general description
Supraventricular tachycardia
is a common type of arrhythmia that originates in a zone located above the ventricles of the heart. The main features of this type of arrhythmia are a sharp increase in heart rate and the persistence of a pathological rhythm for a certain period of time. Currently, this heart disorder is very common in people over 20 years of age.
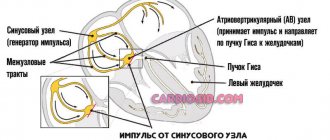
There are five main types of supraventricular arrhythmias, different in etiology and pathophysiology: atrioventricular nodal tachycardia, atrioventricular tachycardia, atrial tachycardia, intraatrial tachycardia, sinoatrial reentrant tachycardia (it should be noted that such types of supraventricular arrhythmias as atrial fibrillation and atrial flutter, as a rule, are worth apart from this group).
At risk:
men and women regardless of age
1.What is supraventricular tachycardia?
Supraventricular tachycardia (or as it is also called paroxysmal supraventricular tachycardia, paroxysmal tachycardia or simply tachycardia
the heart beats very fast
at times . This can happen for various reasons - due to physical activity, high temperature, stress. A heart beating too quickly can be dangerous.
During an attack of tachycardia
The electrical system of the heart does not work properly and causes the heart to beat very quickly. The heart rate is at least 100 beats per minute and can even reach 300 beats per minute. After taking medication or just on its own after a while, the heart usually returns to its normal rhythm - from 60 to 100 beats per minute.
Cardiac tachycardia can begin and end quickly, and you may not even feel any unpleasant symptoms. Tachycardia becomes a problem when it occurs frequently, lasts a long time, or causes some kind of discomfort.
A must read! Help with treatment and hospitalization!
Symptoms of supraventricular tachycardia
- cardiopalmus;
- severe dizziness, lightheadedness, fainting;
- feeling of lack of air and difficulty breathing, chest pain;
- pronounced decrease in blood pressure;
- Feelings of fear, panic and anxiety may often be present.
More often, an attack of arrhythmia lasts up to 1 hour (usually 5-20 minutes), attacks can be repeated with varying frequencies. Some patients can independently cope with the next attack by taking certain medications (“a pill in the pocket”) or so-called vagal tests (pressing on the eyeballs, wiping with cold water, etc.)
It is also worth remembering that some types of arrhythmia have absolutely identical symptoms, but unlike supraventricular rhythms, they are life-threatening. That is why a full examination is necessary in order to determine the type of arrhythmia and decide on the need for treatment.
Paroxysmal tachycardia
The question of treatment tactics for patients with paroxysmal tachycardia is decided taking into account the form of arrhythmia (atrial, atrioventricular, ventricular), its etiology, frequency and duration of attacks, the presence or absence of complications during paroxysms (heart or cardiovascular failure).
Most cases of ventricular paroxysmal tachycardia require emergency hospitalization. The exception is idiopathic variants with a benign course and the possibility of rapid relief by administering a certain antiarrhythmic drug. In case of paroxysm of supraventricular tachycardia, patients are hospitalized in the cardiology department in case of development of acute cardiac or cardiovascular failure.
Planned hospitalization of patients with paroxysmal tachycardia is carried out in case of frequent, > 2 times a month, attacks of tachycardia to conduct an in-depth examination, determine treatment tactics and indications for surgical treatment.
The occurrence of an attack of paroxysmal tachycardia requires emergency measures on the spot, and in case of primary paroxysm or concomitant cardiac pathology, a simultaneous call to the emergency cardiological service is necessary.
To relieve paroxysm of tachycardia, they resort to vagal maneuvers - techniques that have a mechanical effect on the vagus nerve. Vagal maneuvers include straining; Valsalva maneuver (an attempt to vigorously exhale with the nasal cleft and oral cavity closed); Aschner's test (uniform and moderate pressure on the upper inner corner of the eyeball); Chermak-Hering test (pressure on the area of one or both carotid sinuses in the area of the carotid artery); an attempt to induce a gag reflex by irritating the root of the tongue; rubbing with cold water, etc. With the help of vagal maneuvers it is possible to stop only attacks of supraventricular paroxysms of tachycardia, but not in all cases. Therefore, the main type of assistance for developing paroxysmal tachycardia is the administration of antiarrhythmic drugs.
