Only a doctor can qualitatively interpret the results of a blood test. However, as in any specialty, in medicine there are good and not so good specialists.
Of course, only an authoritative commission can determine the level of a doctor’s true qualifications, but we want to control the quality of the care provided ourselves, if only to develop trust in the doctor and his recommendations. In this article we tell you how to understand what a deviation in a particular blood test parameter means.
From a standard analysis form you can find out what normal blood test values should be, but this is often not enough to determine pathology. It is important to know exactly how an increase or decrease in the indicator affects the physiology of the body. It is valuable to know under the influence of what factors the value of the analysis can rise or fall, in what combinations these changes become a characteristic syndrome - a group of typical signs of the disease. Let's try to understand each indicator separately.
Prothrombin
Prothrombin time (PTT) is a laboratory indicator that reflects the functioning of the extrinsic pathway of activation of the human blood coagulation system. Often, the PTT test is prescribed in conjunction with the determination of activated partial thromboplastin time (aPTT) - this test shows the activity of the intrinsic coagulation pathway and activation of the coagulation system.
Often, in addition to PTT and APTT, the attending physician refers the patient to determine the prothrombin index (PTI) and international normalized ratio (INR). These indicators are calculated by the laboratory where the research is carried out.
PTT and APTT provide the physician with a wide range of data on the state of both the patient's coagulation and anticoagulation systems. Based on this information, the doctor can begin conservative treatment of the patient, prepare for surgery, or conduct therapy aimed at normalizing the functioning of the coagulation system.
The PTV norm, which is accepted throughout the world, is 11-16 seconds. It is believed that this indicator of prothrombin time is optimal for most healthy people.
Before prescribing a PTT test, the doctor must take into account the patient’s medical history. For example, when taking anticoagulants (especially warfarin), the prothrombin time changes, increasing significantly.
Platelets are reduced (thrombocytopenia)
When the concentration of platelets in the CBC decreases, they speak of the development of thrombocytopenia, which is accompanied by a blood clotting disorder and a tendency to bleed (gums bleed, nosebleeds or intestinal bleeding often occur, menstruation becomes long and heavy). Thrombocytopenia develops in a number of serious diseases due to the loss of elasticity of the vascular wall, their fragility and fragility and the risk of internal bleeding.
Reasons that provoke a decrease in platelet levels include:
- hemolytic-uremic syndrome or Gasser's disease (a combination of hemolytic anemia, thrombocytopenia and acute kidney failure);
- thrombocytopenic purpura or Werlhof's disease (one of the widows of hemorrhagic diathesis);
- allergic thrombocytopenia (taking a number of medications: procainamide, heparin, co-trimoxazole);
- DIC syndrome (second stage);
- severe liver damage (hepatitis, cirrhosis);
- alcoholism;
- malaria;
- enlarged spleen;
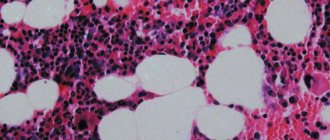
- bone marrow diseases, some leukemias;
- megaloblastic anemia;
- pathology of the thyroid gland (hypothyroidism, thyrotoxicosis).
It is important to note that a decrease in platelet concentration (75 – 150) is observed in pregnant women, which is not regarded as a pathology.
When is the study scheduled?
The attending physician prescribes a determination of prothrombin time in a number of situations:
- Diagnosis of the patient's body. PTT is often prescribed as one of the methods for studying the state of the human body. Diagnosis is carried out both for preventive purposes (to notice the development of a pathological condition in time and begin its treatment), and if a person is suspected of having a certain disease.
- Preoperative preparation. Classical preparation for planned surgery includes an analysis of the patient’s hemostatic system. If a person has disorders in the blood coagulation system, the doctor needs to normalize coagulation parameters to prevent bleeding on the operating table.
- Postoperative diagnosis. In the postoperative period, careful monitoring of the condition of the human body, in particular, the hemostatic system, is necessary. An increase in prothrombin time carries a risk of bleeding, and a decrease in PTT should alert the physician to the threat of blood clots in a person.
- Suspicion of the presence of pathology of the hemostatic system. If a patient comes with complaints of bleeding that occurs easily and does not stop for a long time or constant bruising, the doctor will refer him for a PTT test. Many other symptoms that indicate a malfunction of the blood coagulation system will alert the doctor, so he will refer the person for additional studies of the hemostasis system.
