Diffuse toxic goiter (DTZ, Graves-Bazedow disease) is an autoimmune disease characterized by persistent pathological hypersecretion of thyroid hormones and, as a rule, a diffusely enlarged thyroid gland (thyroid gland).
Goiter is a pathological enlargement of the thyroid gland, without specifying its functional state. The normal volume of the thyroid gland, determined by ultrasound, should not exceed 25 ml in men and 18 ml in women. Palpation of the thyroid gland, being the main method of clinical examination of the thyroid gland, does not allow determining its volume and has no independent significance for the diagnosis of goiter.
Thyrotoxicosis is not a disease, but a clinical syndrome caused by persistent pathological hypersecretion of thyroid hormones. The term hyperthyroidism means an increase in the functional activity of the thyroid gland, which can be pathological (thyrotoxicosis) and physiological (for example, during pregnancy). The severity of thyrotoxicosis is assessed by the clinical picture and the presence of complications associated with the disease (atrial fibrillation, dystrophic changes in internal organs, thyrotoxic psychosis, etc.).
The cause of thyroid disease is a defect in the immune system, leading to the formation of antibodies that stimulate the production of excess amounts of thyroid hormones.
Antibodies are proteins produced by cells of the immune system - lymphocytes. These antibodies are able to bind to TSH receptors (a hormone that normally regulates thyroid function) and, like a wolf in sheep's clothing, uncontrollably stimulate the production of thyroid hormones. The thyroid gland simply “does not understand” who is stimulating it. Hence they received the name – antibodies to TSH receptors (ATrTSH).
Circulating antibodies are detected in 50% of relatives of a patient with DTG. Sometimes there is a combination with other autoimmune diseases (chronic adrenal insufficiency, type 1 diabetes, etc.). Women get sick 5-10 times more often than men. As a rule, DTZ manifests itself in young and middle age.
When should you take the Thyroid Function Test?
1. Reduced or increased TSH level;
2. Control study for detected diffuse toxic goiter (1.5 - 2 years, 1 - 3 times a month);
3. Goiter;
4. Clinical picture of hypothyroidism or thyrotoxicosis.
1. Diagnosis of subclinical stages of primary hypo- and hyperthyroidism. Conditions associated with delayed mental and sexual development in children, cardiac arrhythmias, myopathy, idiopathic hypothermia, depression, alopecia, infertility, amenorrhea, impotence and decreased libido, hyperprolactinemia;
2. Goiter;
3. Monitoring of replacement therapy for primary hypothyroidism;
4. Screening of pregnant women in the first trimester to identify hidden hypothyroidism, potentially dangerous to the fetus;
5. Monitoring the condition in case of detected hypothyroidism (lifelong 1-2 times/year);
6. Monitoring the condition of detected diffuse toxic goiter (1-3 times/month for 1.5-2 years).
Differential diagnosis of thyroid diseases;
2. Control study for isolated T3 toxicosis.
“Thyroid” causes of a “restless” heart
When the heart is “out of place,” we are usually talking about experiences of a psychological nature. But, if the heart is pounding with or without reason, the cause of the condition is no longer only in emotions, but first on the list of “heart provocateurs” are thyroid hormones.
Will make you worry not only the heart
Arrhythmia is a group of heart rhythm disorders that have a paroxysmal nature and can occur both after exercise and at rest.
During such an “attack,” the heart begins to beat faster or intermittently, and the minute volume of blood passing through the heart normally decreases significantly. Blood pressure “falls”. And patients at such moments may experience shortness of breath, headaches, dizziness and even lose consciousness.
The causes of this pathology may be hidden in defects in the conduction system of the heart itself, changes in the volume and rheological properties of the blood (for example, with dehydration or anemia) or an excess of thyroid hormones.
At the same time, T4 (or thyroxine) makes not only the heart “nervous,” because the hormone is a stimulator of absolutely all metabolic, energy and recovery processes in the body. And among the common symptoms of hyperthyroidism:
- general agitation and fussiness,
- unmotivated anxiety and irritability,
- insomnia,
- exhaustion due to normal nutrition,
- increase in body temperature,
- sweating, even at normal room temperature,
- increased thirst, frequent urination,
- increased pressure,
- redness of the skin and hair loss,
- Spastic digestive disorders (abdominal pain, diarrhea, constipation, etc.)
