Arrhythmia
- a definition that reflects changes in the frequency, regularity, source of excitation of the heart and various types of disturbances in its electrical conductivity.
Heart rhythm disturbances are a widespread disease of our time.
The abundance of causative factors, the difference in the electrophysiological mechanisms of the formation of arrhythmias and the topography of the zones in which these mechanisms are executed, the difference in ECG indicators, manifestations and prognosis determine the polymorphism of heart rhythm disorders.
What is atrial rhythm
Myocardial contractions normally occur regularly and do not depend on consciousness: even when the brain dies, the heart still works for some time.
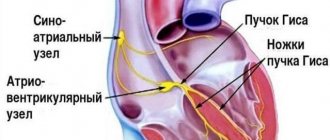
This process is very important for maintaining life. Failures occur due to serious damage to the cell structure or metabolic disorders. If the main pacemaker is affected, its function passes to the underlying sections located in the atria, atrioventricular zone, and bundle branches.
In this case, the normal impulse becomes too weak or absent. If the generation of myocardial contractions comes from the atria, then in this case an atrial ectopic rhythm is recorded on the ECG.
Causes and types
The main causes of atrial, as well as any ectopic (displaced) rhythm, are:
- Changes in the structure of the myocardium - as a result of inflammation, ischemia, cardiosclerosis, hypertrophy or dystrophy.
- Valve defects and other congenital anomalies.
- Violation of electrolyte and water levels. This happens with a sudden loss of fluid (vomiting, diarrhea, taking diuretics).
- Metabolic changes in diseases of the endocrine organs.
- Internal or external intoxication (impaired kidney and liver function, smoking, alcoholism, drug addiction, ingestion of heavy metal salts, etc.).
- Overdose of cardiac glycosides.
- Traumatic chest injury.
All these reasons are characteristic of ectopic atrial impulses in an adult. In children and adolescents, they most often occur against the background of impaired autonomic innervation.
Depending on the frequency of contractions, slow and accelerated atrial rhythms are distinguished. The lower the pacemaker is located in the conduction system, the rarer the pulse - up to 45–60 beats per minute. An increase of up to 130 or more occurs when, under the influence of inflammation or other pathology, hyperexcitation and excessive activity of the ectopic focus develop.
The displaced rhythm may be permanent or temporary. According to localization, it can be left or right atrial, but this division has no particular clinical significance and does not affect the prescribed treatment regimen.
Ectopic impulses can vary in frequency, regularity and strength. But in the absence of normal sinus rhythm, they allow the heart to continue pumping.
ECG diagnostics of dysfunctions of sinus node automatism, replacement complexes and rhythms
The sinus node (sinoauricular node, Keys–Flac node) (SU) is the normal pacemaker of the heart. Pacemaker cells of the SG (first order pacemaker) have the greatest automaticity; they generate 60–90 impulses per minute. Disorders of the automatism function of the SG can be divided into types that have and do not have hemodynamic significance, which, in turn, makes their timely and correct diagnosis extremely important, which makes it possible to prescribe adequate therapy and avoid (including iatrogenic) errors in the process treatment, to prevent the development of sudden death and other complications. Table 1 presents the classification of rhythm and conduction disorders [1–5].
