Surely, each of us has come across the concepts of “blood serum” and “plasma” at least a couple of times in our lives. It is especially likely to hear such words in a hospital, clinic, or diagnostic laboratory. Do you know how they differ? Most likely, you will answer “no,” although this question was discussed in biology lessons N number of years ago... And maybe you even wrote an “excellent” test on this topic.
In the modern world, a lot of biological and medical information and terminology are popularized. We use words that, unfortunately, we do not always understand ourselves. It would be useful to broaden your horizons and still understand the above concepts.
Obtaining plasma and serum
Most often, transfusion now requires not so much whole blood as its components and plasma. It is extracted from whole blood using centrifugation, that is, separation of the liquid part from the formed elements by hardware. The blood cells are then returned to the donor. The duration of this procedure is forty minutes. In this case, blood loss is much less, and after two weeks you can donate plasma again, but no more than twelve times a year. Venous blood is taken in the morning on an empty stomach. In this case, it is worth taking into account factors that can affect the result of the analysis: emotional arousal, excessive physical activity, eating or drinking alcohol before the study, smoking, etc.
To exclude their influence, the following donor preparation conditions must be met:
- blood is taken after fifteen minutes of rest;
- the patient must sit (lying blood is taken from seriously ill people);
- Smoking, drinking alcohol and eating before the study are excluded.
Blood glucose
Blood glucose determination is one of the most widely used tests in clinical laboratory diagnostics. Glucose is determined in plasma, serum, and whole blood. According to the Laboratory Manual for the Diagnosis of Diabetes presented by the American Diabetes Association (2011), it is not recommended to measure serum glucose when diagnosing diabetes because the use of plasma allows samples to be quickly centrifuged to prevent glycolysis without waiting for clot formation.
Differences in glucose concentrations between whole blood and plasma require special attention when interpreting results. The concentration of glucose in plasma is higher than in whole blood, with the difference depending on the hematocrit value, therefore, using a constant factor to compare blood and plasma glucose levels may lead to erroneous results. According to WHO recommendations (2006), the standard method for determining glucose concentration should be the method for determining glucose in venous blood plasma. The concentration of glucose in the plasma of venous and capillary blood does not differ on an empty stomach, but 2 hours after a glucose load the differences are significant (Table).
| Glucose concentration, mmol/l | ||||
| Whole blood | Plasma | |||
| venous | capillary | venous | capillary | |
| Norm | ||||
| On an empty stomach | 3,3–5,5 | 3,3–5,5 | 4,0–6,1 | 4,0–6,1 |
| 2 hours after OGTT | <6,7 | <7,8 | <7,8 | <7,8 |
| Impaired glucose tolerance | ||||
| On an empty stomach | <6,1 | <6,1 | <7,0 | <7,0 |
| 2 hours after OGTT | >6,7<10,0 | >7,8<11,1 | >7,8<11,1 | >8,9<12,2 |
| SD | ||||
| On an empty stomach | >6,1 | >6,1 | >7,0 | >7,0 |
| 2 hours after OGTT | >10,0 | >11,1 | >11,1 | >12,2 |
The glucose level in a biological sample is significantly affected by its storage. When storing samples at room temperature, glycolysis results in a significant decrease in glucose content. To inhibit glycolysis processes and stabilize glucose levels, sodium fluoride (NaF) is added to the blood sample. When collecting a blood sample, according to a WHO expert report (2006), if immediate separation of plasma is not possible, the whole blood sample should be placed in a tube containing a glycolytic inhibitor, which should be kept on ice until plasma is isolated or analyzed.
Indications for the study
- Diagnostics and monitoring of diabetes;
- diseases of the endocrine system (pathology of the thyroid gland, adrenal glands, pituitary gland);
- liver diseases;
- obesity;
- pregnancy.
Features of sample collection and storage.
Before the study, it is necessary to exclude increased psycho-emotional and physical stress.
Preferably, venous blood plasma. The sample should be separated from the formed elements no later than 30 minutes after blood collection; hemolysis should be avoided.
Samples are stable for no more than 24 hours at 2–8 °C.
Research method.
Currently, enzymatic methods for determining glucose concentration - hexokinase and glucose oxidase - are most widely used in laboratory practice.
Increased values
- DM type 1 or 2;
- pregnancy diabetes;
- diseases of the endocrine system (acromegaly, pheochromocytoma, Cushing's syndrome, thyrotoxicosis, glucoganoma);
- hemachromatosis;
- acute and chronic pancreatitis;
- cardiogenic shock;
- chronic liver and kidney diseases;
- physical exercise, strong emotional stress, stress.
Reduced values
- Overdose of insulin or hypoglycemic drugs in patients with diabetes;
- diseases of the pancreas (hyperplasia, tumors) causing disruption of insulin synthesis;
- deficiency of hormones with counter-insular effects;
- glycogenosis;
- oncological diseases;
- severe liver failure, liver damage caused by poisoning;
- gastrointestinal diseases that interfere with the absorption of carbohydrates.
- alcoholism;
- intense physical activity, feverish conditions.
How is blood plasma different from serum?
Plasma is a yellowish, cloudy substance that is part of the blood. It contains basic information about the individual's health status. It helps to identify hormonal imbalances and problems in the functioning of individual organs and systems. Among the disadvantages of plasma, experts note its short shelf life, after which it becomes unsuitable for study and use. Serum is plasma without fibrinogen, which increases its lifespan. The serum can be used to obtain various drugs that have medicinal properties. It helps conduct large-scale studies of the capabilities of the human body, testing the reaction of blood cells to various types of pathogenic microorganisms.
The difference between plasma and serum is as follows:
- Plasma is the entire component of blood, while serum is only a part.
- Plasma contains fibrinogen, a protein responsible for blood clotting.
- Plasma is always yellowish, and serum may have a reddish tint due to damaged red blood cells.
- Plasma coagulates under the influence of the enzyme coagulase, and serum is resistant to this process.
The differences between these two components of blood are so enormous that it is impossible to consider them identical.
What is the difference?
The main difference between Plasma and Serum is that Plasma contains a blood clotting agent whereas Serum does not contain blood clotting factors. Plasma is the clear and yellowish liquid part of the blood, whereas Serum is the liquid part of the blood after coagulation.
Contrary to popular belief, serum and blood plasma are not the same thing, and therefore the terms cannot be used interchangeably. In this article, we'll look at what plasma and serum are and the main differences between them.
Content
- Overview and main differences
- What is Plasma
- What is Serum
- Separation of Blood Plasma and Serum
- What is the difference between Plasma and Serum
- Conclusion
What is Plasma
Plasma is the liquid part of blood, which is 90% water and makes up about 55% of the total blood volume. Its main function is to transport proteins, nutrients, hormones and antibodies, among other things, throughout the body. As it spreads throughout the body, cells also release their waste into the plasma.
Blood composition
In addition to water, plasma also contains albumin, fibrinogen, globulin, hormones, nutrients, amino acids, and nitrogenous waste products. Typically, plasma helps regulate body temperature and blood pressure. Plasma has a long shelf life and can last up to a year.
What is Serum
Simply put, serum is plasma without clotting factors and blood cells. During the process of removing clotting factors (achieved by centrifugation), the protein fibrinogen is converted into fibrin. Fibrin is an insoluble protein that is used to repair damaged tissue by forming a clot in a wound that impedes blood flow.
Obtaining blood serum
It is noteworthy that the whey has a short shelf life and can be stored for only a few months. It is used to identify problems related to cholesterol, blood sugar and blood pressure.
