Causes of appearance in the blood
C reactive protein is produced in liver cells. It consists of carbohydrates and proteins. In the blood of a healthy person, the amount of the substance is minimal, so it is impossible to detect it even with the help of high-precision methods and modern equipment. Increased production of CRP begins only with the development of pathologies that pose a threat to the human body. They can be provoked by a variety of harmful microorganisms: bacteria, viruses, fungi.
CRP appears in increased quantities in the blood during injuries and surgical operations, damage to internal organs and the development of tumors. Also, CRP analysis shows the presence of a substance in the blood during autoimmune reactions of the body, which lead to impaired immunity. In this case, substances are produced that damage healthy tissue.
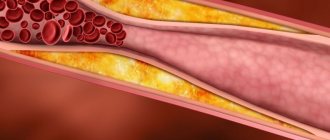
When C reactive protein in the blood is elevated, this indicates the activation of the natural defense systems of the human body. But at the same time, the substance at high concentrations has a negative effect on fat metabolism, which increases the risk of cholesterol plaques on the walls of blood vessels. That is, if the presence of CRP is confirmed, the likelihood of vascular complications can be assessed by its concentration.
C-reactive protein test: what is it for?
What is C-reactive protein? What can a test result for this substance tell a doctor? What is the normal level of C-reactive protein in the blood? Nikita Valerievich Vorobyov, a neurologist at the Expert Clinic Kursk, answers these and other questions.
— Nikita Valerievich, before we talk about the analysis for C-reactive protein, please tell us what kind of substance this is? Is it present in the body normally or does it appear only during certain diseases? And what is the significance of the C-reactive protein test?
— C-reactive protein is a kind of indicator of various diseases, the most sensitive marker of the inflammatory process. With its help, the doctor can determine the severity of inflammation in the body. This substance is synthesized by liver cells in response to inflammatory processes in the body: during tissue damage, cell necrosis, during an infectious process, during exacerbation of chronic diseases, for example, rheumatological ones, including ankylosing spondylitis.
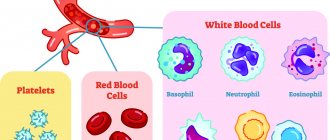
Being in the body within normal concentrations, C-reactive protein has a protective function: it initiates immune processes, stimulates phagocytosis (a process in which special blood cells and body tissues - phagocytes - capture and absorb various foreign structures, such as destroyed cells, bacteria, antigen-antibody complexes, etc.).
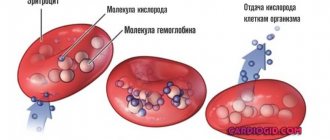
When the content of C-reactive protein in the blood begins to exceed the norm, this indicates some kind of inflammatory process, the nature of which the doctor will have to find out. Moreover, during acute inflammation, the content of C-reactive protein increases very quickly, literally in 6 hours. Much faster than, for example, ESR changes - the erythrocyte sedimentation rate.
When the treatment itself has already begun, an analysis for C-reactive protein helps the doctor understand what phase the pathology is in: is the acute period still ongoing or the disease has declined.
— What is the normal level of C-reactive protein in the blood?
- Depending on the laboratory, the norm of C-reactive protein varies from 0 to 1 milligram per liter and from 0 to 5 milligrams per liter. There is no lower limit of normal; this protein is detected in the blood only in response to acute inflammation. Within acceptable limits, the level of C-reactive protein can fluctuate during physical activity (for example, after playing sports), smoking, or eating fatty foods.
- Then, it turns out, there is no point in asking under what circumstances C-reactive protein can be lowered? Is this question not valid?
- Right. There are two options: either the protein is normal, or its content is increased. There can be no reduction.
— Why can C-reactive protein be elevated?
— I have already partially answered this question: its content increases with the appearance of inflammatory processes in the body. The reasons for the increase in C-reactive protein may be:
- previous trauma, burn;
- rheumatological disease;
- presence of infection;
- transplant rejection reaction.
The content of this protein also increases during myocardial infarction, after undergoing severe operations.
An analysis for C-reactive protein - I repeat, as an auxiliary study - is used if there is a risk of developing cardiovascular complications, in particular, when diagnosing atherosclerosis: with inflammation of the vascular walls, the concentration of this protein also increases.
— Tell me, how does C-reactive protein behave during pregnancy?
