Lymphangitis of the penis is a serious disease associated with inflammation of the lymphatic vessels. The pathological process occurs along the shaft of the penis or around the coronary sulcus. It causes significant discomfort and is accompanied by copious discharge of pus. In 90% of cases it develops due to mechanical injuries. The risk group includes men with increased sensitivity in the groin area. The causes of lymphangitis include:
- frequent sexual intercourse
- increased masturbation,
- choosing an inappropriate position for sex,
- painful stimulation of the penis,
- regular damage to the penis.
The disease is not sexually transmitted. However, its symptoms are similar to some sexually transmitted infections. Only a doctor can make a differential diagnosis. Therefore, if suspicious signs are detected, you must promptly contact a specialist.
General information
Lymphangitis (lat. lymphangoitis) is an acute inflammatory process of lymphatic vessels of various locations/calibers (lymphatic capillaries, vessels, trunks), developing as a complication of local purulent-inflammatory foci or infected skin lesions. That is, lymphangitis is a secondary disease, most often developing against the background of an infected wound , boil / carbuncle , panaritium , phlegmon , abscess , trophic ulcers , erysipelas, etc. or skin damage (microtraumas, abrasions, scratching, bites). As a rule, lymphangitis is accompanied by lymphadenitis (enlargement of the submandibular, cervical, supra/subclavian, axillary, inguinal, popliteal and other lymph nodes). The place of primary localization of the purulent-inflammatory process and lymphangitis is the upper/lower extremities (photos of lymphangitis are given below), but since the human lymphatic system is extremely extensive, the pathological process can develop on any part of the body.
Lymphangitis is accompanied by
painful swelling / hyperemia of inflamed lymphatic vessels along their course, regional lymphadenitis , edema , weakness , chills , and increased body temperature.
In andrology/urology, a condition such as “non-venereal lymphangitis of the penis” is often diagnosed. Non-venereal lymphangitis develops when the tissues of the penis are injured (during prolonged sexual intercourse/frequent masturbation). Its manifestation is the appearance of a painless, compacted (on palpation) lymphatic vessel localized along the shaft of the penis or parallel to the coronary groove. As a rule, such manifestations of lymphangitis do not require treatment, and they disappear without a trace/spontaneously within 1-2 days.
Treatment of lymphangitis
Any therapeutic measures for the disease in question begin with eliminating the main source of infection. In case of suppuration, treatment is carried out in a hospital setting; the suppurating lymph node is opened. If lymphangitis of the extremities is diagnosed, then it is necessary to ensure their immobility - the arm or leg must be fixed in an elevated position, which allows for complete drainage of lymph. The patient is recommended to be sedentary and drug therapy is prescribed:
- antibiotics;
- cephalosporins;
- aminoglycosides;
- antihistamines.
To alleviate the patient's condition against the background of general intoxication of the body, infusion therapy is carried out. If the pathology occurs in a chronic form with a vague clinical picture (this is different, for example, from pulmonary lymphangitis), then compresses with dimethyl sulfoxide, physiotherapeutic procedures - mud therapy, irradiation with ultraviolet rays will be effective.
Damage to the penis requires special attention. In case of non-venereal origin, no specific treatment is required, but for 2-3 days it is recommended not to have sexual relations and avoid injury. If lymphangitis of the penis is diagnosed against the background of a progressive sexually transmitted infection, then it is treated.
More information about the pathology and what epizootic lymphangitis is can be found on the pages of our website https://www.dobrobut.com/.
Pathogenesis
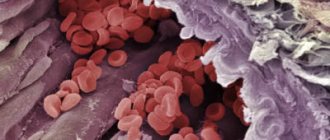
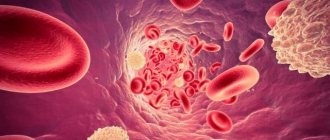
In the development of lymphangitis, a significant role is played by the anatomical and physiological specificity of lymph circulation in one or another part of the body, the localization/depth of the wound or primary inflammatory focus, the virulence of pathogenic microflora and the state of general immunity . Pathogens/their toxins initially enter the interstitial spaces, and then move into the lymphatic vessels from the primary site of infection with the lymph flow into large-caliber lymphatic vessels or adjacent lymph nodes.