Separation of Blood Plasma and Serum
The composition of serum and plasma can be separated by centrifugation. Notably, each component can be separated due to its different size, weight and density. EDTA Heparin, which is an anticoagulant, is needed to separate blood components such as white blood cells and red blood cells from the plasma. However, the whey separation process is relatively complex.
What is blood plasma?
Blood consists of plasma and cells (red blood cells, platelets and white blood cells). If we imagine the entire volume of our blood as a percentage, we get the following picture: plasma takes up from 55 to 60% of the total blood composition, and cells – from 40 to 45%.
Thus, plasma is one of the main components that make up blood. It looks like a homogeneous yellowish liquid. It is often cloudy, but can also be completely transparent. This characteristic of plasma is influenced by factors such as, for example, the amount of bile pigment or frequent consumption of fatty foods.
Compound
Most of the plasma is water, its amount is approximately 92% of the total volume.
In addition to water, it includes the following substances:
- proteins;
- glucose;
- amino acids;
- fat and fat-like substances;
- hormones;
- enzymes;
- minerals (chlorine, sodium ions).
About 8% of the volume is proteins, which are the main part of plasma. It contains several types of proteins, the main ones being:
- albumins – 4-5%;
- globulins – about 3%;
- fibrinogen (belongs to globulins) – about 0.4%.
Albumen
Albumin is the main plasma protein. It has a low molecular weight. Content in plasma is more than 50% of all proteins. Albumin is formed in the liver.
Protein functions:
- perform a transport function - transport fatty acids, hormones, ions, bilirubin, medications;
- take part in metabolism;
- regulate oncotic pressure;
- participate in protein synthesis;
- reserve amino acids;
- deliver medications.
A change in the level of this protein in plasma is an additional diagnostic sign. The condition of the liver is determined by the concentration of albumin, since many chronic diseases of this organ are characterized by its decrease.
Globulins
The remaining plasma proteins are classified as globulins, which are large in molecular weight. They are produced in the liver and in the organs of the immune system.
Main types:
- alpha globulins,
- beta globulins,
- gamma globulins.
- Alpha globulins bind bilirubin and thyroxine, activate the production of proteins, transport hormones, lipids, vitamins, and microelements.
- Beta globulins bind cholesterol, iron, vitamins, transport steroid hormones, phospholipids, sterols, zinc and iron cations.
- Gamma globulins bind histamine and participate in immunological reactions, which is why they are called antibodies, or immunoglobulins.
There are five classes of immunoglobulins: IgG, IgM, IgA, IgD, IgE. Produced in the spleen, liver, lymph nodes, and bone marrow. They differ from each other in biological properties and structure. They have different abilities to bind antigens, activate immune proteins, have different avidity (rate of binding to antigen and strength) and ability to pass through the placenta. Approximately 80% of all immunoglobulins are IgG, which have high avidity and are the only ones that can cross the placenta. IgM is synthesized first in the fetus. They are also the first to appear in the blood serum after most vaccinations. They have high avidity.
Fibrinogen is a soluble protein that is produced in the liver. Under the influence of thrombin, it is converted into insoluble fibrin, due to which a blood clot is formed at the site of vessel damage.
Other proteins
In addition to the above, plasma also contains other proteins:
- complement (immune proteins);
- transferrin;
- thyroxine-binding globulin;
- prothrombin;
- C-reactive protein;
- haptoglobin.
Non-protein components
In addition, blood plasma includes non-protein substances:
- organic nitrogen-containing: amino acid nitrogen, urea nitrogen, low molecular weight peptides, creatine, creatinine, indican. Bilirubin;
- organic nitrogen-free: carbohydrates, lipids, glucose, lactate, cholesterol, ketones, pyruvic acid, minerals;
- inorganic: sodium, calcium, magnesium, potassium cations, chlorine anions, iodine.
The ions in the plasma regulate the pH balance and maintain the normal state of cells.
Laboratory diagnosis of reproductive system disorders (part 2)
Nechaev V.N., Ph.D.
Determination of prolactin levels
The first stage of laboratory examination of persons of both sexes suffering from reproductive disorders, according to WHO recommendations, is to measure the concentration of prolactin (milk hormone) in the blood serum (plasma). Prolactin does not directly affect the functional activity of the gonads, while at the same time the level of prolactin in the blood clearly correlates with the state of the hypothalamus and adenohypophysis . Prolactin regulates milk secretion during lactation. Prolactin is a hormone antagonist of FSH and LH , and with increased production of prolactin, the hormonal function of the ovaries is disrupted and a hyperprolactinemic form of infertility occurs. Physiological hyperprolactinemia is observed in women who are breastfeeding. In non-breastfeeding women, elevated prolactin levels may be associated with certain medications, a tumor of the pituitary gland, or a malfunction of the pituitary gland. One of the manifestations of hyperprolactinemia is the release of colostrum or milk from the mammary glands, especially in nulliparous women. Pathological changes in the body, with increased or decreased levels of prolactin, are presented in Table 1.
Table 1. Pathological changes in the body with increased or decreased levels of prolactin
| Increased concentration | Decreased concentration |
| Prolactinoma | Acute porphyria |
| Neurogenic and psychiatric disorders, menstrual disorders | Acute and chronic physical and mental stress situations (depression, surgery, painful periods) |
| Acromegaly | Hypoglycemia |
| Hirsutism (hyperandrogenism) |
Prolactin is found in the blood serum in three different forms. The biologically and immunologically active monomeric form predominates (approximately 80%), 5-20% is present as a dimeric inactive form and 0.5-5% is present as a tetrameric, also inactive form. Table 2 presents reference values for the concentrations of the monomeric form (biologically active) of prolactin.
Table 2. Reference values for serum prolactin concentrations
| Age | Prolactin, mIU/l |
| Children under 10 years old | 91 — 526 |
| Women | 61 — 512 |
| pregnancy 12 weeks | 500 — 2000 |
| pregnancy 12-28 weeks | 2000 — 6000 |
| pregnancy 29-40 weeks | 4000 — 10000 |
| postmenopausal (over 45 years old) | 64 – 354 |
| Men | 58 — 475 |
Indications for determination:
Women of childbearing period:
- Menstrual irregularities and amenorrhea
- Infertility
- Lactation disorders
- Galactorrhea
- Pituitary hyperfunction syndrome
- Pituitary insufficiency
- Replacement therapy after removal of a pituitary tumor
Men:
- Testicular failure
- Azoospermia, oligospermia
- Galactorrhea
- Pituitary hyperfunction syndrome
- Pituitary insufficiency
- Replacement therapy after removal of a pituitary tumor
Preparing samples for analysis
Prolactin has a fairly pronounced circadian rhythm with the maximum release of the hormone during night sleep. It is recommended to take blood sampling in the morning (8-10 hours), in the early follicular phase of the cycle (in women with a regular cycle) and in a calm environment. To exclude an accidental increase in prolactin levels in response to stress (blood drawing), a 2-3-fold study is desirable.
Material for research:
- blood serum
- heparinized blood plasma
FSH and LH are the “main” hormones of reproduction
If determining the level of prolactin in the blood provides information about the functional state of the hypothalamic-pituitary complex as a whole, then to assess the activity of the reproductive system, measuring the content of gonadotropic hormones in the blood - FSH and LH - is used.
