases during night sleep in this category of patients (Table 2).
Table 2. Relationship between saturation indicators and IR during night sleep according to computer pulse oximetry data. It has been established that with increasing age, IR during night sleep decreases ( R
–0.22;
p
<0.05), and this indirectly confirms the literature data on an increase incidence of OSA in older age groups [1].
The analysis revealed a statistically significant weak correlation between SS and ID during night sleep with gender: a decrease in SPO2 and an increase in ID are more often observed in men ( F
=2,93;
p
<0,05).
It has been established that an increase in BMI is accompanied by an increase in ID ( F
= 16.675553;
p
<0.001) and a decrease in SV during night sleep (
R
= –0.41;
p
<0.05) (Table 3).
Table 3. Relationship I.D.
with BMI in patients undergoing examination for OSA. A study of the relationship between SV during night sleep and pathology of the ENT organs revealed a significant effect of chemotherapy: in patients with this pathology, SV is statistically significantly lower ( F
=70.599975) than in persons without H.T.
The influence of chronic ENT pathology on ID, in particular chemotherapy ( F
= 2.886226), as well as obstruction of the nasal cavity caused by IPN (
F
= 3.856211), was revealed. At the same time, a significant effect on ID of CAP and retro-, micrognathia has not been established.
At the final stage of the work, we used the original author's software application NI5LOG ver. 1.0, with the help of which single- and multifactorial dispersion complexes were constructed and analyzed. Analysis of the obtained dispersion complexes and the corresponding coefficients of the influence of binary and trinary gradation of BMI and pathology of the ENT organs, retromicrognathia on the signs characterizing OSA (SPO2 and ID) showed the following (Table 4):
Table 4. The degree of influence of factors in a two-factor dispersion complex with a binary gradation of BMI BMI as an organized factor has the greatest statistically significant effect on the presence of signs of OSA - 21.02%.
The combined influence of the organized factors BMI and HT is only 1.92% of the statistical influence. The combined influence of the organized factors BMI and HAR amounts to 1.63% of the statistical influence, and BMI and IPI - 0.88%. The combined influence of organized factors of retromicrognathia and increased BMI in the development of OSA symptoms is 3.3% of the statistical influence, and the combination of organized factors of BMI and gender is 1.47%.
It should be noted that the organized factor BMI has the greatest influence on SV during night sleep among other factors or their combinations.
The combination of the organized factors BMI and CT ranges from 20.96 to 23.47% of the statistical influence with a trinary gradation of BMI (Table 5).
Table 5. The degree of influence of factors in a three-factor dispersion complex with a trinary gradation of BMI. The combination of organized factors BMI and CAP ranges from 22.73 to 26.35% of the statistical influence, and BMI and IPI - from 21.73 to 23.06%. The combination of organized factors of retromicrognathia and increased BMI accounts for 21.69 to 27.36% of the statistical influence. In combination with gender, the statistical influence of the BMI factor in the development of OSA symptoms ranges from 23.91 to 24.16%. It should be noted that BMI has the greatest impact on saturation levels during night sleep among other factors or their combinations.
The combined statistical influence of the organized factors BMI, chemotherapy and male gender in the development of OSA symptoms is 60.88%. In this case, the BMI factor has the greatest influence, but an increase in the strength of influence is observed in combination with male gender and chemotherapy.
The combined statistical influence of the organized factors BMI, CT, CHAR in the formation of OSA symptoms is 25.55% (see Table 5). The BMI factor also has the greatest influence, and an increase in the strength of influence is observed in combination with other parameters.
The combined statistical influence of the organized factors BMI, chemotherapy and IPI in the formation of indicators characterizing OSA is 58.23%, the combined statistical influence of the organized factors BMI, chemotherapy and retromicrognathia is 26.67%.
The influence of increased BMI, CAR in combination with retromicrognathia is 52.7%, the combined statistical influence of the organized factors BMI, CAR and INP is 57.65%. BMI in combination with IPI in the presence of retromicrognathia in 56.73% leads to the development of symptoms of OSA.
Thus, chronic obstruction of the nasal cavity, leading to a lack of adequate nasal breathing during night sleep, makes the most significant contribution to changes in saturation parameters during this period. Moreover, the situation is aggravated in the presence of increased BMI.
The combined statistical influence of the organized factors BMI, HAR in combination with male gender is 63.09%. A similar situation is observed with a combination of BMI, INI and male gender (68.66%). The combined statistical influence of organized factors of obesity and retromicrognathia in men is 59.48%.
Having conducted a three-factor analysis of variance of qualitative indicators that secondary characterize OSA, we identified the clinically most significant combinations that increase the risk of developing OSA:
— for the organized factors IPI, increased BMI and male gender, the statistical influence was 68.66%;
- for organized factors CAP, increased BMI, male gender - 63.09%;
- for organized factors of retromicrognathia, increased BMI and male gender - 59.48%;
- for organized factors HT, increased BMI and male gender - 60.88%.
The combination of increased BMI and male gender occurs in all four variants, from which we can conclude that these 2 parameters are the main organized factors leading to the development of OSA. Therefore, overweight or obese men are most susceptible to this disease.
For an integrative assessment of the forces of influence of factors, a generalizing histogram was constructed (see figure).
Percentage distribution of influence forces for each combination of factors. Blue is the three-factor dispersion complex ABC, green is the two-factor dispersion complex BC, blue is the two-factor dispersion complex AC, yellow is the two-factor dispersion complex AB, purple is the one-factor dispersion complex A, brown is the one-factor dispersion complex B (BMI), black is the one-factor dispersion complex complex C. Other explanations in the text. Each histogram column corresponds to a set of influencing factors:
1. Factors: A - “Retromicrognathia”, B - “BMI” and C - “Rhinitis”, plus their various combinations.
2. Factors: A - “Retromicrognathia”, B - “BMI” and C - “Tonsillitis”, plus their various combinations.
3. Factors: A - “Rhinitis”, B - “BMI” and C - “INI” plus all possible combinations thereof.
4. Factors: A – “Tonsillitis”, B – “BMI” and C – “INI” plus all possible combinations thereof.
5. Factors: A - “Tonsillitis”, B - “BMI” and C - “Gender”, plus their various combinations.
6. Factors: A - “Tonsillitis”, B - “BMI” and C - “Rhinitis”, plus their various combinations.
7. Factors: A - “Gender”, B - “BMI”, C - “Retromicrognathia”, plus all possible combinations thereof.
8. Factors: A - “Gender”, B - “BMI” and C - “Rhinitis”, plus their various combinations.
9. Factors: A - “Retromicrognathia”, B - “BMI” and C - “INI”, plus their various combinations.
10. Factors: A - “INI”, B - “BMI” and C - “Gender” plus all possible combinations thereof.