Their action is manifested by a reactive inflammatory process of the walls of lymphatic vessels with swelling of the vascular endothelium, increasing its permeability, release of exudate and loss of fibrin with the formation of clots (thrombi), which contributes to the development of local lymph circulation disorders (lymphostasis). The pathological process develops as endolymphangitis / panlymphangitis with its spread towards the lymph nodes.
As the inflammatory process progresses, purulent lymphangitis , and in the absence of treatment, purulent fusion of blood clots. perilymphangitis develops with damage to muscles, blood vessels, joints, etc.
Why is lymphangitis dangerous?
Long-term lymphangitis can lead to:
- lymph circulation disorder (the qualitative composition of lymph changes, its quantity increases significantly);
- obliteration of lymphatic vessels (the lumen of the vessel becomes overgrown);
- development of elephantiasis (skin and subcutaneous tissue thicken due to chronic inflammation of the lymphatic vessels), lymphostasis (tissue swelling resulting from impaired lymph outflow);
- abscess (purulent inflammation of tissues with their melting, which leads to the formation of a purulent cavity);
- sepsis (a systemic inflammatory reaction diagnosed as a result of infectious agents entering the blood);
- cellulite (changes in the structure of the subcutaneous fat layer, which lead to disturbances in lymphatic outflow and lymph circulation).
Classification
The classification is based on several factors, according to which they distinguish:
- Depending on the etiological factor, nonspecific and specific lymphangitis .
- Depending on the course – acute and chronic.
- According to the depth of the affected vessels - superficial and deep.
- The nature of the inflammation is serous (simple) and purulent.
- According to the caliber of the affected vessels - capillary (reticular/mesh), in which an extensive network of small capillaries is involved in the pathological process, and truncular (stem), which is based on inflammation of one/several large vessels.
Diagnostics
To diagnose acute reticular lymphangitis, as a rule, a simple examination is sufficient, but it should be separated from erysipelas and superficial phlebitis. It is very important to correctly identify the primary source of inflammation.
Acute truncular lymphangitis is differentiated from superficial thrombophlebitis.
Deep lymphangitis causes difficulties in diagnosing the disease. To determine it, a comprehensive examination is carried out.
Causes
The etiological factor of nonspecific lymphangitis is pathogenic pyogenic microflora. The most common causative agents of the disease include coccal flora (Staphylococcus aureus/beta-hemolytic streptococcus), Pseudomonas aeruginosa , Escherichia coli , Proteus , both in the form of a monoculture and their combinations, and in patients with immunodeficiency - anaerobes and gram-negative bacteria .
Specific lymphangitis in a patient is associated primarily with the presence of tuberculosis infection (Koch bacillus), syphilis (treponema pallidum), plague (plague bacillus), actinomycosis (actinomycete bacteria), genital herpes (herpes simplex virus type 1/2), etc.
Predisposing factors are the presence of local purulent-inflammatory foci/infected skin lesions and decreased immunity .
Symptoms
Acute lymphangitis is characterized by severe general intoxication accompanying the purulent-inflammatory process, manifested by weakness , chills , high temperature (39-40°C), sweating and headache . With reticular lymphangitis, superficial pronounced hyperemia first appears in the area of the source of infection ( abscess , boil , etc.) with a pronounced mesh pattern against the background of increasing erythema . At the same time, reticular lymphangitis in clinical symptoms resembles erysipelas , but hyperemia has unclear boundaries uncharacteristic of erysipelas.
A local manifestation of stem lymphangitis is the presence on the skin of red stripes of narrow inflamed lymphatic vessels towards the regional lymph nodes. There is induration, swelling and pain in the inflamed cord-type cords, tension/swelling of the surrounding tissues, and often the development of regional lymphadenitis.
When deep vessels are damaged, there is no local hyperemia, but pain and swelling in the affected area quickly increases; on palpation - severe pain, lymphedema .
In the chronic course of lymphangitis, the clinical symptoms are erased and manifest mainly by persistent edema and lymphostasis caused by blockage of the deep lymphatic trunks with minimal appearance of a general nature.