- and others.
Symptoms increase unnoticed, each time demonstrating greater resistance to standard treatment regimens.
As for the heart, then:
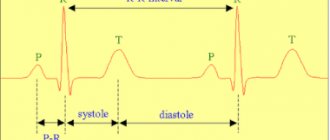
- with mild hyperthyroidism, the heart rate during an “attack” usually does not exceed 100 beats/minute;
- with moderate severity - on average, 120-140;
- and a severe form of pathology is accompanied by tachycardia above 140 beats.
Such arrhythmia, as already noted, is resistant to the action of conventional “heart” drugs. And, in the absence of correction of thyroid (“thyroid”) hormones, it can lead to the development of fibrillation and cardiac arrest.
When there is too much thyroxine
Hyperthyroidism, or excess thyroid hormones, can result from:
- excessive independent activity of the gland (diffuse toxic or nodular goiter, overdose of iodine-containing drugs)
- or an excess of the pituitary hormone TTT, which controls the activity of the gland.
In the first case, the cause of excess production of hormones may be either in the thyrocytes themselves (thyroid cells) or in stimulating antibodies. But the second - in most cases, in the pathology of the pituitary gland.
The exact cause of the disease can only be identified with the help of blood tests, ultrasound of the gland (with a biopsy in some cases), as well as CT or MRI, if necessary.
When is it time to see an endocrinologist?
The presence of arrhythmia along with several of the listed symptoms is a good reason to check the “health” of the thyroid gland. And in this case you will need:
- blood test for TSH,
- and free
- as well as antibodies to TSH receptors.
A decrease in TSH, even against the background of still normal or slightly elevated T4 and T3, indicates latent (subclinical hyperthyroidism); and if they significantly exceed the normative limits - about the clinical form (requiring immediate treatment) of the disease.
An increase in T4 and T3 simultaneously with TSH is a sign of pituitary pathology.
Detection of antibodies in the presence of symptoms is evidence in favor of Graves' disease.
Hypothyroidism and the heart
Cardiologist of the Cardiology Department No. 2 Subotka T.A.
Heart damage in hypothyroidism is caused by a decrease in the content of thyroid hormones in the body, which can occur as a primary process or result from surgical treatment of thyroid diseases (total or subtotal resection) or treatment with radioactive iodine. In these cases, the activity of metabolic processes in the heart muscle is significantly suppressed, and the work of the heart decreases.
Heart damage is most severe in primary hypothyroidism. The intensity of oxidative phosphorylation decreases, protein synthesis slows down, and oxygen absorption in the myocardium decreases. Developing disorders lead to a decrease in myocardial contractility associated with dysfunction of contractile proteins. With hypothyroidism, anemia often develops, aggravating the course of MCD.
Clinical picture and diagnosis . Patients complain of shortness of breath associated with minimal physical activity, swelling of the face and legs. Pain in the heart area occurs in less than 50% of cases. The presence of general manifestations of hypothyroidism is characteristic: muscle weakness, physical inactivity, mental retardation, drowsiness. The boundaries of the heart are significantly displaced due to myocardial edema and the presence of fluid in the pericardial cavity. The heart sounds are muffled, the activity is rhythmic, bradycardia and a small slow pulse are characteristic.
Due to the disturbance of lipid metabolism that occurs with hypothyroidism, it is quite difficult to carry out a differential diagnosis with ischemic heart disease, especially against the background of the presence of angina-type pain syndrome. When carrying out differential diagnosis of these conditions, the following signs must be taken into account:
Manifestations of hypothyroidism are characterized by:
- pain in the heart area like cardialgia
- negative results of stress tests
- the presence of sinus bradycardia;
- absence of acrocyanosis;
- localization of swelling on the face and legs
- absence of pits when pressing in the area of edema
- absence of liver enlargement, congestion in the lungs, cardiac asthma (in the initial stages of the disease)
- low absorption of iodine-131;
- decreased levels of thyroid hormones in the blood;
- Hormone replacement therapy gives positive results.