As an emergency treatment, intravenous administration of universal antiarrhythmics is indicated, effective for any form of paroxysms: novocainamide, propranoloa (obsidan), ajmaline (gilurythmal), quinidine, rhythmodan (disopyramide, rhythmileka), ethmosin, isoptin, cordarone. For prolonged paroxysms of tachycardia that cannot be controlled by medications, electrical pulse therapy is used.
In the future, patients with paroxysmal tachycardia are subject to outpatient monitoring by a cardiologist, who determines the volume and regimen of antiarrhythmic therapy. The prescription of anti-relapse antiarrhythmic treatment of tachycardia is determined by the frequency and tolerability of attacks. Continuous anti-relapse therapy is indicated for patients with paroxysms of tachycardia that occur 2 or more times a month and require medical assistance to stop them; with more rare but prolonged paroxysms, complicated by the development of acute left ventricular or cardiovascular failure. In patients with frequent, short attacks of supraventricular tachycardia, self-limiting or with the help of vagal maneuvers, the indications for anti-relapse therapy are questionable.
Long-term anti-relapse therapy of paroxysmal tachycardia is carried out with antiarrhythmic drugs (quinidine bisulfate, disopyramide, moracizine, etacizine, amiodarone, verapamil, etc.), as well as cardiac glycosides (digoxin, lanatoside). The selection of the drug and dosage is carried out under electrocardiographic control and monitoring the patient’s well-being.
The use of β-blockers for the treatment of paroxysmal tachycardia can reduce the likelihood of the transition of the ventricular form to ventricular fibrillation. The most effective use of β-blockers in combination with antiarrhythmic drugs, which allows you to reduce the dose of each drug without compromising the effectiveness of the therapy. Prevention of relapses of supraventricular paroxysms of tachycardia, reducing the frequency, duration and severity of their course is achieved by constant oral administration of cardiac glycosides.
Surgical treatment is resorted to in particularly severe cases of paroxysmal tachycardia and ineffectiveness of anti-relapse therapy. As a surgical aid for paroxysms of tachycardia, destruction (mechanical, electrical, laser, chemical, cryogenic) of additional impulse pathways or ectopic foci of automatism, radiofrequency ablation (RFA of the heart), implantation of pacemakers with programmed modes of paired and “capturing” stimulation, or implantation of electrical defibrillators.
Diagnostics
To confirm the diagnosis and clarify the severity of the disease, additional diagnostic methods are needed:
- taking an electrocardiogram (ECG) at rest and during the next attack of arrhythmia
- 24/7 ECG recording is performed (Holter ECG monitoring)
- according to indications, further examination is required to exclude the symptomatic nature of arrhythmic syndrome
- according to indications, it is possible to conduct an endocardial electrophysiological study of the heart in a hospital setting
2. Causes of tachycardia
Most cases of cardiac tachycardia are caused by defects in the electrical connections of the heart. But what causes these problems is still not known.
Tachycardia can be a side effect of certain medications, such as those taken to treat heart or lung conditions.
Some types of tachycardia can be inherited, or be a consequence of lung diseases - COPD or pneumonia.
Visit our Cardiology page
ESC 2021 recommendations for the management of patients with supraventricular tachycardias: review of changes
Presented at the European Congress of Cardiology in August of this year, the recommendations for the management of patients with supraventricular tachycardias were only the second edition of the document since their release in 2003. The unusually long period of time that elapsed before the first update of the document was due to the extremely small number of randomized clinical trials in this area .
The recommendations are devoted to the diagnosis and treatment of tachycardia (atrial contraction rate > 100 per minute), the development mechanism of which involves tissues of the His bundle and any structures located “above” it, with the exception of atrial fibrillation, approaches to the diagnosis and treatment of which are discussed in a separate document.
Since 2003, the guidelines have undergone significant changes, affecting both drug therapy and interventional methods of treating arrhythmias. Thus, fundamentally new sections dedicated to the management of special groups of patients have appeared. They were: supraventricular tachycardia in adult patients with congenital heart defects, supraventricular tachycardia in pregnant women, tachycardia-induced cardiomyopathy, supraventricular tachycardia in athletes, supraventricular tachycardia and driving restrictions.