Diagnosis of lymphangitis
A lymphologist can diagnose regional lymphangitis during a routine visual examination. In this case, the disease must be differentiated from superficial phlebitis and erysipelas, which can only be done through laboratory and instrumental studies.
Diagnostic signs of lymphangitis:
- pronounced leukocytosis in peripheral blood;
- duplex scanning and ultrasound doppler scanning reveal changes in the lymphatic vessels according to the type of heterogeneity of structure, narrowing of the lumen, reticular changes in the lymph nodes;
- during computed tomography, it is possible to determine the depth and extent of lymphangitis, to distinguish the disease from other pathologies that have similar symptoms;
- Bacteriological culture of a detachable purulent wound makes it possible to identify the pathogen.
In case of a complicated form of the disease, a blood test for sterility is required.
Tests and diagnostics
Diagnosis of superficial lymphangitis is not difficult and is based on clinical symptoms and the presence of a focus of primary infection. To diagnose lymphangitis of deep lymph nodes, additional laboratory and instrumental studies are carried out:
- Complete blood count (increased ESR/moderate leukocytosis).
- Blood test (bacteria culture) for sterility.
- Bacterial culture of discharge from the primary source of infection in order to identify the pathogen and determine its sensitivity to antibiotics.
- Doppler ultrasound/duplex scanning/CT. Allows you to visualize the narrowing of the lumen of the lymphatic vessels/hardening of soft tissues, the extent of the pathological process.
Differential diagnosis with deep vein thrombophlebitis , soft tissue phlegmon , osteomyelitis , erysipelas .
Diagnostics and therapy
An andrologist treats lymphangitis. The disease is diagnosed by examination and palpation of the penis. A lump on the penis is one of the main signs of inflammation of the lymphatic trunks. To confirm the diagnosis, the patient may be given a blood test. If no antibodies to syphilis are detected, the doctor will develop an individual treatment regimen for lymphangitis.
At the initial stages of development, the inflammatory process can go away on its own. However, in advanced cases, professional medical help cannot be avoided. In the presence of purulent foci, their opening and drainage is indicated. The patient is also prescribed antibacterial and antiseptic drugs. After the final suppression of the purulent process, physiotherapeutic procedures are indicated. They promote lymphatic drainage and rapid wound healing.
You can make an appointment with a specialist by calling the number listed on the website. We will select a convenient time for your appointment. The cost of the clinic's services is shown in the price list.
Prevention
Prevention consists of preventing purulent infection. A healthy lifestyle and strong immunity play a big role in this. If you have cuts or other wounds, it is important to promptly treat them with antiseptics at home. If ulcers appear ( furuncle , carbuncle , abscesses after insect bites, etc.), you need to contact a surgeon in time to sanitize the lesions and follow his instructions regarding taking antibiotics (if necessary).
Treatment options
The main therapy is designed to eliminate the primary focus. The patient's wounds are treated, opened, the contents of the inflammation are removed and sanitized.
It is forbidden to heat or massage inflamed areas. The patient must remain in bed.
Drug treatment involves taking:
- antibacterial agents;
- antiallergic drugs;
- anti-inflammatory complexes.
Physiotherapy methods include irradiation of the patient's blood with laser and ultraviolet light.
Surgical methods are used when it is necessary to drain abscesses.
List of sources
- Ermolaev V. L., Makarova N. P. Diseases of lymphatic vessels and nodes. Ekaterinburg: GBOU VPO USMU Ministry of Health of Russia, 2015. – 264 p.
- Shlyapnikov S.A. Surgical infections of soft tissues - an old problem in a new light // Infections in surgery, 2003, No. 1(1). – P. 14-21.
- Belousova T.A., Kayumova L.N., Goryachkina M.V. Systemic antibiotics in the treatment of bacterial infections of the skin and soft tissues: focus on macrolides / breast cancer. - 2011. - No. 5.
- Guchev I.A., Sidorenko S.V., Frantsuzov V.N. Rational antimicrobial chemotherapy for skin and soft tissue infections. Antibiotics and chemotherapy. 2003, vol. 48, 10, pp. 25–31.
- Surgical infection: A guide for general practitioners / Stolyarov E.A., Grachev B.D., Kolsanov A.V., Batakov E.A., Sonis A.G. - 2004.