Treatment . It is carried out against the background of hormone replacement therapy with thyroid hormones with careful selection and control of the dose. Inadequate doses can provoke attacks of angina pectoris and aggravate the symptoms of circulatory failure.
Types of tachycardia
Tachycardia as such is divided into two groups:
- physiological , which is not considered a pathology and is a consequence of physical activity, and also occurs in preschool children, and then in adolescents during the period of hormonal changes. In addition, this “safe” tachycardia can also be caused by some external factors in addition to physical activity - stress, emotional arousal, heat, coffee, alcohol, some medications, sudden changes in body position, etc. In all these cases, a certain amount of adrenaline is released into the blood, which and serves as a “trigger” for increased heart rate;
- pathological tachycardia is already a disease, and it may be associated not necessarily with the cardiovascular system, but also with other systems of the body. Such tachycardia, if not detected in a timely manner, leads to various organic pathologies, including those related to the cardiovascular system - heart attacks, strokes.
The pathological form of the disease is also divided into types depending on the parts of the heart that “accelerate” its work - the atria (atrial tachycardia) and the ventricles (ventricular tachycardia). A subtype of ventricular tachycardia is sinus tachycardia.
Journal "Emergency Medicine" 1(2) 2006
Heart pathology is often the leading cause of thyroid disease in the clinic, accompanied by its dysfunction (hypo- or hyperthyroidism), often leading to loss of ability to work and decreased quality of life. The significance of thyroid pathology especially increases when it is combined with other diseases of internal organs and, above all, with cardiovascular disorders (hypertension, cardiosclerosis, heart defects, arrhythmias), the course of which it aggravates.
Among the main cardiovascular manifestations in patients with thyrotoxic heart is tachycardia, which occurs in 42-73% of patients. The second place in frequency is occupied by atrial fibrillation (AF) - it is recorded in 9-23% of patients with thyrotoxicosis (in the general population - in 0.4-1% of cases). In addition to these heart rhythm disorders, extrasystoles (5-7%), paroxysmal tachycardia (0.2-3.3%) and atrial flutter (in 1.4% of cases) also occur. The incidence of AF increases with age, reaching 25-67% after 60 years, and is more common among men, as well as in the presence of T3 thyrotoxicosis.
The high incidence of atrial fibrillation and flutter, which cardiologists and endocrinologists encounter in their practice, led to a substantiated recommendation from the working group on cardiac arrhythmia of the Ukrainian Association of Cardiologists (2005) to assess thyroid function in all patients with newly diagnosed AF/AFL, and also with difficult control of ventricular rate and the use of cordarone.
At the onset of the disease with diffuse toxic goiter (DTG), AF is paroxysmal in nature, but later, with a long course of this disease and the formation of metabolic cardiomyopathy, it becomes a permanent form, especially in elderly patients in the presence of concomitant cardiac pathology and developed heart failure as a result of concomitant pathology , which aggravates the severity and course of the resulting hemodynamic changes.
Mechanisms of development of arrhythmias
The basis for the development of cardiac arrhythmia and, above all, AF/AFL in patients with DTG are various pathophysiological changes that develop under the influence of the action of thyroid hormones, which secretes 2 types of hormones (T3 and T4). The physiological effect of hormones is associated to a greater extent with triiodothyronine (T3), which is 4-5 times more active than thyroxine (T4). About 100 µmol of thyroxine and 5 µmol of triiodothyronine are secreted per day. 99.96% of these hormones are in protein-bound form and are deposited. The biological activity of thyroid-stimulating hormones (TG) is carried out due to the remaining 0.4% of these hormones.
The main effects of TH are realized at the level of the cell nucleus, changing the expression of the genome, as well as outside the genome through its effect on the plasma membrane of the cell (regulating the flow of substrates and cations into and out of the cell), cytoplasm, and mitochondria (affecting oxidative metabolism).