— Since pregnant women have a higher immune system tension than non-pregnant women and, even more so, than men, the content of C-reactive protein during this period may be increased. If the woman is healthy and gestation is normal, this indicator increases from the 16th to the 28th week of pregnancy, then gradually begins to decrease. Then it may increase immediately before childbirth. A high concentration of C-reactive protein in the blood may indicate a risk of developing late toxicosis.
— Which doctor and under what circumstances prescribes a test for C-reactive protein? What might be the reason for this research?
— A general practitioner, therapist, or neurologist can refer a patient for this analysis. But, since this type of research is primarily used in the diagnosis of rheumatological diseases, most often this direction is issued by a rheumatologist.
An analysis for C-reactive protein is carried out, for example, if ankylosing spondylitis is suspected. When making a diagnosis, this study plays an auxiliary role; it is used in conjunction with other markers. When ankylosing spondylitis has already been detected, the doctor can determine by the concentration of C-reactive protein what phase the disease is in - in the stage of exacerbation or remission (the period of weakening or disappearance of the symptoms of the disease).
This test is also prescribed for joint pain, increased body temperature, and infectious processes.
Neurologists use this type of analysis to understand the nature of a patient's back pain.
— Do you always need a referral from a doctor to get tested for C-reactive protein? And if not, what is more correct: to take it as directed or on your own initiative?
— Having a referral for such an analysis is not a prerequisite. But it is still better to do any research after consulting a doctor.
— Does the patient need to somehow prepare for the C-reactive protein test?
— The procedure is a simple blood draw from a vein. No special preparation is required from the patient. The generally accepted rules in such cases apply. The test is taken on an empty stomach, after a 12-14 hour fast (usually this is done in the morning). The day before, 24 hours before the test, you need to avoid drinking alcohol and intense physical activity. It may be necessary to temporarily stop taking certain medications, but only after consultation with your doctor.
1-2 hours before the test, you need to refrain from smoking, tea, coffee, and juices. You can drink still water. Running and quick climbing of stairs should be avoided. It is not recommended to do the study after emotional stress or severe anxiety.
— How long should I wait for the test result?
- Usually no more than one day.
Interviewed by Igor Chichinov
Want to learn more about other tests? Read articles in our “Laboratory Tests” section If you need to get tested for C-reactive protein or other tests, you can sign up here You can make an appointment with specialists here ATTENTION: services are not available in all cities
The editors recommend:
Pain with rheumatoid arthritis: how to help the patient? Are you worried about pain in your lower back? We're talking about sacroiliitis Are you crunchy? What will an MRI of joints tell you?
For reference:
Vorobiev Nikita Valerievich
Graduate of the Faculty of Medicine of Kursk State Medical University in 2021. In 2021, he completed his residency at Kursk State Medical University in the direction of Neurology. Advanced training: interventional methods of treatment in neurology, First Moscow State Medical University named after. THEM. Sechenova, 2021. Advanced training: local therapy of diseases of the musculoskeletal system and compression-neural syndromes, Kursk State Medical University, 2021. Currently, a neurologist at the Expert Clinic Kursk. Receives at the address: st. Karl Liebknecht, 7.
Standard indicators
C reactive protein, the norm of which is universal for all categories of people, makes it possible to detect inflammatory processes in the human body. But it is impossible to make a diagnosis solely on the basis of a CRP blood test.
Today it is believed that the SRP norm is up to 5 mg/l. In newborns, the level can increase to 15 mg/l. When C reactive protein is elevated, suspicions arise about the development of an inflammatory or malignant process. This means that more accurate diagnostics using other methods is required.
But since the use of high-precision equipment makes it possible to determine the minimum amount of a substance in the blood, experts have begun to apply the concept of the basic value of CRP. It was introduced to assess the risks of damage to the heart and blood vessels, in cases where the development of any inflammatory processes is excluded. The norm for the basic indicator of the substance is less than 1 mg/l.
Effect of drugs on CRP concentration
Taking acetylsalicylic acid or aspirin, even in high doses, does not affect the quantitative level of CRP. This is somewhat surprising since aspirin is known for its anti-inflammatory properties.
Patients with high cholesterol who take statins are less likely to have a heart attack because statins not only lower lipid levels but also have anti-inflammatory properties. This is very important because high CRP and low cholesterol are more dangerous than high cholesterol and low CRP. The level of CRP is also reduced by drugs from the group of fibrates and beta-blockers, but less effectively than by statins.
Reasons for the increase
When C reactive protein is elevated, there may be different reasons. Today they are divided into three main groups:
- Oncology.
- Inflammatory processes.
- Vascular pathologies.