According to the etiology, heart rhythm disturbances can be divided into the following main types: 1. Dysregulatory or functional: associated with disorders of neuroendocrine regulation, autonomic dysfunction, psychogenic influences, fatigue, reflex influences (gastritis, peptic ulcer, aerophagia, Roemheld syndrome, cholelithiasis, nephroptosis, urolithiasis, colitis, constipation, flatulence, pancreatitis, intervertebral hernia, embolism in the pulmonary artery system, mediastinal tumors, bronchopulmonary processes, pleural adhesions, chest surgery, genital diseases, skull injuries, brain tumors, multiple sclerosis). 2. Myogenic or organic: associated with myocardial diseases (cardiomyopathy, myocarditis, post-myocardial cardiosclerosis, myocardial dystrophy), with damage to cardiomyocytes that occurs against the background of coronary heart disease (myocardial infarction, ischemic cardiomyopathy), hypertension, heart defects. 3. Toxic: occurring under the influence of drugs (cardiac glycosides, anesthetics, tranquilizers, antidepressants, neuroleptics, aminophylline and its analogues, adrenomimetics (adrenaline, nor-adrenaline, mesaton, dobutamine, dopamine, salbutamol), acetylcholine, vagolytics (atropine), glucocorticosteroids, ACTH, antiarrhythmic drugs, cytostatics, antiviral drugs, antifungal drugs, antibiotics, diuretics, ether, alcohol, caffeine, nicotine, heavy metal salts, benzenes, carbon monoxide, mushroom poisoning, infections, endogenous intoxication in oncopathology, uremia, jaundice and etc. 4. Electrolytic: hypokalemia, hyperkalemia, hypocalcemia, hypercalcemia, hypomagnesemia 5. Dyshormonal: thyrotoxicosis, hypothyroidism, pheochromocytoma, puberty, menopause, pregnancy, hypopituitarism, ovarian dysfunction, premenstrual syndrome, tetany 6. Congenital: congenital atrioventricular (AV) conduction disorders, long QT syndrome, ventricular preexcitation syndromes (WPW, CLC, etc.). 7. Mechanical: cardiac catheterization, angiography, cardiac surgery, cardiac trauma. 8. Idiopathic. ECG diagnosis of arrhythmias caused by dysfunction of the automatism of the sinus node is carried out using an electrocardiographic study, which allows us to identify the following main types [1, 2, 4–16]. 1. Sinus tachycardia
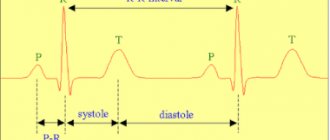
– this is a regular rhythm with unchanged ECG waves (P wave, PQ interval, QRS complex and T wave do not differ from the norm) from the sinus node with a frequency of > 90 per minute. Sinus tachycardia at rest rarely exceeds 150–160 beats per minute (Fig. 1) [1, 16].
Differential diagnosis:
– supraventricular non-paroxysmal tachycardia;
– supraventricular paroxysmal tachycardia; – atrial flutter 2:1; – atrial fibrillation with ventricular tachysystole; – ventricular paroxysmal tachycardia. Etiology
: – physiological tachycardia: physical activity, emotions, fear, orthostatic, congenital features;
– neurogenic tachycardia: neurosis, neurocirculatory asthenia; – CVD: inflammatory and degenerative myocardial diseases, valve defects, collapse, heart failure, cor pulmonale, myocardial infarction, arterial hypertension; – drug and toxic tachycardia: vagolytics (atropine), sympathicotonics (adrenaline, norepinephrine, mesaton, dobutamine, dopamine), aminophylline, corticosteroids, ACTH, caffeine, coffee, tea, alcohol, nicotine; – infectious diseases: ARVI, sepsis, pneumonia, tuberculosis, etc.; – other: blood loss, anemia. 2. Sinus bradycardia
– slowing of the sinus rhythm with heart rate < 60 per minute due to reduced automaticity of the sinus node. Sinus bradycardia with a heart rate <40 beats per minute is rare (Fig. 2) [1, 16].
Differential diagnosis:
– AV block II stage.
2:1 or 3:1; – AV block, stage III; – atrial rhythms; – nodal rhythm; – atrial fibrillation with ventricular bradysystole, Frederick’s syndrome; – atrial flutter with conduction 4:1, 5:1; – SA blockade, SA failure; - atrial extrasystole. Etiology
: – physiological bradycardia: constitutional, in athletes and people engaged in physical work, during sleep, during vagal tests (pressure on the eyeballs, solar plexus and carotid sinus, Valsalva test), during breath holding, sometimes with fear, emotions , in the second half of pregnancy, with vomiting and hypothermia;
– extracardial vagal bradycardia: neurosis with vagotonia, depression, peptic ulcer, increased intracranial pressure with cerebral edema, meningitis, brain tumor, cerebral hemorrhage, labyrinth diseases, Meniere’s syndrome, hypersensitive carotid sinus, shock, increased blood pressure, vago-vagal reflexes for renal, biliary, gastric and intestinal colic, intestinal obstruction, myxedema, hypopituitarism; – drug and toxic bradycardia: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, cordarone, sotalol, calcium antagonists, anesthetics, tranquilizers, antipsychotics, pilocarpine. Uremia, jaundice, mushroom poisoning, hyperkalemia; – infectious diseases: viral infections (viral hepatitis, influenza), typhoid fever, diphtheria, cholera; – CVD: ischemic heart disease, diphtheria myocarditis, rheumatism, cardiomyopathies. 3. Sinus arrhythmia
– irregular activity of the sinus system, leading to alternating periods of increased and decreased rhythm.
