Home / Cardiologist / Treatment of cardiosclerosis
Cardiosclerosis is a disease of the heart muscle, which is characterized by deformation of the heart valves and replacement of the cardiac muscle tissue with connective tissue. Due to the fact that scar tissue does not participate in heart contraction, the myocardium begins to work with increasing load. The heart muscle gradually increases in size, hypertrophy of the left ventricle develops, and then of other parts of the heart. Over time, the reserves of the hypertrophied myocardium are exhausted, this leads to a decrease in the contractility of the heart (it cannot pump blood normally) and the development of circulatory failure, that is, heart failure.
This is a heart disease that can occur at any age, but against the background of vascular lesions it is observed mainly in middle-aged and elderly patients.
Causes of cardiosclerosis
The basis of atherosclerotic cardiosclerosis is a violation of the lumen of blood vessels with a chronic lack of oxygen and nutrients in the heart muscle.
Cardiosclerosis occurs in people of all ages. However, the reasons that will lead to the replacement of normal heart tissue with connective tissue, depending on age, vary significantly.
- In children, cardiosclerosis is usually the result of inflammatory or dystrophic processes in the myocardium.
- In adults , this is the result of heart disease, metabolic disorders and, to a lesser extent, changes due to inflammatory processes in the myocardium.
The development of cardiosclerosis is caused by:
- myocarditis (inflammation of the heart muscle),
- cardiodystrophy (muscle damage due to disruption of its nutrition),
- coronary heart disease (damage due to impaired blood supply to the myocardium),
- atherosclerosis of the coronary arteries (due to impaired blood flow and nutrition of the myocardium).
Cardiosclerosis against the background of dystrophic processes is formed:
- with excessive physical exertion in professional athletes,
- for endocrine pathology (thyroid disease, obesity, diabetes),
- for disorders of vitamin metabolism and their chronic deficiency,
- with severe anemia and its prolonged course,
- in case of intoxication (alcoholism, toxic industries),
- with amyloidosis (accumulation of a special substance in the tissues of the heart - a gelatinous mass of amyloid),
- in case of impaired iron metabolism with its accumulation in tissues (hemosiderosis).
Cardiosclerosis in coronary heart disease occurs:
- with angina pectoris,
- with myocardial infarction.
Classification
The typification of the pathological process is carried out on one basis. The degree or area of active tissue replacement by scar tissue.
Fine-focal type
Occurs against the background of a recent heart attack. Only if the volume of affected tissue is minimal. The number of scar cells is insignificant. The area is clearly visible, has clear contours and can be conditionally delimited from functionally active tissues.
In the vast majority of cases, the condition does not manifest itself at all. There is no discomfort, complications are extremely rare.
Patients with a similar diagnosis need to be monitored over time. If ischemia is detected, maintenance therapy is indicated. Courses.
Large-focal post-infarction cardiosclerosis
It is defined by the same features as the previous type: the presence of a clearly demarcated area of replacement with connective tissues. One exception is that the affected area itself is much larger.
The prospects for recovery in this case are worse; dynamic observation is continued, but now against the background of ongoing maintenance treatment.
The therapy is permanent, lifelong. If ineffective, the supervision scheme may be changed.
Diffuse cardiosclerosis
It is determined by the prevalence of epithelialization foci throughout the muscle layer. There are no clear areas, scar-type cells are found in cardiac structures.
Usually becomes a consequence of an extensive heart attack or an inflammatory process. Causes severe symptoms.
However, cardiosclerosis itself does not have a clinical picture. It provokes ischemic heart disease, and it is this condition that determines the discomfort in all its diversity.
It is ischemia that causes the death of patients, not the sclerotic changes themselves. A repeated heart attack puts an end to the patient’s life.
Interesting:
Post-infarction cardiosclerosis is not considered an independent diagnosis and does not have a code in ICD-10. However, the process is of great clinical importance.
Taking into account the results of echocardiography, the doctor determines what therapy to carry out and how intensively. Also how often should the patient be re-examined. The prospects for recovery are also subject to assessment.
Development mechanism
All the reasons described above lead to oxygen deficiency in myocardial tissues and the gradual replacement of normal muscle with connective tissue. Areas of this tissue cannot perform their functional load, and the neighboring normal areas take over the work of the heart.
Due to this, their hypertrophy is formed (an increase in muscle size due to active work). But the heart cannot withstand such loads for a long time - the muscles get tired and are again replaced by connective tissue. This tissue stretches, and the cavities of the heart expand, and blood circulation is disrupted. Heart failure develops.
