The condition when the heart beats slowly is called bradycardia. This term describes a slow or irregular heart rate (HR) that can cause dizziness or shortness of breath during normal daily activities or light exercise. The condition is defined as a heart rate less than 60 beats per minute. At this frequency, a sufficient amount of oxygenated blood cannot be distributed throughout the body.
Characteristics of the symptom
Typically the heart beats 60-90 times per minute. A person feels these contractions as a pulse when palpating the arteries. Under certain circumstances, heart activity may slow to below 60 beats per minute - in this case we are talking about bradycardia. Some people with slow heartbeats have serious problems with this condition, while others don't even know they have it.
Group 1 includes people whose slow heart rate is caused by other diseases, mainly dysfunction of the cardiac conduction system, disorders of the thyroid gland, and increased intracranial pressure. Group 2 includes athletes whose bradycardia is caused by training and is practically harmless.
Caution: fainting!
“AiF”: – Your center pays great attention to the so-called syncope, that is, fainting. Why?
L.M.: – First of all, because this is a very common problem. Especially in childhood. By the way, for a long time, many fainting spells in children were considered a purely neurological problem and were primarily associated with epilepsy. But later it turned out that in most cases, fainting is associated not only with neurological problems, but also with a sudden disruption of cardiovascular regulation, with a drop in blood pressure, which may be based on cardiac arrest caused by a disturbance in the heart rhythm. Moreover, 5% of fainting in children are associated with life-threatening arrhythmias. Most often - with a sudden increase in contractions of the ventricles of the heart (ventricular tachycardia) or a sudden slowdown in the rhythm (up to long pauses that can last 10 seconds or more).
This problem cannot be left without attention. If, after running up the stairs or racing with someone, your child gets tired quickly, sit down, if he turns pale or loses consciousness. The same thing with babies. If your baby suddenly turns pale or limp while crying or feeding, or if his nasolabial triangle suddenly turns blue, there is no need to think twice. See a doctor urgently!
Moreover, now there are a lot of technologies with which you can determine what causes fainting in a child, most of which are quite harmless. And often it is enough to simply adjust the child’s lifestyle, remove provoking factors and achieve excellent results without any medications.
“AiF”: – What if the situation is serious?
L.M.: – And in this case there is no need to panic. In the arsenal of arrhythmologists there are many effective means for treating cardiac arrhythmias. The main thing is to correctly assess the situation, which in childhood can range from normal to serious pathology, when the most active therapy or even heart surgery is necessary.
Causes and diseases
Bradycardia is considered more of a physical disease. On the contrary, the human psyche increases heart rate. There are many reasons for the slowdown, so let’s look at the most common ones.
Sport
Professional athletes are usually well trained, and their cardiovascular system works effectively at rest, even at low frequencies. Therefore, it is not surprising that athletes often have a heart rate of about 50 beats per minute without accompanying symptoms. This bradycardia is discovered by chance, it is natural, does not limit a person, and does not jeopardize his health. For these reasons, she is not being treated.
Medicines
Bradycardia can be caused by medications that slow the heart rate. Most often, an overdose of β-blockers occurs. These drugs are prescribed primarily for heart disease. They have a wide range of effects - lowering blood pressure, reducing the risk of dangerous arrhythmias and, among other things, slowing heart rate, thereby reducing the impact of stress on the heart.
Overdosing on these drugs may slow your heart rate too much. The situation can be resolved relatively simply - by reducing the dose or discontinuing β-blockers. The risk of side effects from β-blockers is worsened when combined with certain calcium channel blockers (eg, Verapamil, Isoptin, Veragexal, Diacordin). Often the heart pumps slowly due to digoxin poisoning (severe bradycardia).
Decreased thyroid function
When the concentration of thyroid hormones decreases, cardiac activity slows down.
Sick sinus syndrome
This is a disease (English: Sick Sinus Syndrome - SSS), more common in old age. We are talking about a violation of the SA node, which is part of the cardiac conduction system. This is the area where electrical stimulation usually occurs. Excitement in the SA node propagates through the transmission system from the atrium to the ventricles, causing coordinated contractions of the myocardium. With sick sinus syndrome, the sinus node does not work properly, and the heart rate may be too slow and alternate with rapid atrial fibrillation. The cause of SA node failure is most likely due to age-related degeneration.
Disorder of the cardiac conduction system
When the SA node and atrial transport system are disrupted, the heart adapts and begins to generate electrical signals in the ventricular junction or ventricular region. But these areas cannot generate excitations with sufficient frequency, and the heart rate can drop to 40 beats per minute. A similar situation occurs with certain types of atrioventricular blockages, characterized by disturbances in the transmission of impulses from the atria to the ventricles.
Ion vibrations
Bradycardia often occurs as a concomitant sign of increased potassium concentrations.
The heart beats, stops...
“AiF”: – Leonid Mikhailovich, your center is one of the few in our country that seriously deals with the diagnosis and treatment of heart rhythm disorders in children. How often do they occur at this age?