There are respiratory and non-respiratory sinus arrhythmia [1, 16]. With respiratory sinus arrhythmia, the heart rate gradually increases when inhaling, and slows down when exhaling. Non-respiratory sinus arrhythmia persists during breath-holding and is not associated with the phases of breathing. Non-respiratory sinus arrhythmia, in turn, is divided into 2 forms: periodic (periodic, gradual alternation of acceleration and deceleration of cardiac activity) and aperiodic (lack of gradual alternation of phases of acceleration and deceleration of cardiac activity) (Fig. 3). Etiology
: – physiological arrhythmia: adolescents, elderly people;
– extracardiac diseases: infectious diseases, temperature reactions, obesity, pleuro-pericardial adhesions, increased intracranial pressure; – CVD: rheumatism, ischemic heart disease, heart defects, heart failure; – drug and toxic arrhythmia: opiates, cardiac glycosides, vagotonics. Differential diagnosis:
– AV block II stage;
– SA blockade, SA failure; – migration of the pacemaker through the atria; – atrial fibrillation; – atrial flutter (irregular shape); - atrial extrasystole. 4. Stopping the control system
(failure of the control system, sinus arrest, sinus pause, sinus-inertio) – periodic loss of the control system’s ability to generate impulses. This leads to loss of excitation and contraction of the atria and ventricles [1, 16, 17]. There is a long pause on the ECG, during which the PQRST waves are not recorded and the isoline is recorded. The pause when stopping the ultrasound is not a multiple of 1 RR (PP) interval (Fig. 4).
Etiology
: – reflex: sensitive carotid sinus, vagal tests;
– medicinal and toxic arrest of sinusitis: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, calcium antagonists. Hypokalemia, intoxication; – CVD: coronary artery disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus. Differential diagnosis:
– AV block II-III stage;
– blocked atrial extrasystoles; – SA blockade, stage II; – atrial fibrillation with ventricular bradysystole, Frederick’s syndrome; – nodal rhythm; – sinus arrhythmia; – sinus bradycardia; – atrial asystole. 5. Atrial asystole
(partial asystole) – absence of atrial excitation, which is observed during 1 or (more often) more cardiac cycles [1, 12, 16]. Atrial asystole can be combined with ventricular asystole, in such cases complete cardiac asystole occurs. However, during atrial asystole, pacemakers of the II, III, IV order usually begin to function, which cause excitation of the ventricles (Fig. 5).
Etiology
: – reflex: sensitive carotid sinus, vagal tests, intubation, deep breathing, due to irritation of the pharynx;
– medicinal and toxic: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, calcium antagonists. Hyperkalemia, intoxication, hypoxemia; – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus, terminal cardiac condition. Differential diagnosis:
– AV block II-III stage;
– SA blockade, stage II; – blocked atrial extrasystoles; – atrial fibrillation with ventricular bradysystole; – Frederick's syndrome; – nodal rhythm; – sinus arrhythmia, sinus bradycardia; – SU stop. 6. Sick sinus syndrome
(SSNS) (sinus sinus syndrome dysfunction, bradycardia and tachycardia syndrome, sick sinus syndrome, Short syndrome, sick sinus syndrome, lazy sinus syndrome, sluggish sinus syndrome) is the presence of one or more of the following signs [1, 3–5 , 11, 12, 16, 17]: – persistent severe sinus bradycardia (Fig. 2); – the minimum heart rate determined during daily ECG monitoring for 1 day is <40 per 1 min, and its increase during physical activity does not exceed 90 per 1 min; – bradysystolic form of atrial fibrillation; – migration of the atrial pacemaker (Fig. 12); – stopping the SU and replacing it with other ectopic rhythms (Fig. 6–10, 13); – sinoauricular block; – pauses >2.5 s that occur as a result of the arrest of the sinus system, SA blockade, or rare replacement rhythms (Fig. 6);
– tachy-brady syndrome, alternating periods of tachycardia and bradycardia (Fig. 6); – rarely attacks of ventricular tachycardia and/or ventricular fibrillation; – slow and unstable restoration of the function of the suture system after extrasystoles, paroxysms of tachycardia and fibrillation, as well as at the moment of termination of stimulation during electrophysiological examination of the heart (post-tachycardial pause, which normally does not exceed 1.5 s, in case of suction systolic systolic activity can reach 4–5 s); – inadequate reduction in rhythm when using even small doses of beta blockers. Presence of bradycardia during the administration of atropine and exercise testing.