The mechanisms of non-genomic effects may involve components of cell signaling systems: phospholipid or Ca-dependent protein kinase, cAMP-dependent protein kinase, calmodulin-Ca complex. Non-genomic effects of TG include: regulation of the intracellular level of certain ions and their distribution within the cell.
Diseases of the thyroid gland (TG) are manifested by qualitative or quantitative changes in the secretion of hormones, an increase in the size of the organ (goiter), or both. Excessive secretion of hormones causes hypermetabolism and other signs of a syndrome called thyrotoxicosis.
The clinical diagnosis of hyperthyroidism is confirmed by data on an increase in the blood serum concentration of thyroid hormones or one of them.
Impaired thyroid function is also accompanied by a toxic thyroid adenoma (adenomatous node), which produces an excess amount of thyroid hormones, mainly triiodothyronine, which causes the development of triiodothyronine thyrotoxicosis. This form of thyrotoxicosis is manifested by tachysystolic attacks of AF, occurring as a paroxysm against the background of a normal rhythm or bradycardia, and is accompanied by an increased level of TG concentration in the blood during the paroxysm. Arrhythmia worsens the quality of life of such patients and may be the main reason for visiting a doctor. With a long course of the disease, AF becomes permanent.
A relationship was identified between the frequency of AF, the type of hormone, the amount of which increases, and the nature of the morphological changes in the thyroid gland. It was found that with an increase in the amount of T3, atrial fibrillation is observed in 36% of those examined, with an increase in T4 - in 13%, and with an increase in the level of both hormones - in 21% of cases. AF is most often observed in patients with solitary thyroid adenoma (43%). In patients with nodular goiter, the frequency of AF is 33%, in multinodular goiter - 18%, and in diffuse toxic goiter - 10% of cases.
The pathogenesis of arrhythmias in thyrotoxicosis has not been fully studied, and currently the following factors are considered important in their development in thyrotoxicosis: the toxic effect of TG on the myocardium, an increase in the sympathetic tone of the autonomic nervous system, and a decrease in intracellular potassium (Table 1). Depletion of the normotopic function of the sinus node due to a decrease in the reserves of the substrate of automatism, acetylcholine, also leads to the development of sick sinus syndrome and the transition to a pathological rhythm.
Under the influence of TG, oxidative phosphorylation is uncoupled, which leads to disruption of the synthesis of energy-rich ATP molecules, a sharp compensatory increase in metabolism, and an increase in tissue demand for oxygen. Protein synthesis and enzyme activity, oxygen consumption and calcium levels in cells increase, which is carried out by nuclear and extranuclear mechanisms. As a result, the transport of amino acids, calcium and glucose across the cell membrane changes. This mechanism is one of the main mechanisms underlying increased myofibril contractility and cardiac hypertrophy. Left ventricular hypertrophy in DTG is moderate and is combined with dilatation of the heart cavities.
In addition, dystrophic lesions of the atria play a role in the origin of AF/AFL in thyrotoxicosis. Electrocardiographic signs of right atrium hypertrophy, often combined with dilatation, were recorded in 30.5% of patients with thyrotoxicosis, left atrial hypertrophy - in 13.7%, hypertrophy of both atria - in 11.8% of patients. The expansion of the atria, their increased excitability, combined with the ease of occurrence of functional blockades due to the heterogeneity of different parts of the myocardium underlie the re-entry mechanism.
In addition to the inotropic effect, the direct chronotropic effect of excess TG on the conduction system of the heart has been confirmed: due to disturbances in energy processes and changes in the potassium-sodium pump, spontaneous diastolic depolarization in the cells of the sinus node is accelerated, which predisposes to more frequent generation of impulses in it.
Experimental studies have proven that in hyperthyroidism there is an increase in the sensitivity of the sympathoadrenal system, mediated by an increase in the number of b-adrenergic receptors and guanine nucleotide-regulating protein. Beta-adrenergic receptors increase almost 2-fold in the sinoatrial node compared to the surrounding myocytes, of which the majority (75%) are beta-1 receptors. Beta-2 receptors are the predominant species in non-myocyte vascular cells. In cardiac tissue, the beta 1 adrenergic receptor gene is thought to be sensitive to T3, while the beta 2 receptor gene is minimally influenced by it.