- Threat of hidden bleeding. If the patient has characteristic complaints indicating the development of hidden bleeding (pallor, weakness, tachycardia, impaired consciousness, weak pulse wave), the doctor may suspect the development of hidden bleeding and prescribe a determination of prothrombin time.
- Risk of blood clots . PTT analysis is often prescribed to patients who are at risk of developing extremity venous thrombosis. Timely determination of PTT allows the doctor to prescribe anticoagulant therapy (drugs that reduce the activity of the blood coagulation system) in time to prevent the development of dangerous complications of thrombosis.
- Analysis of the liver condition. The liver is an organ in which many factors of the human blood coagulation system are synthesized. If liver function is impaired, the homeostasis system will necessarily suffer - due to its excessive activation, or, conversely, insufficiency of factors that the liver should synthesize. Determining prothrombin time helps to detect liver diseases in time and begin timely therapy for the patient.
- Alarming patient history. A prothrombin time study is required if the patient suffers from cardiovascular pathology or complications of heart disease. If there is a history of thromboembolism of certain arteries (blockage of an artery with a thrombus or embolus), the doctor will definitely prescribe a PTT determination to prevent the progression of this condition or the formation of a new thromboembolism.
- Diagnosis of nosebleeds, hemorrhages in the patient’s organs and tissues. PTT analysis often helps to determine the reasons for the development of frequent nosebleeds in a patient in order to begin the correct therapy in a timely manner. In addition, the study plays an important role in determining hemorrhages in individual tissues or organs of a person.
- Study of anemia in a patient. Anemia is a condition accompanied by a decrease in the concentration of hemoglobin in the red blood cell, as well as a decrease in the number of red blood cells (red blood cells that carry hemoglobin) per unit of blood. What does this mean for prothrombin time? With a decrease in the number of red blood cells, the time for thrombus formation increases, which necessarily affects the PTT: the PTT rate increases significantly.
- as well as conditions in which there is a deficiency of vitamin K. These particular situations are considered by doctors on an individual basis: antiphospholipid syndrome is not so common in the population. Vitamin K deficiency is a more common condition. Vitamin K is one of the factors of the blood coagulation system, and its deficiency will certainly negatively affect the homeostasis system.
The determination of prothrombin time is constantly used by doctors to monitor the patient’s dynamics when prescribing anticoagulant therapy. Both direct and indirect anticoagulants require special attention from the attending physician: with pathological PTT values, dosage adjustment or the prescription of another drug is necessary. PTT analysis is also usually prescribed when a patient is hospitalized for inpatient treatment.
What is PLT in blood test?
The term PLT (or platelets) refers to the well-known platelets - the formed elements of blood, which are also called blood platelets. Cellular structures have a number of features: small diameter, flattened shape, and the absence of a formed nucleus (in humans). These factors together “lighten” the mass of each platelet, allowing it to move around the body at high speed.
The formation of plates occurs in the bone marrow. Their lifespan is only 7–11 days. In order to understand the significance of PLTs, it is necessary to know their main function - it is to stop bleeding from fractures, cuts, burns and severe blows, accompanied by internal ruptures of blood vessels. When the resulting injury provokes a violation of the integrity of the blood vessels, platelets, having received an alarm signal from the brain, rush to the site of injury.
With the help of their pseudopodia (different-sized outgrowths), they attach to the edges of the wound, stick to each other, and then self-destruct. As a result of the breakdown process, blood platelets secrete a unique enzyme - thrombin, which, acting on another enzyme - fibrinogen, converts it into fibrin, which is thin elastic threads. They, in turn, quickly entwine the damaged area, holding red blood cells (blood cells) in their network. Thus, a clot or thrombus is formed, which dissolves immediately after the wound heals.
In addition, platelets remove from the vessels a group of antibodies that retain viral particles. A low or high percentage of PLT content in a general blood test most often means the development of pathology, since blood platelets are indicator cells that show sensitivity to almost any destructive change in the internal environment of the body. To study the number of platelets, both capillary blood (from a finger) and venous blood (from the ulnar vein) are suitable.
After collecting the biomaterial, the samples are studied within the chemical laboratory. Test results are usually reported the next day.
What is the research used for?
Prothrombin time is an important laboratory indicator that doctors use to diagnose a patient and prescribe the correct treatment. A significant list of indications for performing PTT analysis includes both various screening studies and diagnostic purposes. In addition, prothrombin time analysis is used to monitor the progress of human therapy.
Thus, PTT is an exceptional diagnostic marker, without which correct and effective treatment of a person is impossible.