Classification
There is no unified classification of SSSU.
Depending on the nature of the lesion, true (organic), regulatory (vagal), medicinal (toxic) and idiopathic SSS are distinguished (Fig. 6). According to clinical manifestations, the following are distinguished:
– latent SSSU: there are no changes on the ECG, and the pathology of the SS is detected by additional functional research methods (EFI);
– compensated SSSU: no clinical changes, there are changes on the ECG; – decompensated SSSU: there are clinical and ECG manifestations of the disease. Based on ECG signs, the following are distinguished: – bradyarrhythmic variant of SSSS. – tachycardia-bradycardia syndrome. Etiology
: – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, rheumatism, congenital defects; – reflex: sensitive carotid sinus, vagal tests, reflex effects in peptic ulcers, cholelithiasis, hiatal hernia; – medicinal and toxic: cardiac glycosides (digoxin, strophanthin), opiates, acetylcholine, quinidine, beta blockers, calcium antagonists. Hyperkalemia, intoxication, hypoxemia; – idiopathic forms.
Passive ectopic complexes and rhythms
Reduced activity of the sinus sinus or complete blockade of sinus impulses due to functional or organic damage to the sinus system causes the activation of automatic centers of the second order (cells of atrial pacemakers, AV connection), third order (His system) and fourth order (Purkinje fibers, ventricular musculature).
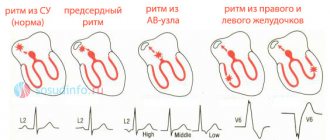
Automatic centers of the second order produce unchanged ventricular complexes (supraventricular type), while centers of the third and fourth order generate dilated and deformed ventricular complexes (ventricular, idioventricular type). The following rhythm disturbances have a substitutive nature: atrial, nodal, migration of the pacemaker through the atria, ventricular (idioventricular rhythm), jumping contractions [1, 5, 16]. 7. Atrial rhythm
(slow atrial rhythm) - a very slow ectopic rhythm with foci of impulse generation in the atria (Table 2).
Right atrial ectopic rhythm is the rhythm of an ectopic focus located in the right atrium. The ECG shows a negative P wave in leads V1-V6, II, III, aVF. The PQ interval is of normal duration, the QRST complex is not changed. Coronary sinus rhythm (coronary sinus rhythm) - impulses to excite the heart come from cells located in the lower part of the right atrium and the coronary sinus vein. The impulse propagates through the atria retrogradely from bottom to top. This leads to the registration of negative P waves in leads II, III, aVF. The PaVR wave is positive. In leads V1-V6 the P wave is positive or 2-phase. The PQ interval is shortened and typically <0.12 s. The QRST complex is unchanged. The coronary sinus rhythm may differ from the right atrial ectopic rhythm only by shortening the PQ interval. Left atrial ectopic rhythm - impulses to excite the heart come from the left atrium. In this case, a negative P wave is recorded on the ECG in leads II, III, aVF, V3-V6. The appearance of negative P waves in I, aVL is also possible; the P wave in aVR is positive. A characteristic sign of left atrial rhythm is the P wave in lead V1 with an initial rounded dome-shaped part, followed by a pointed peak - “shield and sword” (“dome and spire”, “bow and arrow”). The P wave precedes the QRS complex with a normal PR interval of 0.12–0.2 s. Atrial rate is 60–100 per minute, rarely <60 (45–59) per minute or >100 (101–120) per minute. The rhythm is correct, the QRS complex is not changed (Fig. 7).