Now, for patients with sinus tachycardia, after excluding reversible causes, if symptoms are present, therapy with ivabradine or its combination with beta-blockers is recommended, while calcium channel blockers and catheter ablation are not mentioned at all in this section. However, neither ivabradine nor beta-blockers, nor other drugs are recommended (IIb) for the initial treatment of postural orthostatic tachycardia syndrome. And the position on salt and fluid intake in this syndrome changed its class from IIa to IIb.
Given the development of catheter methods for diagnosing and treating arrhythmias associated with additional pathways, electrophysiological testing for the purpose of risk stratification is indicated even for asymptomatic patients with the presence of ventricular pre-excitation (delta waves) on the ECG. For athletes, the recommendation was grade I, while for other patients it was grade IIa. Catheter ablation in these patients is recommended (Class I) if high-risk features are present.
For the acute treatment of tachycardias with a narrow QRS complex in stable hemodynamics in the absence of an accurate diagnosis after performing vagal maneuvers, in addition to verapamil and diltiazem, beta-blockers can now be used - all of these groups of drugs have a class IIa recommendation, while amiodarone and digoxin are not mentioned at all.
According to the new document, amiodarone should not be used (class IIb) and in the treatment of tachycardia with a wide QRS complex in the case of stable hemodynamics and in the absence of an accurate diagnosis.
For the treatment of focal atrial tachycardia in the acute period after an attempt to stop it with adenosine, it is proposed to use calcium channel blockers or beta-blockers (class IIa), while amiodarone received class IIb for this variant of supraventricular arrhythmia.
This downgrade of amiodarone is due to the proarrhythmogenic potential of the drug and the availability of safer drugs for most of the clinical situations discussed. It is especially emphasized that amiodarone should not be used (class III) in the treatment of atrial fibrillation in combination with the presence of ventricular preexcitation syndrome.
The mainstay of treatment for symptomatic or AV nodal and AV reentrant tachycardias, as well as for high-risk features associated with the presence of an accessory pathway, is catheter ablation (Class I). Catheter ablation is now recommended (Class IIa) for asymptomatic patients in the presence of preexcitation and left ventricular dysfunction due to electrical dissociation.
The new section on the diagnosis and treatment of tachycardia-induced cardiomyopathy emphasizes that such cardiomyopathy is one of the few reversible causes of heart failure and severe dilatation of the heart chambers. The main treatment for cardiomyopathy is catheter ablation (class I), and if it is impossible or ineffective, beta-blockers (class I).
Interestingly, the section on atrial flutter notes that the risk of thromboembolic complications in the presence of isolated flutter without fibrillation is probably lower than in the latter. It is emphasized that in the case of their combination, the decision to make a decision on prescribing anticoagulant therapy should not differ for that in the case of the presence of only atrial fibrillation, however, with isolated atrial flutter, clear criteria for starting therapy are not identified.
More detailed information about the text of the recommendations can be found on the website of the European Society of Cardiology: www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Supraventricular-Tachycardia
Sources:
1. Brugada J, Katritsis D, Arbelo E, Arribas F, Bax J, Blomstrom-Lundqvist C, et al. EurHeartJ. 2021. doi: 10.1093/eurheartj/ehz467. .
4. Treatment of the disease
When cardiac tachycardia does not cause any serious symptoms or deterioration in well-being, it usually does not require treatment. But if tachycardia causes various health problems, the doctor will prescribe the necessary treatment for tachycardia. To treat an attack of tachycardia, medications may be recommended that will need to be taken during an attack of tachycardia. In addition, the doctor will tell you how you can slow down your heart rate without medications.
. This can be done, for example, by coughing, gagging, or putting your face in ice water.
If this does not help, and the tachycardia is quite severe, you need to seek emergency help. Doctors will stop the tachycardia using strong, fast-acting medications, and in particularly serious cases, perform an electrical cadioversion
, which uses an electrical current to slow the heart rate.
If episodes of tachycardia occur frequently, you may need to take daily medications to prevent attacks or slow your heart rate. Another way to treat tachycardia is surgery.
destruction of a tiny section of the heart that causes tachycardia.