The risks of developing certain diseases are assessed by the concentration of the substance in the blood:
- Less than 19 mg/l. This deviation is considered insignificant. Exceeding the norm can be triggered by any negative factor affecting the body. As a rule, in this case, analysis is required at a certain frequency. If constantly elevated CRP is detected, diagnostics are required to exclude autoimmune and oncological pathologies.
- 20-50 mg/l. Indicators always rise to this level with various viral infections.
- More than 100 mg/l. A bacterial infection can provoke a strong immune reaction in the body, against which serious diseases develop: pneumonia, salmonellosis, pyelonephritis, etc.
C-reactive protein and ESR
ESR or Birnatsky reaction is a measurement of the erythrocyte sedimentation rate in a test tube with blood. It is expressed in millimeters per hour. ESR is an indirect indicator of the inflammatory response. However, the ESR test is less specific than CRP.
In addition to inflammation, an increase in ESR is also affected by:
- Obesity. Adipose tissue is a source of interleukin 6. This is one of the proteins involved in the formation of inflammation.
- Kidney failure. In end-stage renal failure and in the case of nephrotic syndrome, patients have significantly increased ESR values.
- Hemoglobin concentration. Anemia speeds up the decline of red blood cells.
- Shape of red blood cells. Determination of ESR is unreliable in diseases with abnormal red blood cells, such as sickle cell disease.
If there is a disproportion between CRP concentration and ESR, the first step is to consider the possibility of a false measurement due to the above factors or laboratory error, such as taking too long from collection to delivery to the laboratory or storing the tube in inappropriate conditions.
CRP levels respond more dynamically to increased inflammation than ESR. In the case of, for example, lupus erythematosus, the ESR value may be elevated when the level of CRP in the blood is low. This is caused by high levels of type 1 interferon, which suppresses the liver's production of CRP.
If you find an error, please select a piece of text and press Ctrl+Enter
General information
CRP is produced in liver cells (hepatocytes) immediately after damage has occurred, the provoking factors of which can be bacteria, fungi, antigens, various immune complexes, etc.
The level of C-reactive protein directly depends on the type, form (acute, chronic), stage and activity of the disease. Within the first 4-6 hours after cell damage, active synthesis of CRP begins, and after a day its density increases exponentially.
With early diagnosis of the disease and timely treatment, within a few days the analysis will show a decrease in the concentration of CRP. The indicator will be completely reset only 1-2 weeks after the start of conservative therapy.
Chronic pathologies are characterized by an undulating course; accordingly, CRP will increase during the period of exacerbation and independently decrease during remission (subsidence of clinical symptoms).
A biochemical blood test with determination of CRP values makes it possible to distinguish a bacterial disease from a viral, fungal or parasitic one. It is known that in case of viral pathology, CRP does not increase much, but in the case of a bacterial infection it can increase several times. Also, a high concentration of C-reactive protein may indicate malignancy, injury, or necrosis (death) of tissue.
CRP analysis plays an important role in the diagnosis of atherosclerosis. If the level of protein in the plasma increases, then we can talk about the pathology of the vascular walls and the onset of the inflammatory process. Additional diagnostics will reveal what kind of disease is developing: stroke or heart attack, coronary artery disease, hypertension, atherosclerosis, etc.
In newborns, liver function is insufficient, so the level of C-reactive protein may not increase even during acute inflammatory processes and sepsis (blood infection). Antibacterial treatment in infants should be initiated when CRP concentrations exceed 12 mg/L.
Indications
A referral for the determination of C-reactive protein can be carried out by an immunologist, infectious disease specialist, internist, pediatrician or general practitioner.
- Prof. examinations of workers of social institutions.
- Comprehensive examination of people of older age groups.
- Analysis of the state of the cardiovascular system after coronary artery bypass surgery.
- Monitoring the effectiveness of treatment of cardiovascular pathologies.
- Monitoring the condition of patients after angioplasty (an operation to restore the lumen of blood vessels).
- Differential diagnosis of inflammatory, bacterial, viral, fungal, parasitic and infectious diseases.
- Monitoring the effectiveness of antibacterial therapy.
- Monitoring the treatment of chronic diseases, preventing relapses.
- Diagnosis and treatment of cancer patients.
- Determining the risk of developing cardiovascular pathologies in diabetics, as well as patients with atherosclerosis and undergoing hemodialysis.
- Control of cardiovascular disease therapy with statins and aspirin.