Regular rhythm with a negative wave PI, II, III, aVF, V3-V6 before the QRS complex. The P wave in lead V1 has an initial rounded dome-shaped portion followed by a pointed peak—a “shield and sword.” Normal PR interval = 0.12-0.2 s. Inferior atrial ectopic rhythm is the rhythm of an ectopic focus located in the lower parts of the right or left atria. This leads to the registration of negative P waves in leads II, III, aVF and a positive P wave in aVR. The PQ interval is shortened (Fig. 8). Differential diagnosis:
– sinus arrhythmia;
– nodal rhythm; – migration of the pacemaker through the atria; – atrial flutter; – polytopic atrial extrasystole; – atrial rhythms (right atrial, left atrial, lower atrial, coronary sinus rhythm). 8. Nodal rhythm
(AV rhythm, replacing AV nodal rhythm) - heart rhythm under the influence of impulses from the AV junction with a frequency of 40–60 per minute. There are 2 main types of AV rhythm [1]: – junctional rhythm with simultaneous excitation of the atria and ventricles (junctional rhythm without P wave, junctional rhythm with AV dissociation without P wave): the ECG shows an unchanged or slightly deformed QRST complex, P wave absent (Fig. 9);
– junctional rhythm with different-time excitation of the ventricles and then the atria (junctional rhythm with a retrograde P wave, isolated form of the AV rhythm): an unchanged QRST complex is recorded on the ECG, followed by a negative P wave (Fig. 10).
Differential diagnosis:
– sinus bradycardia;
– atrial rhythm; – migration of the pacemaker through the atria; – polytopic atrial extrasystole; – idioventricular rhythm. 9. Migration of the pacemaker through the atria
(wandering rhythm, sliding rhythm, migrating rhythm, migration of the cardiac pacemaker, wandering pacemaker). There are several variants of the wandering (wandering) rhythm [1, 5,15]: Wandering rhythm in the SU. The P wave is of sinus origin (positive in II, III, aVF), but its shape changes with different heart contractions. The PR interval remains relatively constant. Severe sinus arrhythmia is always present. Wandering rhythm in the atria. The P wave is positive in II, III, aVF, its shape and size change with different heart contractions. Along with this, the duration of the PR interval changes. Wandering rhythm between the sinus and atrioventricular nodes. This is the most common variant of the wandering rhythm. With it, the heart contracts under the influence of impulses that periodically change their location: they gradually move from the suture block, atrial muscles to the AV junction and return to the suture block again. ECG criteria for pacemaker migration in the atria are ≥ 3 different P waves in a series of cardiac cycles, a change in the duration of the PR interval. The QRS complex does not change (Fig. 11, 12).
Etiology
: – reflex: healthy people with vagotonia, sensitive carotid sinus, vagal tests, intubation, deep breathing;
– medicinal and toxic effects: cardiac glycosides (digoxin, strophanthin), quinidine. Infectious diseases, intoxication; – CVD: ischemic heart disease, rheumatism, heart defects, heart surgery. Differential diagnosis:
– SA blockade II degree, failure of the SA;
– AV block II stage; – atrial fibrillation; – sinus arrhythmia; – polytopic atrial extrasystole. 10. Idioventricular (ventricular) rhythm
(intrinsic ventricular rhythm, ventricular automatism, intraventricular rhythm) - ventricular contraction impulses arise in the ventricles themselves. ECG criteria: widened and deformed QRS complex (>0.12 s), rhythm with heart rate < 40 per 1 min (20–30 per 1 min). Terminal idioventricular rhythm is very slow and unstable. The rhythm is often correct, but may be incorrect if there are several ectopic foci in the ventricles or the presence of one foci with varying degrees of impulse formation or exit block. If an atrial rhythm is present (sinus rhythm, atrial fibrillation/flutter, ectopic atrial rhythm), it is independent of the ventricular rhythm (AV dissociation) (Fig. 13, 14) [1, 5, 16, 17].
Differential diagnosis:
– AV block, stage III;
– SA blockade II-III stage; – atrial fibrillation with ventricular bradysystole, Frederick’s syndrome; – nodal rhythm; – sinus bradycardia; – jumping contractions. Etiology
: – medicinal and toxic effects: cardiac glycosides (digoxin, strophanthin), quinidine.
Infectious diseases, intoxication; – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus, terminal cardiac condition. 11. Jumping contractions
(replacement systoles, escape systoles, ersatzsystolen, echappements ventriculaires, individual automatic contractions of the ventricles) - single impulses from the AV junction or ventricles. The difference between jumping contractions and nodal or idioventricular rhythm is the absence of a long period of contractions [1, 16]. Nodal jump-out contractions (the QRS complex is not changed and is the same in shape as the rest of the ventricular complexes. A jump-out contraction can be recognized by the position of the negative P wave or its absence) (Fig. 15). Ventricular jump contractions (the QRS complex is deformed and widened) (Fig. 16).