Hyperfunction of the heart and increased adrenergic influences on it cause loss of potassium inside the cell, which is one of the causes of rhythm disturbances in diffuse toxic goiter.
In thyrotoxicosis, there is functional heterogeneity of different parts of the myocardium. Any additional impact that increases this heterogeneity can cause complete discoordination of the activity of different parts of the heart muscle, which is manifested by various arrhythmias.
A long-term discussion about what underlies atrial fibrillation and flutter - the re-entry mechanism or the focal formation of impulses - led to the conclusion about the simultaneous existence of frequent focal impulses with circular movements of the excitation wave.
Ventricular forms of rhythm disturbances in thyrotoxicosis are rare, mainly when thyrotoxicosis is combined with cardiovascular diseases, and persist when euthyroidism is achieved. The higher sensitivity of the atria to the arrhythmogenic effects of TH compared to the ventricles may be explained by a higher density of beta-adrenergic receptors in the atrial tissue or by autonomous different innervation of the atria and ventricles.
The effect of thyroid hormones on the vascular system has also been established. Researchers observed in a cell culture the rapid relaxation of vascular smooth muscle cells of the heart under the influence of T3. It has been revealed that T3 can directly regulate vascular resistance, reducing it, which reflexively leads to changes in blood pressure and cardiac output, and consequently, pre- and afterload. These changes are the earliest. In response to an increase in TG, peripheral resistance decreases and constriction of venous vessels increases, as a result of which the reverse flow of blood into the right atrium increases, diastolic pressure decreases and cardiac output changes reflexively.
Treatment of heart rhythm disorders
Treatment of cardiac arrhythmias should be aimed primarily at eliminating thyrotoxicosis and compensating for the activity of the cardiovascular system.
Compensation for thyrotoxicosis is achieved by using antithyroid drugs (Mercazolil, Timazol, Methimazole). When using the latter, a chemical blockade of hormone synthesis occurs. This effect persists only during the period of drug administration or until the onset of spontaneous remission and does not prevent exacerbations. More radical treatment is surgery or radioiodine therapy.
It is known that in 60-90% of patients with DTG and AF/AFL, normal sinus rhythm is restored with adequate thyreostatic therapy, even without the use of antiarrhythmic drugs or in the postoperative period after subtotal resection of the thyroid gland.
To eliminate the increased sympathetic influence on the heart, adrenergic antagonists (propranolol, obzidan) are widely used, which do not directly affect the secretion of TG, but realize a clinical effect by blocking the influence of the sympathetic nervous system on the heart, which leads to a decrease in cardiac work and a decrease in myocardial oxygen demand . In addition, these drugs affect the metabolism of TG, promoting the conversion of T4 into the inactive form of T3 - reverse T3. It has been established that large doses of propranolol (more than 160 mg per day), by inhibiting 51-monodeiodinase, can also reduce the concentration of T3 in the blood plasma by almost 30%. For patients with a relative contraindication to the prescription of b-blockers, it is better to prescribe cardioselective drugs: betaxolol (Locren), atenolol, metoprolol, despite the fact that they very weakly reduce the level of T3 in the blood plasma. Treatment with b-blockers is carried out until euthyroidism is achieved, and then gradually withdrawn, if necessary, maintenance dosages are prescribed.
Indications for the use of beta-blockers are persistent tachycardia, resistant to treatment with thyreostatics; heart rhythm disturbances in the form of ES, AF, angina pectoris; HF associated with increased force of heart contractions. As an additional therapeutic agent, beta blockers are useful mainly during the treatment period, when a reaction to antithyroid drugs or radioiodine has not yet manifested, as well as during thyrotoxic crisis and in preoperative preparation.
The positive cardiovascular effect of beta-blockers used in combination with thyreostatic drugs is higher than with monotherapy, and at the same time they make it possible to reduce the dose of the latter.