It is these hormones that ensure the growth and development of follicles (FSH) and stimulate the synthesis of sex hormones in the gonads (LH). The secretion of LH and FSH is, in turn, under the control of gonadal sex hormones (negative feedback mechanism). An increase in the level of sex hormones, primarily estradiol, in the blood is accompanied by inhibition of the secretion of gonadotropins (and vice versa). FSH secretion is additionally regulated by inhibin, a polypeptide synthesized by the gonads. During the preovulatory period, the mature dominant follicle secretes large amounts of estradiol into the blood, under the influence of which an ovulatory release of LH and FSH occurs (a positive feedback phenomenon). This rise (ovulatory peak) lasts very briefly, 1-2 days. The intensity of gonadotropin secretion during the periovulatory period determines the future functional activity of the corpus luteum. The daily (circadian) rhythm of secretion of LH and FSH in adults is not pronounced, unlike in adolescents, while the circhoral (hourly) rhythm of secretion is very characteristic of gonadotropins.
Modern ELISA test systems for the determination of FSH and LH are based on the use of monoclonal antibodies that do not cross-react with the closely related hormones TSH and hCG.
Table 3. Reference values for FSH and LH concentrations in blood serum.
| Age | Cycle phase | FSH, IU/l | LH, IU/l |
| Children under 10 years old | < 3 | < 1 | |
| Men | 0,8 – 13 | 0,5 – 10 | |
| Women | Folliculin phase | 3 – 12 | 05 – 18 |
| Ovulatory peak | 6 – 25 | 14-80 | |
| Luteal phase | 2 – 12 | 0,5 – 18 | |
| Menopause | 30 – 120 | 10 – 70 |
Preparing samples for analysis
Gonadotropin levels do not follow a circadian rhythm and there is no need to draw blood in a fasting state. It should be borne in mind that with a preserved menstrual cycle, a single determination of gonadotropins can be performed only in the early follicular phase (days 6-8 of the cycle). More clear results are obtained by taking 2-3 blood samples with an interval of 30-40 minutes and then combining the resulting sera. LH and FSH cannot be determined once in a blood sample taken in the middle of the cycle to detect ovulation. The timing of ovulation for cycles of different lengths is different (about 14 days before the start of the expected menstruation) and can shift by 1-2 days from the expected ones. In this regard, the results of a single determination of gonadotropins on the 13-14th days of the cycle in most cases provide false information about the nature of the cycle. The pulsatile nature of secretion at intervals of 1-2 hours is especially characteristic of PH, so the results of single tests should be considered approximate. Serum or plasma samples after clotting and/or red blood cell separation are stable for a time sufficient to allow samples to be mailed. Frozen samples can be stored for long periods of time.
It is not recommended to use hemolyzed, lipemic or icteric samples as this may affect the test results.
Blood must be collected with a wide bore needle, by gravity flow, or with slight negative pressure from the syringe piston.
Material for research:
- blood serum
- heparinized blood plasma
Determination of sex hormones
There is no doubt that for a complete examination of the state of the reproductive system, it is necessary to have ELISA test systems for determining sex hormones (estradiol, testosterone, progesterone) in blood serum. If the synthesis of sex hormones in the gonads is sharply reduced, then, through a negative feedback mechanism, the secretion of gonadotropins increases sharply so that the diagnosis of lack of ovarian function does not cause difficulties.
In the diagnostic algorithm of examination for suspected endocrine infertility, the key is to determine the concentrations of LH, FSH, estradiol and testosterone.
Methods for determining these hormones today are predominantly based on enzyme-linked immunosorbent or immunofluorescent technology, which ensures their widespread use.
Estradiol
Estradiol is the main estrogenic steroid hormone. Catabolism in the liver leads to the transformation of estradiol into estriol or into glucuronides and sulfates excreted in the urine.
In women, estradiol is synthesized and secreted in the ovaries , in the membrane and granulosa cells of the follicles. It stimulates the development of the first phase of the ovarian cycle, causing an increase in uterine muscle protein and endometrial hyperplasia. At the pituitary level, it also acts on the secretion of LH, FSH . During the first phase of the cycle, an increasing increase in estradiol leads to massive secretion of LH , which “triggers ovulation.” During pregnancy, the concentration of estradiol increases. Plasma estradiol analysis ovulation induction and ovarian stimulation . estradiol synthesis and its concentration at the end of stimulation reflects the number and quality of maturing follicles.
Table 4. Reference values for estradiol concentrations in blood serum.
| Age | Concentration (pg/ml) | |
| Children under 11 years old | < 15 | |
| Men | 10-50 | |
| Women | Folliculin phase | 20 — 350 |
| Ovulation phase | 150 — 750 | |
| Luteal phase | 30 — 450 | |
| Menopause | < 20 |
Indications for determination:
women:
- control of stimulated ovulation,
- assessment of ovarian function,
- menstrual irregularities,
- amenorrhea of hypothalamic origin,
- estrogen-producing tumors
- monitoring of infertility treatment,
- osteoporosis;
men:
- gynecomastia,
children:
- monitoring the progress of puberty.
Table 5. Diseases and conditions in which the concentration of estradiol in the blood serum may change
| Increased concentration | Decreased concentration |
| Gynecomastia | Turner syndrome |
| Uterine bleeding during menopause | Primary and secondary hypogonadism |
| Estrogen-producing tumors | |
| Cirrhosis of the liver | |
| Feminization in children | |
| The use of clomiphene, estrogens, gonadotropins |
Progesterone
Progesterone is one of the main steroid hormones. It is secreted in small quantities by the cells of the corpus luteum of the ovaries in the luteal phase of the menstrual cycle. It acts on the endometrium together with estradiol , as a result of which the menstrual cycle passes from the proliferative phase to the secretory phase. Progesterone levels reach their maximum on the 5th – 7th day after ovulation . If fertilization does not occur, progesterone levels decrease, and conversely, if fertilization does occur, the corpus luteum continues to secrete large amounts of progesterone until 12 weeks of pregnancy . the placenta comes into play , which becomes the main site of hormone production. Progesterone is also secreted in small quantities by the adrenal cortex and testes and is an intermediate in the synthesis of androgens.
In the blood, progesterone is found both in free and bound to protein carriers (albumin and transcortin) states. The half-life of the hormone is several minutes, two-thirds of progesterone is metabolized in the liver and secreted into the urine as free pregnanediol, pregnanediol glucuronide and pregnanediol sulfate.
Table 6. Reference values for progesterone concentration in blood serum
| Age | Concentration (ng/ml) | Concentration (nmol/l) |
| Men | 0,13 — 1,26 | 0,4 — 4,0 |
| Women | ||
| follicular phase | 0,06 — 1,26 | 0,2 — 4,0 |
| ovulatory peak | 0,08 — 1,2 | 0,25 — 3,8 |
| luteal phase | 2,5 — 25 | 8 — 78 |
| postmenopause | 0,06 — 1,6 | 0,2 — 5 |
| Pregnancy: weeks | ||
| 18 – 21 | 53 – 76 | |
| 22 – 25 | 60 – 86 | |
| 26 – 29 | 71 – 133 | |
| 30-33 | 86 – 142 | |
| 34 – 37 | 104 – 175 | |
| 38 – 41 | 117 – 187 |
Indications for determination:
women:
- ovulation disorders,
- absence of ovulation with or without oligomenorrhea,
- insufficiency of corpus luteum function;
- accurate determination of ovulation
- induction of ovulation by human menopausal gonadotropin or clomiphene (both in the presence of hCG and without it);
- confirmation of ovulation (determination in the second half of the cycle);
- monitoring the progress of ovulation in women who have undergone spontaneous abortion;
men and children:
- defect in steroid biosynthesis.
Progesterone causes an increase in basal body temperature. In case of diagnosis of insufficiency of corpus luteum function, samples are taken 3 times (each after 3-4 days of the previous collection). In at least 2 cases, the progesterone concentration should exceed 10 μg/ml.
Testosterone
In women, testosterone is formed in the adrenal cortex and ovaries in a 1:1 ratio and serves as a substrate for the formation of estrogens, and also stimulates the preovulatory release of LH. Testosterone levels do not change with age in women. Normal testosterone levels in women are 0 – 0.9 ng/ml.