CRP and osteoporosis
Until now, doctors continue to study what this test shows, in addition to inflammation and cardiovascular risk. Recent studies have proven the connection of C-protein with depletion of calcium reserves and pathologies of bone tissue, that is, osteoporosis. Why does this condition occur, and why is it dangerous?
The fact is that maintaining the inflammatory process requires a large amount of enzymes and microelements, including calcium ions. If it lasts long enough, the amount of these substances in the blood becomes insufficient. In this case, they begin to arrive from the depot. For calcium, bones are such a depot.
A decrease in its concentration in bone tissue leads to its increased fragility. For a person with osteoporosis, even a minor injury is enough for them to experience a complete fracture or “crack in the bone” (incomplete fracture).
At this time, doctors have not determined the exact cutoff for CRP at which the risk of bone changes increases. However, scientists from the NIIR RAMS have found that prolonged excess of this test norm is a serious risk factor for depletion of calcium reserves.
Assessing the risk of heart attack using CRP
What does C-reactive protein indicate if a person does not have inflammatory or oncological diseases? Not long ago, scientists discovered the connection of this substance with the development of vascular complications. This study is especially relevant for people with cardiovascular disease or risk factors.
| Diseases | Risk factors |
|
|
For people with any of these conditions, a CRP level greater than 1 mg/L indicates a risk of a vascular complication. These patients are significantly more likely to have strokes, heart attacks, kidney damage, or heart failure.
- A protein level of 1-3 mg/l indicates an average risk of developing pathologies;
- Exceeding the limit of 4 mg/l demonstrates a high risk of vascular accident.
Preparing for analysis
No special preparation is required from the patient. It is necessary to comply with the standard requirements that apply before donating blood from a vein:
- You need to donate blood on an empty stomach, after 12-14 hours of fasting. As a rule, blood is donated in the morning. The last meal the day before should be 4-6 hours before bedtime. After dinner and until blood donation (the next day), only drinking clean water (not tea, coffee, juices or other drinks) is allowed.
- During the day before donating blood, you should refrain from drinking alcoholic beverages (including beer). Heavy physical activity is also undesirable.
- Your doctor may tell you to stop taking certain medications 1-2 days before donating blood (if possible). If it is impossible to cancel the medicine, then the decoding of the received data is done with a correction for this circumstance.
- You should refrain from smoking 1-3 hours before donating blood. Also avoid stress, anxiety, fast climbing stairs and any heavy physical activity.
Important: what can affect the result
Certain circumstances may distort the results of the study. You risk receiving false data if:
- took oral contraceptives the day before;
- are on hormone replacement therapy;
- are taking beta blockers, glucocorticoids, non-steroidal anti-inflammatory drugs or statins;
- recently had intense physical activity;
- you have bad habits that are difficult to give up in order to obtain correct analysis data.
Complexes with this research
For those who are at risk of COVID-19 Diagnosis of diseases complicating the course of coronavirus infection RUB 4,510 Composition
Nutritionist recommends Metabolic status assessment RUB 7,570 Composition
Rheumatoid arthritis Monitoring the effectiveness of treatment and assessing the prognosis of the disease 3,720 R Composition
IN OTHER COMPLEXES
- Anti-aging diagnostics in postmenopause RUB 12,630
- Advanced anti-aging diagnostics in postmenopause RUB 29,230
- Advanced male anti-aging diagnostics RUB 33,710
- Inflammation of the joints 860 R
- Men's check-up No. 1 RUB 18,570
References
- Kishkun, A.A. Immunological and serological studies in clinical practice. - M.: Medical Information Agency, 2006. - 536 p.
- Sarapultsev, P.A., Sarapultsev, A.P. The role of c-reactive protein in the acute phase response in myocardial infarction. Cytokines and inflammation, 2013. - T.12. - No. 4. - P. 18-24.
- Biasucci, M., Liuzzo, G., Colizzi, C. et al. Clinical use of C-reactive protein for the prognostic stratification of patients with ischemic heart disease. Italian heart journal: official journal of the Italian Federation of Cardiology, 2001. - Vol. 2(3). — P. 164-171.
- Russell, A., Cunninghame, G., Shepherd, C. et al. Polymorphism at the C-reactive protein locus influences gene expression and predisposes to systemic lupus erythematosus. Human molecular genetics, 2004. - Vol. 13(1). — P. 137-147.
- Mevorach, D., Mascarenhas, J., Gershov, D. et al. Complement-dependent clearance of apoptotic cells by human macrophages. The Journal of experimental medicine, 1998. - Vol. 188(12).