Platelets are increased (thrombocytosis)
An increase in platelet count (thrombocytosis) is observed when:
- excessive physical stress
- chronic inflammatory processes (rheumatoid arthritis, tuberculosis, sarcoidosis);
- myeloproliferative diseases (primary erythrosis, chronic myeloid leukemia, myelofibrosis, myelosclerosis);
- some hemolytic anemias;
- hemolysis or severe blood loss;
- carcinoma, lymphoma;
- after removal of the spleen.
Sources:
- Eugenio D. Hottz. Platelets in Immune Response to Virus and Immunopathology of Viral Infections. — Front Med (Lausanne). Apr 2018.
- Data from the independent laboratory Invitro.
- Data from Helix laboratory.
- Steven Kim, MD. Acquired Platelet Function Disorder. — Healthline, Jan 2021
- Douglas B. Cines. Thrombocytopenia in pregnancy. - Blood. 2017 Nov 23; 130(21): 2271–2277
- Danilova L.A., Doctor of Medical Sciences, Prof. Analyzes of human blood, urine and other biological fluids at different age periods, SpetsLit, 2014.
Method of determination
Fresh plasma from the patient is used to determine prothrombin time. At the first stage, blood for testing is collected in a special tube that already contains sodium citrate. Sodium citrate is a necessary component in order to “bind” calcium in the blood. This is because calcium promotes blood clotting, which can have a negative effect on blood samples. For example, blood clotting will occur before the tube containing the material reaches the laboratory.
Then, in a laboratory setting, the tube is placed in a centrifuge and excess calcium is added at a certain temperature range (usually 37 degrees Celsius) in order to “free” the bound calcium: the blood again has the ability to clot.
At the next stage, a special blood clotting factor is added (in medical circles it is called clotting factor III). A laboratory specialist records the period of time during which the formation of a blood clot occurred. This period is the prothrombin time. Traditionally, the normal PTT is considered to be 11-16 seconds. However, PTT values may vary depending on different conditions.
PTV norm
| Age category of the person | PTV value, sec |
| Premature babies | 13—18 |
| First 185 days of life | 12—16 |
| Up to 5 years | 14—17 |
| Up to 15 years | 11—15 |
| Adult patients (over 18 years old) | 11—16 |
The PTV norm does not depend on a person’s gender: for both men and women, one normal interval for this indicator is determined.
Decoding of PTV analysis
Determining the normal prothrombin time for a particular patient is the task of the attending physician. If a person, for example, is taking anticoagulant therapy, then his PTT rate will be different from a patient not taking such medications. That is why deciphering PTV should be done exclusively by the attending physician: only he knows the characteristics of the human body and represents the expected boundaries of PTV in a person.
A situation where the PTT is elevated in a patient indicates that the blood coagulation system is not working actively enough: in fact, the blood needs more time to form a clot and stop bleeding.
If the prothrombin time is reduced , then the opposite condition is evident: the blood clots too quickly and very actively, which threatens the development of blood clots.
A woman’s special condition is during pregnancy. At this time, at different stages of gestation, PTT can fluctuate significantly, so the gynecologist is obliged to regularly analyze PTT in a woman.
The reasons for the change in the normal PTT value must be determined by the patient’s attending physician, and then the necessary therapy must be prescribed to eliminate the disease that led to the change in PTT.
What factors influence changes in PLT?
Platelet counts in a blood test can rise and fall sharply even in the absence of any diseases. Of course, external factors, a person’s lifestyle and exposure to bad habits play a special role in such changes.
Among the most significant are:
- Use of certain medications (Heparin, Epinephrine, Aspirin, etc.).
- Eating foods that affect blood viscosity, such as cherries, ginger or onions.
- Alcohol poisoning.
- Active sports.
- Poor nutrition.
- Smoking.
- Previous surgery.
- Exposure to radiation.
- Absence of the spleen, which is responsible for the stabilized utilization of 1/3 of platelets unsuitable for work.
If the patient was previously transfused with donor blood with a low platelet content, the recipient's test results will show a reduced PLT index for some time.
Prothrombin time during pregnancy
The study of prothrombin time during pregnancy is an important diagnostic method that is used to analyze the condition of patients. In addition to routine biochemical studies, obstetricians and gynecologists use PTT analysis to assess the condition of a woman during gestation.
Analysis of prothrombin time during pregnancy is indicated for the following conditions:
- the patient had a history of spontaneous abortions or miscarriages, or frozen pregnancy;
- the pregnant woman has been diagnosed with uterine hypertonicity or other conditions that threaten the fetus;
- Obstetricians and gynecologists confirmed the presence of signs of the development of gestosis in a woman, or there is a threat of development of gestosis.