Clinical example
An important stage in compensating for the general condition is the psychological component of the patient and his adherence to treatment.
I would like to give an interesting example from the experience of my colleague. Patient N., 47 years old. Suffered a large-focal myocardial infarction. The diagnosis was made based on an ECG and troponin test. The lower and lateral walls and the apex of the left ventricle were affected. The typical picture of the disease (acute pain syndrome, circulatory disorders) was absent, and therefore, he sought help only 12 hours after the acute thrombosis.
Thrombolytics were ineffective in the long term (more than 4-6 hours), symptomatic therapy was carried out. The patient felt excellent, refused treatment and the prescription of preventive medications, and left the hospital on his own.
After 3 months, he was readmitted to the hospital with severe signs of left ventricular failure. “The diagnosis was made: IHD. Post-infarction cardiosclerosis. CHF III. FC III. Left ventricular aneurysm.” Full life activity was no longer possible. The patient died from cardiac tamponade on the 10th day. If doctors' instructions were followed, this condition could develop only after several years.
Thus, post-infarction cardiosclerosis is a problem faced by almost every person who has suffered a myocardial infarction. It is necessary to understand that the appearance of any signs of cardiac dysfunction that have not previously manifested is an indication for urgent medical help. Only properly selected therapy will ensure a comfortable life.
Types of cardiosclerosis
According to the degree of prevalence of the process, they are distinguished:
- focal lesions (only small areas have connective tissue, essentially these are scars on the heart),
- diffuse lesions (connective tissue progressively replaces large areas of the myocardium).
Cardiosclerosis can also be divided into certain forms:
- primary cardiosclerosis arising against the background of systemic connective tissue diseases,
- post-infarction, occurs at the site of myocardial infarction, where a scar forms.
- myocarditis, occurs against the background of severe inflammation of the muscle, with no damage to the blood vessels of the heart.
- replacement cardiosclerosis, called myofibrosis, occurs when scar tissue forms in place of chronically starving muscle cells (with atherosclerotic damage to blood vessels with a gradual narrowing of their lumen). Connective tissue replaces dying myocardial cells.
Diagnostic procedures
A patient who has suffered a myocardial infarction must be constantly under medical supervision. When the symptoms described above appear, the diagnosis is beyond doubt. The following studies are used to make a diagnosis:
- ECG. Shows disturbances in the functioning of the heart, myocardial defects and contractility disorders.
EchoCG. Deciphering the results of this study is most valuable. Demonstrates the location, the volume of replaced tissue, and also allows you to count the number of ventricular contractions and determine the presence of aneurysmal dilatations.- Radiography. Makes it possible to see the size of the heart and determine whether it is enlarged.
- Scintigraphy. The patient is injected with radioactive isotopes that reach only healthy areas of the myocardium. This allows you to see the microscopically sized affected areas.
- Angiography. Allows you to determine the degree of narrowing of blood vessels and the presence of blood clots in them.
- MRI. Determines the location and size of connective tissue in the myocardium.
The cardiologist needs to carefully examine the patient’s medical history and conduct a detailed interview. An assistant in determining the diagnosis will be the patient’s medical record, which records all the diseases suffered during life. This allows you to predict future complications and prevent them.
Symptoms of cardiosclerosis
Clinical manifestations of cardiosclerosis depend on the degree of spread of connective tissue in relation to healthy myocardial tissue. The more scars, the more pronounced the heart failure and its external manifestations: shortness of breath, swelling, heart rhythm disturbances (atrial fibrillation and extrasystole).
With a common, diffuse form of cardiosclerosis, signs of heart failure occur:
- dyspnea,
- cardiac swelling in the arms and legs,
- cough at night due to congestion in the lungs,
- tachycardia with decreased blood pressure,
- accumulation of fluid in the body cavities - abdominal and thoracic.
Particularly dangerous are complications of advanced cardiosclerosis in the form of
- development of arrhythmias (atrial fibrillation, extrasystole, heart block)
- aneurysms in areas of foci of cardiosclerosis - protrusions of tissue with thinning of the wall and the danger of rupture (heart rupture).
- development of chronic heart failure with impaired blood pumping.