Indications for determination:
- Klinefelter syndrome and other chromosomal diseases;
- hypopituitarism;
- enzymatic disorders of androgen synthesis;
- hirsutism and virilization of women;
- most androgen-producing tumors of the ovaries and kidneys.
In women, it is also necessary to determine the level of DHEA, a sulfate that has a similar effect to testosterone (in men it is an auxiliary agent in the study of testosterone).
Material for research:
- blood serum of women on days 3–7 of the menstrual cycle, preferably between 8 and 10 am.
Steroid binding globulin (SBG) in blood serum
SSG is a protein that binds and transports testosterone and estradiol. In addition to its transport function, DES protects testosterone and estradiol from metabolic activity along the way from the gland secreting them to the target organ, and forms a kind of hormone depot in the body. SSG is an acidic glycoprotein with a molecular weight of 45,000 daltons. Violation of the synthesis of dry hormones leads to disruption of the delivery of hormones to target organs and the performance of their functional activity. The concentration of dry hormones in the blood serum is increased by estrogens and oral contraceptives, and decreased by androgens, T4, and TSH.
Table 7. Reference values for dry serum concentrations
| Age | Concentration nmol/ml | Concentration mg/l |
| Men | 14,9 — 103 | 1 — 12 |
| Women | 18,6 — 117 | 31 — 15 |
| during pregnancy – 30 -120 |
Precursors for the biosynthesis of androgens and estrogens
17α-Hydroxyprogesterone
17a-Hydroxyprogesterone (17OH-P) is an intermediate steroid in the biosynthesis of glucocorticoids, androgens and estrogens, which is synthesized from progesterone and 17a-hydroxypregnenolone. Secreted by the adrenal cortex, ovaries and testes, it circulates in the blood, both in free and bound, like progesterone, with two proteins - albumin and transcortin. The half-life of 17OH-P is several minutes. It is metabolized by the liver and excreted in the urine as pregnanetriol.
17OH-P is produced in small quantities by the ovaries during the follicular phase, then its concentration increases and remains constant during the luteal phase. If fertilization does not occur, the level of 17OH-P decreases. When a fertilized egg is implanted, the corpus luteum continues to secrete 17OH-P.
Analysis of 17OH-P is very important for the diagnosis of congenital adrenal hyperplasia and detection of enzyme deficiency responsible for the occurrence of this disease.
The level of 17OH-P in the blood is particularly indicative and is critical in the diagnosis of 21-hydroxylase deficiency in newborns.
In adulthood, with partial or late-onset enzyme deficiency, the basic level of 17OH-P activity may be normal or increased
Table 8. Reference values for 17OH-P concentration in blood serum
| Gender, physiological state | Concentration (ng/ml) | Concentration (nmol/l) |
| Children, puberty: | ||
| Boys | 01 — 2,7 | |
| Girls | 0,1 — 2,7 | |
| Men | 0,04 — 3,90 | 0,12 — 11,8 |
| Women | ||
| follicular phase | 0,07 — 1,09 | 0,4 — 2,10 |
| luteal phase | 0,04 — 3,30 | 1.0 — 8,7 |
| postmenopause | 0,04 — 2,38 | <2,0 |
Indications for determination:
- congenital enzyme deficiency responsible for the occurrence of adrenal hyperplasia;
- diseases associated with 21-hydroxylase deficiency in newborns (high levels of 17OH-P);
- partially or late manifested deficiency of 21-hydroxylase (normal or high level of 17OH-P);
- differential diagnosis of infertility.
Material for research:
- blood serum;
- blood plasma with the addition of heparin.
Dehydroepiandrosterone
Dehydroepiandrosterone (DHEA) is one of the most important androgens (more precisely, their precursor), synthesized by the adrenal cortex and gonads from 17OH-P. It is catabolized into the virilizing androgens: androstenediol, testosterone and dihydrotestosterone.
Most DHEA is modified by adding a sulfate to (DHEA-S), which is biologically inactive, but removing the sulfate group restores the activity of DHEA. DHEA is actually a prohormone, has a shorter half-life and a higher metabolic rate, due to which its concentration in the blood is 300 times lower than the level of DHEA-S.
DHEA is characterized by a circadian level of secretion with maximum release of the hormone in the morning hours. There are no significant changes in its concentration during the menstrual cycle. Unlike testosterone, DHEA in the circulation is not associated with DES, so changes in the concentration of binding proteins do not affect its levels.
Table 9. Reference values for DHEA concentrations in blood serum
| Age | Concentration (ng/ml) | Concentration (nmol/ml) |
| Blood from the umbilical cord | 30-150 | 1,0-5,2 |
| Newborns. 1-7 days | 20-290 | 0,7-10,1 |
| Children: | ||
| 1-12 months | 6-68 | 0,2-2,4 |
| 1-10 years | 8,0-50 | 0,3-1,7 |
| 10-17 years | 8-240 | 0,3-8,4 |
| Adults: | ||
| Men | 75-205 | 2,6-9,6 |
| Women | 85-275 | 3,0-9,6 |
Indications for determination:
- hirsutism;
- virilization;
- delayed puberty
Material for research:
- blood serum;
- blood plasma with the addition of heparin.
Dehydroepiandrosterone sulfate
DHEA-S is synthesized in the adrenal glands (95%) and ovaries (5%), excreted in the urine and constitutes the main fraction of 17a-ketosteroids. Determination of DHEA-S concentration in blood serum replaces the study of 17a-ketosteroids in urine.
DHEA-S is secreted at a rate of 10-20 mg/24 hours (35-70 µmol/24 hours) in men and 3.5-10 mg/24 hours (12-35 µmol/24 hours) in women, and without circadian rhythm. It does not bind to specific plasma proteins and, therefore, their concentration does not affect the level of DHEA-S. However, DHEA-S binds to serum albumin.
In addition to DHEA-S, DHEA is present in the circulating blood, accounting for ¼ and ½ the rate of DHEA-S secretion in men and women, respectively. Due to its high concentration of DHEA-S in the blood, long half-life and high stability, and because its source is primarily from the adrenal glands, DHEA-S is an excellent indicator of androgen secretion.
If women have elevated testosterone levels, then by determining the concentration of DHEA-S, it is possible to determine whether this is due to impaired adrenal function or ovarian disease.
Table 10. Reference values for DHEA-S concentrations in blood serum
| Age | Concentration (µg/ml) | Concentration (µmol/l) |
| Newborns. | 1,7 — 3,6 | 4,4 — 9,4 |
| Children: | ||
| 6-9 years | 0,025 — 1,45 | 0,07 — 3,9 |
| 10-11 years | 0,15 — 1,87 | 0,4 — 6,0 |
| 12-17 years old | 0,20 — 5,55 | 0,5 — 15.0 |
| Adults: | ||
| Men: | ||
| 18-30 years old | 1,26 — 6,19 | 3,4 — 16,7 |
| 31-59 years old | 1,0 — 3,2 | 2,7 — 11,1 |
| Women: | ||
| 18-30 years old | 0,6 — 4,5 | 1,62 — 12,1 |
| 31-39 | 0,5 — 4,1 | 1,35 — 11,1 |
| Pregnancy period | 0,2 — 1,2 | 0,5 — 3,1 |
| Premenopausal period | 0,8 — 3,9 | 2,1 — 10,1 |
| Postmenopausal period | 0,1 — 0,6 | 0,32 — 1,6 |
Conversion factors:
- 1 ng/100ml = 28.8 nmol/l;
- 1 nmol/l = 2.6 ng/ml
- 1 ng/ml = 368.46 µmol/l
Indications for determination:
- adrenal tumors;
- differential diagnosis of ovarian diseases;
- osteoporosis;
- delayed puberty.