Prothrombin time in women during pregnancy ranges from 11 to 18 seconds. If the PTT is increased, then the doctor will probably suspect the development of bleeding in the patient during the labor or postpartum period. If the prothrombin time is reduced, then there is a threat of developing a dangerous condition - disseminated intravascular coagulation syndrome.
To prevent complications in the childbirth or postpartum period, doctors actively use the PTT study: diagnosis will indicate in time violations of the hemostatic system, which will allow the pregnant woman to begin treatment.
PTV reduced
If, during decoding of the PTT, it turns out that the indicator is reduced, this may indicate the following clinical situations:
- The patient has polycythemia. With this disease, the number of red blood cells (erythrocytes) increases significantly. The blood acquires a “thicker” structure, clots faster, and blood clots form more actively in it, so the prothrombin time is reduced.
- Deep vein thrombosis of the lower extremities. This pathology is characterized by the active formation of thrombi (blood clots) in the veins of the lower extremities, which has a deeper basis - a person may experience both an excess of platelets and too many blood clotting factors. Diagnosis of the primary causes of thrombosis is carried out by the attending physician, and a decrease in PTT in this case is a red marker that indicates the seriousness of the patient’s condition.
- Taking oral contraception. As a rule, PTT is slightly reduced if a woman takes oral contraceptives according to the regimen, both for the purpose of treating gynecological pathology and to protect against unwanted pregnancy.
- Hereditary disorders of the blood coagulation system. Genetically determined pathology in the form of a violation of the amount of one or more factors from the prothrombin complex, hereditary coagulopathies, and - or hypo-fibrinogenemia cause a decrease in PTT in humans.
- Acute DIC syndrome. At one of the stages of development of DIC syndrome, excessive blood clotting is observed, which becomes a life-threatening condition for the patient.
- Violation of the concentration of blood coagulation factors in the serum. Sometimes the reason for a decrease in PTT is a change in the required concentration of antithrombin, antithromboplastin (their increase), or an excess of heparin in the circulating blood.
- Other chronic diseases. Often, in patients with intestinal pathology (diseases of the small intestine, dysbiosis), with damage to the pancreas (chronic pancreatitis, pancreatic cancer), or pathology of the gallbladder, a decrease in PTT is observed. In addition, a decrease in the indicator is characteristic of nephrotic syndrome, which is associated with kidney damage.
- Oncological pathology. Prothrombin time is reduced in acute or chronic leukemia in humans.
It is important to note that some drugs used in various fields of medicine significantly affect the PTT rate:
- barbituric acid derivatives (barbiturates);
- hormone replacement therapy (thyroid hormones, androgens, anabolic steroids);
- some types of antibacterial drugs;
- antiarrhythmic drugs to correct the patient’s heart rhythm;
- antidiabetic agents;
- H2 receptor antagonists, which are used in the treatment of chronic gastritis and gastric and duodenal ulcers;
- diuretics, laxatives.
As a rule, a slight decrease in PTT is observed in women in the last trimester of pregnancy, which is considered a physiological norm and is interpreted on an individual basis.
PTV increased
Prothrombin time is increased in the following conditions:
- Deficiency of individual coagulation factors due to hereditary causes or acquired diseases. PTT is increased when the patient has a deficiency of coagulation factors II, V, VII, X - these conditions are congenital disorders. Acquired deficiency of coagulation factors is observed in chronic diseases of the liver, kidneys, as well as autoimmune pathology.
- DIC syndrome. At one stage of development of DIC syndrome, PTT decreases, at another, a significant increase in PTT is noted.
- Use of anticoagulant drugs. The use of treatment prescribed by a doctor (for example, acetylsalicylic acid, which has, among other things, anticoagulant activity) may be accompanied by a decrease in PTT. The targeted use of other anticoagulants (for example, warfarin) naturally reduces PTT, which should be taken into account by the attending physician when interpreting the study results.
PTT is increased when taking antibacterial drugs, steroid hormones, and some laxatives.
Drugs that affect platelet levels
Long-term use of these drugs may change platelet levels:
- aspirin
- pain relievers such as ibuprofen and naproxen
- antihistamines
- asthma medicine
- sildenafil (Viagra)
- drugs used to prevent blood clots, such as clopidogrel
- antibiotics
- antidepressants and antipsychotic drugs
- Cholesterol-lowering drugs (statins)
- calcium channel blockers (verapamil).