Complications
PICS, causing severe consequences, becomes a common cause of death. These include:
- ischemic cardiomyopathy;
- repeated myocardial infarction “along the scar”;
- ventricular tachycardia;
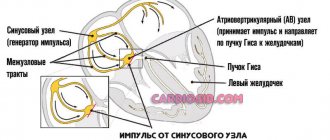
- conduction disturbances such as atrioventricular block;
- pulmonary edema and acute left ventricular failure;
- sudden cardiac death.
If emergency care is not provided in a timely manner, any of the listed conditions leads to death.
Such patients are always in intensive care units or intensive care wards in cardiology departments.
Diagnostics
In addition to anamnesis indicating heart disease and other pathologies, the doctor is important to examine and typical complaints of patients. But the main methods for diagnosing cardiosclerosis are:
- Ultrasound of the heart with assessment of its contractility, structure, size and shape,
- Dopplerography of vessels with assessment of blood flow in the coronary vessels, areas of myocardial ischemia, condition of the heart valves, etc.,
- ECG with changes in the conduction system, the presence of infarctions of fresh origin or in the scar stage with their exact localization.
- X-ray of the heart from several projections, for a visual assessment of its size and condition.
- CT and MRI of the heart with detection of areas of altered myocardium.
Prevention
No methods of prevention have been developed as such. It is enough to adhere to clinical recommendations that are common to all risk groups for developing cardiovascular pathologies.
- Refusal of bad habits and behavioral stereotypes. Smoking, alcohol, drugs will sooner or later play a cruel joke.
- Normalization of the rest regime. Approximately 8-9 hours per night. Not worth it anymore.
- Salt no more than 7 grams per day.
- Regular examinations with a cardiologist. Once a year. If the patient is at risk - every 6 months.
- Hiking. No sports or excessive physical activity.
- Stress and overheating are eliminated.
- Proper nutrition.
- Timely treatment of conditions that can lead to a heart attack. For example, atherosclerosis, arterial hypertension and others.
Treatment of cardiosclerosis
The diagnosis and treatment of cardiosclerosis is carried out by therapists and cardiologists, sometimes they are joined by cardiac surgeons - if it is necessary to correct changes through operations.
Unfortunately, there are no medications or treatment methods that would force connective tissue to transform back into muscle tissue. Therefore, treatment is aimed at maintaining the remaining myocardium in working condition and stopping the proliferation of connective tissue.
In addition, with cardiosclerosis, it is necessary to treat existing heart disorders caused by the disease process:
- therapy of myocarditis, myocardial dystrophy and atherosclerosis,
- treatment aimed at eliminating myocardial ischemia,
- taking medications to normalize heart rhythm (cordarone, amiodarone, rhythmonorm and others),
- drugs for activating and improving metabolic processes in the myocardium (korglykon, dopamine, Simdax, Actovegin, Cardionate and others).
- dietary restrictions - reduced amount of salt and sugar, low-carbohydrate diet, reduced consumption of cholesterol-containing foods to prevent atherosclerosis,
- limiting stress when the heart muscle is overstrained,
- surgical correction of aneurysms, implantation of pacemakers for rhythm disturbances, etc.
Treatment Options
It is not possible to cure this pathology. Therefore, the goals of the therapy are:
- prevention of sudden cardiac death;
- prevention of life-threatening arrhythmias;
- preventing the formation of ischemic cardiomyopathy;
- control of blood pressure and heart rate;
- improving the quality of life of patients;
- increasing the survival rate of patients.
Such goals are achieved by assigning a whole range of activities, including:
- non-medicinal component;
- conservative therapy;
- surgical treatment.
The first point includes general recommendations on maintaining a healthy lifestyle, giving up cigarettes and alcohol.
The drug block consists of the use of the following groups of drugs:
- beta-blockers: Metoprolol, Carvedilol, Bisoprolol;
- ACE inhibitors: Lisinopril, Enalapril;
- sartans: Valsartan;
- antiarrhythmic drugs: Cordarone, Sotalol;
- diuretics: Diuver, Furosemide, Lasix;
- antagonists of mineralococticoid hormones: Veroshpiron, Spironolactone, Inspra;
- lipid-lowering drugs: Atorvastatin, Rosuvastatin;
- disaggregants: Aspirin Cardio, Cardiomagnyl, Acetylsalicylic acid, Plavix, Lopirel, Zilt;
- antihypoxants: Preductal MV, Predizin;
- Omega-3 polyunsaturated fatty acids: Omacor.
The required treatment regimen is selected by the attending physician.
Surgical intervention is indicated when conservative measures are ineffective and gross changes in the myocardium are progressing.