Material for research:
- blood serum;
- blood plasma with the addition of heparin.
Autoimmune diseases of the reproductive system
Physiological depletion of ovarian follicles in women occurs at the age of 45-55 years. Cessation of ovarian function before age 40 indicates a condition known as premature ovarian failure. The consequence of this disease is infertility. In some cases, the cause of this may be an autoimmune process associated with the formation of antibodies to ovarian sex hormones.
In some cases, the development of infertility in men is due to the presence of specific antibodies in the serum or seminal plasma.
Ovarian antibodies in blood serum
Normally, a woman’s blood serum contains no ovarian antibodies. Ovarian antibodies (to ovarian antigens) have been found in women with premature menopause, infertility, and in vitro fertilization. These antibodies can be produced by Leydig cells, granucile cells of the ovary and cells of the placenta. To determine antibodies to sex hormones, the method of indirect immunofluorescence and ELISA is used. The ELISA method allows you to determine both total and antibodies to various classes of immunoglobulins (IgG, IgM, IgA). Autoimmune antibodies can be detected in the blood of women many years before the development of clinical manifestations of premature ovarian failure.
In addition to ovarian antibodies, the ELISA method allows you to detect antibodies to the transparent membrane of the oocyte - total and antibodies to classes (IgG, IgM, IgA), which have the same diagnostic value as ovarian antibodies.
In women, a clear correlation between serum antibody concentrations and fertility prognosis is usually not possible.
Antisperm antibodies in blood serum
Normally, a woman’s blood serum contains no antisperm antibodies. In men, antisperm antibodies are formed as a result of an autoimmune reaction to the sperm epithelium. The reason for the development of such a reaction may be testicular trauma, bacterial and viral infections, or surgical operations on the testicle. To determine antisperm antibodies, the ELISA method is currently used, which is highly sensitive and specific, and also allows the quantitative determination of antibodies of various classes of immunoglobulins (IgG, IgM, IgA), which makes it possible to assess the severity and severity of the autoimmune process. In addition, in men, the concentration of antisperm antibodies correlates with the restoration of fertilization ability.
Women do not normally produce antibodies against sperm antitags, but various etiological factors (infections, autoimmune diseases) can lead to loss of immunological tolerance. If antisperm antibodies are present in a woman’s blood, then the processes of trophoblast formation, growth and formation of the placenta, and implantation are disrupted. And this leads to termination of pregnancy, gestosis, delayed fetal development, and fetoplacental insufficiency.
Testing for antisperm antibodies is recommended for all couples with unexplained infertility.
Chorionic gonadotropin (hCG) in blood serum
HCG is a glycoprotein with a molecular weight of approximately 46,000, consisting of two subunits - alpha and beta. An increased level of hCG in the blood serum is detected already on the 8-12th day after conception. During the first trimester of pregnancy, the concentration of hCG increases rapidly, doubling every 2-3 days. The maximum concentration occurs in the 7-10th weeks of pregnancy, after which the concentration of hCG begins to decrease and remains more or less stable during the second half of pregnancy.
Table 11 shows the concentrations of hCG in a woman’s blood serum during the dynamics of physiological pregnancy.
Table 11. Concentrations of hCG in a woman’s blood serum in the dynamics of physiological pregnancy
| Gestation period, week | Median hCG concentration, IU/l | Reference values hCG, IU/l |
| 1-2 | 150 | 50-300 |
| 3-4 | 2000 | 1500-5000 |
| 4-5 | 20 000 | 10 000-30 000 |
| 5-6 | 50 000 | 20 000-100 000 |
| 6-7 | 100 000 | 50 000-200 000 |
| 7-8 | 70 000 | 20 000-200 000 |
| 8-9 | 65 000 | 20 000-100 000 |
| 9-10 | 60 000 | 20 000-95 000 |
| 10-11 | 55 000 | 20 000-95 000 |
| 11-12 | 45 000 | 20 000-90 000 |
| 13-14 | 35 000 | 15 000-60 000 |
| 15-25 | 22 000 | 10 000-35 000 |
| 26-37 | 28 000 | 10 000-60 000 |
In the second trimester of pregnancy, if the fetus has Down syndrome, the concentration of hCG in the blood is increased, the concentration of AFP (see below) is decreased. Taking this into account, ELISA testing for AFP and hCG are used as a method of mass prenatal screening in the second trimester of pregnancy. The median hCG concentration values for screening congenital malformations of the fetus in the second and third trimester are shown in Table 12.
Table 12. Median hCG concentration values for screening congenital malformations of the fetus in the 2nd and 3rd trimester
| Gestation period, week | Median concentrations for hCG, IU/l |
| 14 | 63 900 |
| 14-15 | 58 200 |
| 15 | 43 600 |
| 15-16 | 38 090 |
| 16 | 37 000 |
| 16-17 | 35 000 |
| 17 | 34 600 |
| 17-18 | 34 000 |
| 18 | 33 400 |
| 18-19 | 29 100 |
| 19 | 26 800 |
| 19-20 | 23 600 |
| 20 | 20 400 |
| 20-21 | 20 000 |
| 21 | 19 500 |
Alpha Fetoprotein (AFP) in serum
AFP is a glycoprotein with a molecular weight of approximately 65,000 kDa, secreted by the fetal liver and yolk sac. AFP in the fetus is the main serum protein; in adults, the content of AFP in the blood serum is insignificant. In the second trimester of pregnancy, if the fetus has Down syndrome, the concentration of AFP is reduced, and the concentration of hCG in the blood is increased. Taking this into account, ELISA testing for AFP and hCG is used as a method of mass prenatal examination of pregnant women, with which it is possible to identify a high-risk group based on the presence of malformations or Down syndrome in the fetus. The median values of AFP concentration in blood serum for screening of congenital malformations of the fetus in the second trimester are shown in Table 13.
Table 13. Median AFP concentrations for screening congenital malformations of the fetus in the second trimester
| Gestation period, week | Median AFP concentration, IU/ml |
| 15 | 32 |
| 16 | 34 |
| 17 | 36 |
| 18 | 40 |
| 19 | 45 |
| 20 | 49 |
Free estriol in blood serum
Estriol is the main steroid hormone synthesized by the placenta. The content of estriol in the blood of a pregnant woman correlates with the activity of the fetal adrenal glands. Estriol penetrates into the bloodstream of a pregnant woman, where its concentration in the free state can be determined. During a normally developing pregnancy, estriol synthesis increases in accordance with increasing gestational age and fetal growth (Table 14).
Table 14. Concentrations of estriol in a woman’s blood serum during physiological pregnancy
| Gestation period, week | Median estriol concentration, nmol/l | Reference values of estriol, nmol/l |
| 6-7 | 1,2 | 0,6-2,5 |
| 8-9 | 1,6 | 0,8-3,5 |
| 10-12 | 4 | 2,3-8,5 |
| 13-14 | 8 | 5,7-15 |
| 15-16 | 10 | 5,4-21 |
| 17-18 | 12 | 6,6-25 |
| 19-20 | 15 | 7,5-28 |
| 21-22 | 24 | 12-41 |
| 23-24 | 28 | 18,2-51 |
| 25-26 | 31 | 20-60 |
| 27-28 | 32 | 21-63,5 |
| 29-30 | 35 | 20-68 |
| 31-32 | 38 | 19,5-70 |
| 33-34 | 43 | 23-81 |
| 35-36 | 52 | 25-101 |
| 37-38 | 64 | 30-112 |
| 39-40 | 65 | 35-111 |
In case of pathology (severe developmental defects of the central nervous system in the fetus, congenital heart defects, Down syndrome, fetal growth restriction, fetal adrenal hypoplasia, intrauterine fetal death), the concentration of free stradiol in the blood serum of the pregnant woman decreases.