ECG criteria: the RR interval before the jumping contraction is always longer than 1 whole interval, and not shortened, as with extrasystole. The RR interval after the pop-up contraction is of normal length, rather than lengthened as with extrasystole, and in all cases shorter than the interval preceding the pop-up contraction. Etiology
: – medicinal and toxic effects: cardiac glycosides (digoxin, strophanthin), quinidine.
Infectious diseases, intoxication; – CVD: ischemic heart disease, myocarditis, cardiomyopathies, surgical damage to the sinus, weakness of the sinus, terminal cardiac condition. Differential diagnosis: – sinus arrhythmia;
– atrial extrasystole; – ventricular extrasystole; – migration of the atrial pacemaker; – SA blockade, stage II, failure of the SU; – AV block II stage; – nodal rhythm; – idioventricular rhythm.
Conclusion
The variety of dysfunctions of the automatism function of the control system significantly complicates their diagnosis. Nevertheless, the relevance of adequate assessment of SU dysfunction is beyond doubt.
What is the danger
Active generation of heart rhythm from an atypical focus is most often a symptom of pathology of the myocardium or other organs and systems. I recommend that you undergo additional examinations and identify the cause of ectopia.
Rhythm and hemodynamic disturbances, especially with a high frequency of contractions and concomitant diseases, can lead to the formation of blood clots, angina attacks, the development of a heart attack, flicker, flutter and the gradual formation of heart failure.
Etiology of arrhythmia
of diseases can become fertile ground for the onset of arrhythmia.
, both
cardiovascular
and other body systems.
These are hypertension, coronary artery disease and myocardial infarction, heart failure, inflammatory, dystrophic diseases of the myocardium, valve defects (congenital and acquired), anomalies of heart development. Often the cause of rhythm disturbances is the dysfunction of the endocrine
system (hypo- and hyperfunction of the thyroid gland, Conn's syndrome, pheochromocytoma, menopause),
nervous, bronchopulmonary, and digestive systems
. Diseases affecting the entire body (anemia, infectious diseases and poisoning) can provoke arrhythmia.
Significant risk factors: abuse of alcohol, strong tea or coffee, any form of smoking, taking certain medications.
In addition, fasting, an unbalanced diet, food depletion of vitamins and microelements, dehydration, that is, any circumstances of disruption of water-electrolyte metabolism or acid-base status can lead to a failure of the normal electrical activity of the heart. Hereditary predisposition also matters.
However, in approximately 1/10 patients, even with high-quality examination, the cause of the arrhythmia cannot be determined (idiopathic arrhythmia).
Possible symptoms
Ectopic left and right atrial rhythms manifest themselves in the same way. A person often does not notice changes, and the symptoms of the underlying disease that caused the deviation come first. The only way to detect a violation is to take an electrocardiogram.
In other cases, the patient makes the following complaints:
- feeling of pulse unevenness and interruptions;
- heart sinking;
- dyspnea;
- weakness, decreased ability to work;
- pain or discomfort in the heart area.
In the presence of temporary jumping atrial complexes, symptoms usually either do not appear or are transient. According to my observations, they do not pose any particular danger and do not affect hemodynamics.
With prolonged attacks, the patient’s condition worsens, in addition to the main complaints, signs of circulatory disorders and cardialgia of ischemic origin appear.
Sometimes ectopic rhythm occurs due to dysfunction of the autonomic system:
- If the influence of the sympathetic department predominates, a person’s pulse quickens, the skin becomes cool and pale, and hypertension is observed. This condition is characterized by chills, headache, and often a panic attack.
- When vagotonia (parasympathetic) comes first, the frequency of contractions decreases, sweat is released, blood pressure decreases, and digestion is disrupted.
How to make a diagnosis
At the moment, the only objective way to detect ectopic atrial rhythm is an ECG. In the case when the impulses are temporary and interspersed with full myocardial contractions, Holter monitoring is used for diagnosis.
An electrocardiogram will reveal not only rhythm disturbances, but also indicate the localization of pathological impulses based on the state of the P wave. For clarity, you can give a table that shows how different types of ectopia manifest themselves:
| Localization in the atria | Leads | Signs (P wave) |
| Left | Right pectorals (V1-2) | two-phase, the first part is domed, the second is pointed, positive |
| Left pectorals (V5-6) | negative | |
| Standard (I, II) | smoothed out | |
| Right (photo 2) | I, II | positive |
| II, III | negative | |
| V1-6 and aVF | smoothed out | |
| Inferior atrial rhythm (Fig. 1) | I, III, aVF | negative |
Atrial rhythm in its pure form is not accompanied by a change in the electrical axis of the heart (EOS), and it is also not characterized by the appearance of deformation of the ventricular complexes.