A very important and difficult task is the treatment of AF/AFL against the background of thyrotoxicosis, since they most often occur at a severe stage of thyrotoxic heart, when there is a decompensated hemodynamic state (cardiac dysfunction, HF), and a long course of the disease, and these patients in most cases need in surgical treatment after conservative preparatory treatment.
Atrial fibrillation is a severe rhythm disorder that adversely affects intracardiac and general hemodynamics and is associated with an increased risk of death. The mortality rate for this rhythm disorder is 2-2.5 times higher than that among patients with sinus rhythm. AF significantly (5-7 times) increases the risk of thromboembolic complications, provokes the development of HF or aggravates its course.
If in the paroxysmal form of AF the probability of restoring the heart rhythm using electrical pulse or drug cardioversion is high, then the permanent form requires significant effort. It should be noted that electrical pulse cardioversion in patients with thyrotoxicosis does not provide a lasting effect and relapse of AF develops in the near future after its implementation. Treatment of patients with a permanent form of AF involves monitoring the heart rate and preventing complications associated with the long-term existence of arrhythmia.
According to existing literature data, and also taking into account our experience, the use of beta blockers against the background of complex drug therapy is rational, and in some cases, extremely necessary:
- in cases of severe thyrotoxicosis and there is a need (allergy or toxic reaction to thyreostatics) to discontinue the thyrostatic drug or reduce its dose to eliminate or reduce the increased sympathetic effect of TG on the heart;
— as part of complex therapy: in preparation for surgical treatment and insufficient effectiveness of drug thyreostatic therapy in terms of restoring sinus rhythm or heart rate control; in the presence of severe cardiovascular disorders (coronary artery disease, previous myocardial infarction, arrhythmia, heart failure, hypertension) to speed up preoperative preparation and minimize hemodynamic disturbances; for successful surgical intervention, prevention of recurrence of arrhythmia during surgery; to prevent thyrotoxic crisis and cardiac complications.
Many years of experience in the use of various classes of antiarrhythmic drugs in the treatment of arrhythmias, and especially AF/AFL, in the clinic of the institute showed the greatest effectiveness when prescribing amiodarone (cordarone), which was used at 600 mg/day. 1-2 weeks, followed by a gradual reduction in its daily dose to 100-200 mg over 3-4 weeks until stable remission of thyrotoxicosis is achieved or before surgical treatment. A faster decrease in heart rate and more frequent restoration of sinus rhythm were noted. After surgery, in the immediate postoperative period, cordarone continued to be prescribed for 1-2 weeks at a dose of 100-200 mg/day, followed by its discontinuation and transfer of patients to beta-blockers. We did not observe any worsening of the functional state of the thyroid gland with this use of amiodarone.
Amiodarone in the treatment of arrhythmias
In the last 25 years, the class III antiarrhythmic drug amiodarone (Cordarone, Sanofi-Aventis, France), which was discovered in 1960 by researchers Tondeur and Binon, has found use in cardiology. It is the only antiarrhythmic drug that does not have a negative inotropic effect, has an inhibitory effect on alpha and beta receptors, dilates coronary and peripheral vessels, reduces the automaticity of the sinoatrial node, slows down conduction and increases the refractoriness of the myocardium of the ventricles, atria, atrioventricular node, in the His system - Purkinje. Slows down the conduction of the impulse along additional pathways. It has been shown that cordarone reduces myocardial oxygen demand, promotes the accumulation of high-energy phosphates in cardiomyocytes and has an antifibrillatory effect. The main mechanism of its action is provided by the blockade of potassium ion channels of the cell membranes of cardiomyocytes. However, unlike other class III antiarrhythmic drugs (sotalol, ibutilide), it can inactivate fast sodium and slow calcium channels, which is typical for class I and IV antiarrhythmic drugs.
When treated with cordarone, heart rate slows down, total peripheral and coronary resistance decreases, and QT dispersion decreases. The drug inhibits the production of cytokines and prevents free radical damage to cardiomyocytes and endothelial cells. Cordarone differs from other antiarrhythmic drugs in its low toxicity and long-lasting effect due to its cumulative properties.