The median values of free estradiol concentration in blood serum for screening of congenital malformations in the second trimester of pregnancy are shown in Table 15.
Table 15. Median concentrations of free estradiol in blood serum for screening of congenital malformations in the second trimester of pregnancy
| Gestation period, week | Median concentrations of free estradiol, nmol/l |
| 15 | 4,3 |
| 16 | 4,8 |
| 17 | 5.5 |
| 18 | 6,4 |
| 19 | 7,1 |
| 20 | 8,2 |
In Down and Edwards syndrome, the concentration of free estradiol is usually 0.7 MoM.
In conclusion, we note that the widespread introduction of full-fledged ELISA diagnostics into clinical practice will significantly increase the efficiency of diagnosis and treatment of patients with disorders of the reproductive system.
Plasma donation
In addition to whole blood donation, plasma donation is also a very common procedure. It is often transfused in cases of violation of the integrity of the skin (burns, injuries), and human plasma is also needed for the manufacture of certain medications.
There is a special medical term for the plasma donation procedure – “plasmapheresis”. The whole process is completely safe and can be manual, but most often it is automated. Automatic plasma collection occurs as follows. First, the future donor undergoes all the necessary tests. After permission for plasmapheresis is received, he comes to a special medical blood donation center to undergo this procedure.
Before donating blood, blood tests are taken from the future donor again, and then he is offered to drink a glass of sweet tea to maintain the necessary fluid balance. Then the donor goes to the room designated for blood donation and sits in a comfortable chair. Using a special apparatus, 450 ml of blood is taken from him, which is then divided into components (plasma and blood cells). The plasma is placed in storage, and the human blood cells, along with saline, are returned back. The entire procedure takes place within 30-40 minutes.
What is blood serum?
Serum is plasma without fibrinogen (the liquid part remaining after blood clotting). It is presented in the form of a yellowish substance (the tint is given by bilirubin). Due to any disturbances in the normal metabolism of pigments, the quantitative concentration of this element will certainly change. And the substance will become transparent.
If you take a serum test from a person who has just eaten, it will be somewhat cloudy. In this case, it contains fats of animal origin. Therefore, doctors recommend donating blood on an empty stomach.
Serum can contain a huge amount of antibodies. And this is quite natural, since it performs an immune function, helping the human body fight infections, parasites, bacteria, fungi and other pathological agents.
The study of serum and blood plasma helps in identifying pathologies that threaten the patient’s health.
This biomaterial is used for:
- Biochemical research.
- Blood group test.
- Detection of infectious diseases.
- Determining the effectiveness of vaccination.
The difference between serum and blood plasma is that it is used as a component (or rather a producer) for the manufacture of drugs. Their help is needed in the fight against infectious diseases.
Difference Between Serum and Plasma
Serum and plasma are two derivatives of blood that lack blood cells such as red blood cells, white blood cells and platelets. Both contain proteins, drugs, hormones, toxins and electrolytes.
Both serum and plasma have therapeutic and diagnostic uses. They can be separated from the blood by centrifugation, which removes the cellular portion of the blood. Anticoagulants are added to the blood after a transfusion to prevent blood clotting.
The serum is amber in color and the plasma is straw in color.
The main difference between serum and plasma is that serum is a protein-rich liquid that is released when blood coagulates while plasma is the liquid component of blood that keeps the blood cells in whole blood in suspension.
This article looks at,
1. What is serum - definition, composition, properties 2. What is plasma - definition, composition, properties 3. What is the difference between serum and plasma
What is serum
Serum is a watery, amber-colored portion of animal blood that remains after the blood has clotted. Consequently, the serum lacks blood cells such as red blood cells, white blood cells and platelets. It also lacks blood clotting factors such as fibrinogen.
But serum contains all the proteins such as albumin and globulin, which are not involved in the blood clotting process. It also contains antibodies, antigens, electrolytes, hormones, drugs and microorganisms. Serology is the study of serum. Serum is separated from the blood by centrifugation, which removes the cellular component of the blood, followed by coagulation.
Coagulation removes clotting factors such as fibrinogen, prothrombin, and tissue thromboplastin from the blood. Whey is a good source of electrolytes. It is used for various diagnostic tests for hormones and enzymes. It is also used to determine blood groups.
Animal serums are used as antidotes, anti-toxins and inoculations. The serum can be stored at 2-6 ºC for several days.
Figure 1: Serum separated from blood
What is plasma
Plasma is a liquid portion of blood. It is a straw-colored protein-saline solution that traps blood cells and platelets. Therefore, plasma serves as an extracellular fluid. This takes up 55% of the total blood volume. water in plasma is about 92%.
Plasma contains dissolved proteins such as albumin, globulin and fibrinogen, glucose, clotting factors, hormones, electrolytes, carbon dioxide and oxygen.
It maintains satisfactory blood pressure and volume, balances the body's pH and serves as a medium for the exchange of minerals such as sodium and potassium.
Plasma is separated from its cellular part by centrifugation. Four units of plasma are diluted with one part of the anticoagulant, citrate-phosphate-dextrose (CPD), to a total volume of 300 ml. When a plasma sample is frozen within 8 hours of collection, it is called fresh frozen plasma (FFP).
When it is frozen for more than 8 hours but less than 24 hours, the plasma sample is called frozen plasma (FP). Once preserved by adding anticoagulants, frozen plasma can be stored for up to one year at -18ºC.
Plasma transfusion is performed in trauma patients, patients with severe liver disease and multiple clotting factor deficiency. Plasma derivatives, such as special plasma proteins, can be obtained by fractionation.
Viruses that cause HIV, hepatitis B and C are destroyed by treatment with heat or solvents. A diagram of a blood sample after centrifugation is shown in Figure 2.
Figure 2: Diagram of a blood sample after centrifugation
Definition
Serum: Serum is an amber-colored protein-rich liquid that is released when the blood coagulates.
Plasma: Plasma is the straw-colored liquid component of blood in which blood cells are suspended.
correspondence
Serum: Serum is that part of the blood that does not contain blood cells or clotting factors.
Plasma: Plasma contains serum and clotting factors.
Purchased from
Whey: Whey is obtained from the spinning after coagulation.
Plasma: Plasma is acquired by spinning before folding.
separation
Serum: Anticoagulants are not required to separate serum from blood.
Plasma: Anticoagulants are necessary to separate plasma from the blood.
Separation process
Whey: Whey is difficult to separate and time consuming.
Plasma: Separating plasma is comparatively easier and requires less time as compared to serum.
volume
Serum: Serum has a smaller volume than plasma.
Plasma: Plasma occupies 55% of the total blood volume.
Clotting factors
Serum: Serum lacks clotting factors.
Plasma: Plasma consists of clotting factors.
density
Serum: The density of serum is 1.024 g/ml.
Plasma: The density of plasma is 1.025 g/ml.
water
Whey: Whey contains 90% water.
Plasma: Plasma contains 92-95% water.
Medical use
Serum: Serum is used for enzyme tests and hormonal tests.
Plasma: Plasma transfusion is done for trauma patients, patients with severe liver disease, etc.
Storage
Whey: Whey can be stored at 2-6 ºC for several days.
Plasma: Once preserved by adding anticoagulants, frozen plasma can be stored for up to one year at -18ºC.