Leonid Makarov: – Heart rhythm disturbances in children are not always the primary cardiac diagnosis, but occupy third place after arterial hypertension and heart defects. At the same time, arrhythmias in children are often detected by chance, during a routine examination by a pediatrician. Indeed, unlike adults, children, even with serious heart rhythm disturbances, often do not feel arrhythmia.
“AiF”: – What types of arrhythmias do pediatric cardiologists most often deal with?
L.M.: – With extrasystole – an interruption of the normal heart rhythm (such, for example, as speech stuttering). This type of arrhythmia, which occurs in 8–20% of healthy children, is usually benign in origin and does not require serious treatment. But there are also types of extrasystole and other heart rhythm disturbances that pose a serious danger to the health and life of the child. At the same time, for the time being, he may feel quite normal and be considered absolutely healthy. The most dangerous are arrhythmias that arise against the background of congenital or acquired diseases of the heart muscle (myocarditis, cardiomyopathy), heart defects, although this, fortunately, is not the most common scenario.
“AiF”: – Why else could dangerous interruptions occur?
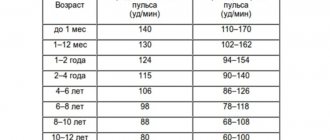
L.M.: – There are many reasons. Unlike adults, many vital systems (vegetative, nervous, immune) in a child are still immature. Including those that affect heart rate. Years must pass before the pacemaker located in the heart - the sinus node - is firmly established as the main generator of impulses that contribute to the synchronous contraction of the necessary chambers of the heart. A child's heart is very different from an adult's. It even beats faster. A growing body places increased demands on it. The slightest glitch and problems begin.
Associated symptoms
Slow heart action may not occur at all or may be accompanied by a variety of signs of heart failure. This is logical - a slow-working heart muscle ceases to sufficiently supply blood to tissues, including the brain.
Symptoms accompanying a slow pulse:
- dizziness;
- fainting;
- extreme fatigue;
- dyspnea;
- chest pain;
- problems with concentration;
- decrease in blood pressure.
Some people have no symptoms, or their symptoms are so mild that a slow heart rate is perceived as just a normal sign of aging.
Treatment
Bradycardia can occur as an independent condition or accompany other diseases. Therefore, it is important to determine its cause, and treat it accordingly. It is important to find out what medications the patient is taking. If beta-blockers are used, they should be stopped and replaced if necessary. If the cause of bradycardia is a thyroid disease, the disease must be controlled with medications (eg appropriate hormone tablets).
But, if the cause of a slow heartbeat is a dysfunction of the transport system, treatment is more complex. If the patient's condition is acute, medications that accelerate cardiac activity (Atropine, adrenaline) are prescribed, but their effect is short-term, and they cannot be used for a long time.
In the case of a disorder of the transfer system, the only long-term treatment option is the implantation of a pacemaker. A pacemaker is a small device implanted under the skin, most often under the collarbone on the left or right side of the chest. The pacemaker consists of a battery and computer circuits housed in a small metal case. The device constantly monitors heart rate.
When it detects a problem in the form of a slow rhythm, it sends a small electrical impulse aimed at correcting the problem.
FacebookvKontakteTwitterWhatsApp
Dangerous failure
“AiF”: – What is more dangerous – tachycardia (too fast heart rate) or bradycardia (too slow)?
L.M.: – Both can be equally dangerous. It all depends on the cause and severity of the arrhythmia, as well as on how far the pathological process has progressed.
“AiF”: – What can provoke it?
L.M.: – In childhood, arrhythmias are often hereditary. But heart rhythm disturbances can also be caused by severe pneumonia, tonsillitis, chronic diseases of the nasopharynx, severe bronchitis and other infectious and inflammatory diseases (including intestinal ones, in which the electrolyte balance of the body may be disturbed). But quite often we do not see obvious damaging factors for the heart, but the child has arrhythmia.
“AiF”: – How do you identify it?
L.M.: – Each pathology has its own specifics for making a diagnosis: from the classic ECG, daily measurement of heart rate (Holter monitoring) to electrophysiological transesophageal study of the heart rate using a thin electrode, which resembles a conventional gastroscopy and is inserted through the esophagus closer to the child’s heart . We also widely use the methods of modern electrocardiological diagnostics, when, through various new methods of analyzing the heart rhythm, we can identify the electrical instability of the heart, which is the basis for the development of arrhythmia and their typical symptoms - palpitations or fainting.
“AiF”: – And at what age can such disorders be diagnosed?
L.M.: – From anyone. There are situations when a newborn child needs to have a pacemaker installed or undergo urgent surgery. By the way, at one time a large-scale study was carried out at maternity hospitals in Kazan, taking ECGs of newborn babies. So, 12% of apparently absolutely healthy babies had serious changes in the ECG and disturbances in the functioning of the heart. Some of them, by the way, can be the cause of most cases of sudden infant death, which most often threatens children aged 4 to 8 months. Since then, ECG examinations have become mandatory in many maternity hospitals in our country.
In addition to infancy, other peak periods for the manifestation of arrhythmias in children are considered to be 4–5 years, 6–8 years, and adolescence. That’s when you need to take an electrocardiogram for the child. Necessarily!