As additional research methods and to identify the cause, I usually recommend:
- General and biochemical analysis of blood and urine. Laboratory results show the presence of inflammatory processes, problems in kidney function, and electrolyte imbalance.
- EchoCG. Ultrasound examination of the myocardium will help detect dilation of the heart, valvular insufficiency, and the presence of structural changes.
- In case of chest injury, an x-ray is taken.
Diagnosis of arrhythmia
Doctors have several methods for detecting arrhythmias, and each has its own characteristics.
- ECG
is a publicly available method that provides information about the patient’s rhythm at a given moment in time, allows you to record permanent disturbances and transient ones, if they are present at the time of registration. - Holter monitoring
ECG - 24-hour recording of an electrocardiogram. With this method, it is possible to establish all disturbances in the functioning of the heart within a day. - EchoCG
is an ultrasound examination of the heart. Makes it possible to visually determine the presence of arrhythmia and identify the organic cause of its occurrence. - Provocative tests
: orthostatic test, transesophageal electrophysiological study, intracardiac ECG recording) are capable of artificially inducing and recording arrhythmia when it cannot be detected during daily monitoring due to its transient nature.
Treatment
If a problem occurs in a healthy person under the influence of external factors, then it is transient and is eliminated when their influence ceases. In this case, no treatment is required. In the presence of a pathological condition, the main therapy should be aimed at eliminating the cause. To directly stop ectopic rhythm from the atria, the following are used:
- beta blockers for frequent contractions (Anaprilin);
- stimulants for bradycardia (Atropine);
- if there is a lack of potassium and magnesium, Panangin is used;
- sedatives for autonomic disorder (Motherwort, Persen);
- soothing herbal infusions.
In case of severe disorders with a pronounced decrease in the frequency of contractions and a high probability of developing a heart attack and other acute conditions, the issue of installing an artificial pacemaker is decided.
Classification of arrhythmia
Taking into account the place of origin of the electrical impulse and the specifics of its conduction from the pacemaker node to the ventricles, arrhythmias can be systematized as follows:
- violation of the generation of electrical impulses;
- conduction changes (blockades and additional conduction pathways);
- combined rhythm disturbances.
The first class of violations is:
- failures of automaticity of the source of excitation (sinus brady-, tachycardia, sinus arrhythmia, sick sinus syndrome, atrial asystole);
- ectopic bursts (ectopic rhythms, extrasystole, escape complexes, pacemaker migration, paroxysmal tachycardia, flutter, atrial fibrillation, ventricular fibrillation)
Heart blocks
divided according to the topography of the area where the movement of the electric wave slows down/interrupts. Their names correspond to the location. Consider sinoatrial, intraatrial, atrioventricular, and intraventricular blockades.
Congenital anomalies in the presence of additional conduction pathways serve as the basis for the occurrence of ventricular pre-exitation (pre-excitation) syndromes.
Combined
disorders are parasystole, atrioventricular dissociations, a combination of blockades with rhythm disturbances (Frederick's syndrome), etc.
According to forecast
distinguish between: non-dangerous arrhythmias, probably dangerous, life-threatening.
Based on this, disorders are differentiated into those requiring treatment and those subject only to observation over time.
Lifestyle restrictions
To prevent rhythm disturbances and the occurrence of ectopic atrial complexes, heart disease should be treated in time and the functioning of the autonomic nervous system should be restored. Following the usual rules will help improve the condition of existing deviations and prevent their development:
- Nutrition plays an important role. It must be balanced and complete. It is necessary to drink 1.5–2 liters of liquid per day, exclude animal fat from the menu, and consume as many vegetables and fruits as possible. You should eat small portions 4-5 times a day.
- Eliminate the possibility of overwork and normalize sleep.
- Breathe fresh air, go hiking, walk in a public garden or park.
- Exercise daily and go to the gym. Swimming, dancing, yoga will be beneficial.
- Studying with a psychologist and meditative practices help to develop stress resistance.
- Do not abuse alcohol, quit smoking.