Conclusion
Serum and plasma are two derivatives of blood. Plasma is the liquid part of the blood in which the blood cells are suspended. It is a protein-rich liquid. Serum is the liquid part that remains after blood clotting.
Consequently, the serum lacks proteins that are involved in coagulation, such as fibrinogen. Both serum and plasma have medical uses.
However, the main difference between serum and plasma lies in the differential processes of release of both derivatives.
Reference: 1. “Blood serum.” Merriam-Webster. Merriam-Webster, n.d. Web. May 27, 2017
Source: https://ru.strephonsays.com/difference-between-serum-and-plasma
Classification of medicinal serums
Based on the direction and characteristics of the action of medicinal serums, they are divided into:
- antibacterial;
- antivirus;
- antitoxic;
- homologous (from human blood);
- heterogeneous (serum or immunoglobulins).
Antibacterial serums are produced by hyperimmunizing horses with the appropriate killed bacteria. These drugs contain antibodies that have opsonizing, lytic, and agglutinating properties. These serums are not very effective, so they are not widely used. They are classified as non-titrated drugs because there is no generally accepted unit for measuring their therapeutic effect. The purification and concentration of antibacterial serums is carried out by a method based on the separation of protein fractions and the isolation of active immunoglobulins using ethyl alcohol at a low temperature. This is called the cold hydroalcoholic deposition method.
Antiviral sera are obtained from the serum of animals immunized with viruses or strains of viruses. Some of these drugs are made using the hydroalcoholic precipitation method.
Antitoxic serums (antitetanus, antidephthyriasis, antigangrenosis, antibotulinum) are obtained by immunizing horses, using increasing doses of toxoids, and then the corresponding toxins. The preparations are subjected to purification and concentration, and are monitored for safety and non-pyrogenicity.
After this, the serum is titrated, that is, it is determined how many antitoxins are contained in one milliliter of the drug. To measure the amount of antibodies or specific activity of serum, a method is used based on their ability to neutralize the corresponding toxins. There is a unit of measurement for drug activity adopted by WHO. These are the International Antitoxic Units. To titrate antitoxic serums, one of three methods is used: according to Rayon, Roemer or Ehrlich.
Treatment with immune serums
Sometimes people wonder why serums are used for medicinal purposes. This possibility is explained by the large number of antibodies in the serum and the absence of rejection of one’s own biomaterial. The product is used to treat and prevent various diseases.
A person develops passive immunity, and the effects of poisons, toxins and pathogens are neutralized. The resulting mixtures are called antisera or immunobiological products.
There are two types of antiserum:
- Homologous.
- Heterogeneous.
Homologous is obtained from the blood of a person who has been vaccinated and has developed antibodies to a certain type of microorganism.
Immune serums are used for the prevention and treatment of infectious pathologies. They also allow you to accurately determine the type of pathogen, which facilitates diagnosis and makes therapy effective. Serums help fight the venoms of snakes and scorpions, and reduce the effect of botulism toxins.
In case of animal bites, anti-rabies serum must be administered, which is the only way to prevent the development of a dangerous disease.
How does serum differ from blood plasma?
Blood is a red liquid that moves through blood vessels, arteries and capillaries.
It carries nutrients to cells, organs and tissues. It is also responsible for cleansing cells of decay products to prevent self-poisoning of the body. Blood performs the following important functions:
- Transports nutrients to cells.
- Transports breakdown products to places of excretion.
- Saturates tissues with oxygen.
- Protects the body from the penetration of pathogenic microorganisms.
- Regulates body temperature.
- Provides stability when external conditions change.
In various types of studies, it is the remaining 10% that is of interest, which includes protein components:
- Albumin.
- Globulins.
- Fibrinogen.
During research, only the level of albumin and globulin is important. Fibrinogen is responsible for blood clotting, so its indicators are often not taken into account.
Serum cannot be obtained directly from blood collection, so plasma must first be isolated. Only after this can serum be prepared in laboratory conditions.
Blood composition
How is blood serum obtained?
To study the state of the body, it is necessary to obtain plasma, for which blood is taken from a vein. Before the procedure, the patient is recommended to follow a special low-fat diet. It is also necessary to avoid the use of alcohol, nicotine and medications that can affect the results.
Thanks to this, the serum has the possibility of long-term storage, which allows it to be actively studied and used for treatment.
The serum contains the following elements:
- Creatinine, responsible for kidney function.
- Enzymes.
- Good and bad cholesterol.
- Nutrients.
- Vitamins.
- Hormones.
They allow you to study your general health and identify various pathologies at the initial level. If the laboratory technician was careless when taking the analysis, red blood cells may be destroyed. They will turn the serum pink, making it unsuitable for study.
If the blood is drawn correctly, the specialist determines how to obtain the serum:
- Through the use of calcium ions.
- Through natural blood clotting.
Serum contains the most antibodies, which allows it to be used for various purposes:
- Carrying out biochemical analysis.
- To determine the type of pathogen in infectious diseases.
- To obtain an individual treatment serum.
- Checking the effectiveness of the vaccination.
It is stored longer, which makes it different from plasma. Thanks to this feature, the serum is subjected to long-term preservation in order to test for the presence of pathogens. Such measures make it possible to prevent the infusion of contaminated material into patients.
How to get serum
How is blood plasma different from serum?
Plasma is a yellowish, cloudy substance that is part of the blood. It contains basic information about the individual's health status. It helps to identify hormonal imbalances and problems in the functioning of individual organs and systems.
Serum is plasma without fibrinogen, which increases its lifespan. The serum can be used to obtain various drugs that have medicinal properties.
It helps conduct large-scale studies of the capabilities of the human body, testing the reaction of blood cells to various types of pathogenic microorganisms.
The difference between plasma and serum is as follows:
- Plasma is the entire component of blood, while serum is only a part.
- Plasma contains fibrinogen, a protein responsible for blood clotting.
- Plasma is always yellowish, and serum may have a reddish tint due to damaged red blood cells.
- Plasma coagulates under the influence of the enzyme coagulase, and serum is resistant to this process.
Blood in a test tube
Serum study
Laboratory tests of serum can determine the amount of proteins, carbohydrates and minerals in the blood. The results are used to draw conclusions about the coherence of the internal organs.
If a decrease in total serum protein is detected, prolonged fasting or a low-protein diet may be suspected.
When a person has not limited his diet, and the indicators are significantly below the norm, they speak of the following violations:
- Serious pathologies of the liver, kidneys, endocrine system.
- Burns or major blood loss.
- Presence of neoplasms.
- Problems with protein production under the influence of medications.
Exceeding the norm leads to:
- Dehydration.
- Vaccination.
- Tumor.
In such cases, additional diagnostics are often required. If the problems are caused by dehydration, the patient is recommended to adjust the drinking regime. In other situations, special treatment is necessary, which is prescribed by an appropriate specialist.
Serum is the most informative reagent when performing blood biochemistry, which allows you to diagnose pathologies:
- Pancreas.
- Liver.
- Kidney.
- Prostate gland.
- Bone tissue.
- Muscle fibers.
If its levels are reduced, problems begin with the level of iron in the blood. Neopterin reflects the speed of the immune response to adverse conditions.
Each protein is responsible for its own area, so the likelihood of error when making a diagnosis is minimal.
Blood serum
Treatment with immune serums
Sometimes people wonder why serums are used for medicinal purposes. This possibility is explained by the large number of antibodies in the serum and the absence of rejection of one’s own biomaterial. The product is used to treat and prevent various diseases.
There are two types of antiserum:
- Homologous.
- Heterogeneous.
Homologous is obtained from the blood of a person who has been vaccinated and has developed antibodies to a certain type of microorganism.
Immune serums are used for the prevention and treatment of infectious pathologies. They also allow you to accurately determine the type of pathogen, which facilitates diagnosis and makes therapy effective. Serums help fight the venoms of snakes and scorpions, and reduce the effect of botulism toxins.
In case of animal bites, anti-rabies serum must be administered, which is the only way to prevent the development of a dangerous disease.
Source: https://znk-mos.ru/otlichaetsya-syvorotka-plazmy-krovi/
Obtaining blood serum
To obtain whey, you can use several methods:
- Natural blood clotting.
- Another method is by adding calcium ions to the biomaterial, which implies an artificial coagulation process.
In any case, fibrinogen is activated, resulting in the formation of the desired substance.
In medicine, this procedure is called defibrination (centrifugation). This involves drawing blood from a vein.
But to get a reliable result, it is recommended to follow some rules:
- 24 hours before the test, avoid drinking alcohol and do not smoke;
- donate blood strictly on an empty stomach;
- the day before, do not eat fatty, salty, smoked foods, in other words, all dishes that have a detrimental effect on the human body;
- a few days before donating the serum, do not strain the body with significant physical activity;
- be less nervous, receiving negative emotions and stress;
- half a month before taking the tests, stop using any medications (there is no difference in them), including those against parasitic diseases. But if this is not possible, you need to tell the laboratory assistant about it.
Practice shows that most people understand what a blood test is, but serum is something incomprehensible to them. And they view this blood substance solely as a component for research, nothing more.
Difference between plasma and serum
Many people know that plasma and serum are related to blood. But not everyone has deeper knowledge on this issue. Let's consider what the declared substances are and how they fundamentally differ.
So, one of the fluids that performs its important functions in the body is blood. Obedient to the beats of the heart, it constantly moves, transporting various substances to their designated places. In addition to transportation, blood is responsible for many other aspects. Solving a large number of problems, this substance is quite complex.
A significant part of the blood consists of the so-called formed elements. They are represented by a certain number of leukocytes, platelets and bodies called erythrocytes. All mentioned components exist in a liquid medium, which is plasma. This substance can be observed at the top of the settled blood in the form of a light layer, while heavier particles settle down.
Plasma itself is also a combination of many components, each of which has a clear purpose. The basis here is water. Some types of proteins, vitamins, and nutrients are dissolved in it. In addition, mineral compounds, excreted metabolic products and other various elements are found in the plasma.
As we can see, we are talking about a rich substance that is naturally found in the blood, which always functions in the body. At the same time, serum can only be obtained outside the body. It is produced on the basis of plasma. The latter contains fibrinogen, a protein component responsible for blood clotting.
Serum remains after fibrinogen is removed using certain techniques. The resulting fraction is usually yellowish, but may also have a reddish tint due to the presence of certain particles. The value of such a liquid lies in its stability. Whey that is not subject to coagulation is stored for a long time. At the same time, its composition remains uniform, without unnecessary clots.
At the same time, the practical significance of the serum lies in the fact that it is rich in antibodies, which pathogens are afraid of. This blood processing product is indispensable in the manufacture of drugs that perform not only a therapeutic, but also a preventive function. A similar composition is used in the process of diagnosing diseases, for conducting various studies, as well as for some other purposes.
conclusions
- Blood plasma is the liquid part of the blood that remains after the removal of formed elements. In a suspended state, it contains formed elements - blood cells and platelets (or blood cells).
- Blood plasma in its composition is a very complex liquid biological medium, which includes vitamins, carbohydrates, proteins, various salts, lipids, hormones, dissolved gases and intermediate metabolic products.
- Blood serum (or blood serum) is the liquid fraction of clotted blood.
- Blood plasma is obtained by precipitation of formed elements, and serum is obtained by introducing coagulants (substances that promote blood clotting) into the blood plasma.
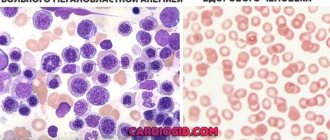
- Blood serum differs from plasma in the absence of a number of proteins of the coagulation system, such as fibrinogen and antihemophilic globulin, therefore it does not coagulate in the presence of coagulase, incl. microbial
Video
How does BLOOD SERUM differ from PLASMA?
The cells of our body are washed by a certain amount of bodily fluids, or humors. Due to the fact that these fluids occupy an intermediate position between human cells and the external environment, they ensure the survival of cells and play the role of a so-called shock absorber during sudden external changes, in addition, they are an effective means of transporting nutrients and waste products in the body.
An important role in the human metabolic process is played by blood, which consists of the liquid part of blood plasma and formed elements suspended in it:
- leukocytes - white blood cells that perform protective functions;
- erythrocytes - red blood cells containing hemoglobin (red respiratory pigment);
- platelets - blood platelets necessary for blood clotting.
Formed elements make up 40–45%, plasma – 55–60% of the total blood volume. This ratio is called the hematocrit ratio, or hematocrit number. In some cases, the hematocrit number includes only the volume of blood that accounts for the formed elements.
Blood plasma is a solution that consists of:
- water (90-92%) and dry residue (10-8%);
- organic and inorganic substances;
- formed elements (blood cells and plates);
- dissolved substances: proteins (albumin, globulins and fibrinogen); inorganic salts that are dissolved in the form of anions (sulfate, chlorine ions, phosphate, bicarbonate) and cations (potassium, magnesium, sodium and calcium); transport substances derived from digestion (amino acids, glucose) or respiration (oxygen and nitrogen), metabolic products (urea, carbon dioxide, uric acid) or substances absorbed by the lungs, skin and mucous membranes.
Plasma constantly contains all microelements, vitamins and intermediate metabolic products (pyruvic and lactic acids).
Lymph, blood, tissue, pleural, spinal, joint and other fluids form the internal environment of the human body. They originate from blood plasma and are formed through the process of plasma filtration by passing through the capillary vessels of the human circulatory system.
Plasma protein contains fibrinogen, which appears due to changes in the physicochemical state during blood clotting. Fibrinogen has the ability to pass from a soluble to an insoluble form, converting into fibrin and forming a clot.
Blood serum is a clear, yellowish (or light yellow) liquid separated from a blood clot after blood has coagulated outside a living body. From the blood serum of animals and people immunized with certain antigens, it is possible to obtain immune sera used in the diagnosis, treatment and prevention of various diseases.
The serum can be either red due to hemolysis - this is the process of destruction of red blood cells with the release of hemoglobin into the environment surrounding the red blood cells, or icteric - due to increased values of bilirubin (a pigment that is contained in the blood and excreted with bile, due to which it is called bile pigment).
Blood serum is used for preventive, diagnostic or therapeutic purposes. To obtain it, it is necessary to place sterilely collected blood in a thermostat for 30–60 minutes, remove the clot from the wall of the test tube with a Pasteur pipette and place it in the refrigerator for several hours (preferably for a day). The settled blood serum is aspirated or drained using a sterile Pasteur pipette into a sterile test tube.
Conclusions:
- Blood plasma is the liquid part of the blood that remains after the removal of formed elements. In a suspended state, it contains formed elements - blood cells and platelets (or blood cells).
- Blood plasma in its composition is a very complex liquid biological medium, which includes vitamins, carbohydrates, proteins, various salts, lipids, hormones, dissolved gases and intermediate metabolic products.
- Blood serum (or blood serum) is the liquid fraction of clotted blood.
- Blood plasma is obtained by precipitation of formed elements, and serum is obtained by introducing coagulants (substances that promote blood clotting) into the blood plasma.
- Blood serum differs from plasma in the absence of a number of proteins of the coagulation system, such as fibrinogen and antihemophilic globulin, therefore it does not coagulate in the presence of coagulase, incl. microbial