Multicenter studies BASIS, PAT, CAMIAT, EMIAT, meta-analysis of 13 studies ATMA, ALIVE, ARREST, conducted in the 90s and 2000s, as well as studies RASE, AFFIRM, GESICA and EPAMSA showed that the drug improves long-term prognosis and life expectancy of patients with some forms of ventricular and supraventricular arrhythmias. After 35 years of clinical use, cordarone remains the main antiarrhythmic drug included in the latest recommendations of the European Society of Cardiology for the treatment of AF, heart failure, and prevention of sudden death.
Cordarone has the properties of almost all classes of antiarrhythmics and is an iodinated fat-soluble derivative of benzofurin containing 37% iodine, which corresponds to 75 mg of iodine in 200 mg of one tablet. The molecular structure of the drug is similar to iodothyronines, so cordarone can affect the transport of thyroid hormones into cells and their intracellular metabolism. Cordarone is excreted very slowly through the intestines, and iodine is excreted in the urine in the form of iodide salts. The half-life of this drug averages 28 days. The drug penetrates and accumulates in adipose tissue, liver, lungs, thyroid gland and myocardium. During the metabolism of cordarone, approximately 6 mg of inorganic iodine is released daily, while the daily iodine requirement is about 150 mcg and depends on the age of the patient. Its antiarrhythmic effect lasts for 10-100 days after discontinuation.
A very low arrhythmogenic potential has been proven (ventricular tachycardia, sudden death, atrial flutter with 1:1 conduction to the ventricles, bradycardia, AV block, asystole) when used in patients with cardiac pathology. Thus, according to WH Maisel, the risk of arrhythmogenic effects when using cordarone is 4% compared to 11.6, 18.8 and 18.1% when using drugs of classes 1A, 1C and sotalol.
Researchers have found that excessive iodine consumption reduces not only the synthesis, but also the secretion of thyroxine (T4) and triiodothyronine (T3), leading to a slight decrease in their concentration in the blood serum and a compensatory increase in basal and stimulated thyroid-stimulating hormone (TSH), which does not go beyond the limits normal fluctuations. In this case, the euthyroid state is maintained, and the levels of thyroid hormones and TSH in the serum are restored after discontinuation of iodide.
It is believed that the smallest amount of iodide that does not affect thyroid function is 500 mcg per day.
Excessive iodine consumption does not always lead to dysfunction of the thyroid gland, since it has its own regulatory mechanism that ensures its normal functioning with excess iodine. This mechanism, called the Wolf-Chaikov effect, is that when excess iodine enters the patient’s body against the background of normal thyroid function, it is inhibited and the synthesis of hormones transiently decreases for a short time (48 hours), and then, despite continued consumption iodine, is restored (the “escape” effect). Researchers explain this phenomenon by a decrease in the uptake of iodine by the gland, which leads to a decrease in its concentration in the latter and is ensured by a change in the activity of the iodide transporter (Na+ / I– symporter).
These properties of cordarone, on the one hand, classify it as one of the most effective antiarrhythmic drugs with a proven ability to reduce mortality in individuals with cardiac pathology and ventricular arrhythmias and the lowest arrhythmogenicity. On the other hand, doctors are concerned about the possibility of inducing changes in thyroid function (hyper- or hypofunction) when using it due to the high iodine content in its structure. This fact served as an impetus for studying thyroid function in individuals with cardiac pathology and rhythm disturbances who were prescribed cordarone.
Thus, according to a multicenter study (in 5 centers of Ukraine), conducted in 2002, it was found that there was no change in thyroid function after 6 months of use of cordarone in patients with a persistent form of atrial fibrillation and HF, but without impaired thyroid function to restore and preserve sinus rhythm.
According to other researchers, cordarone-induced thyrotoxicosis develops in 0.003-0.9% of patients, hypothyroidism in 6%, subclinical hypothyroidism in 3.05% of patients with long-term use (1-2 years).
It has been established that the clinical effect of excess iodine varies depending on its content in the regions of residence and the initial function of the thyroid gland. If hypothyroidism develops mainly in patients living in iodine-supplied areas, then thyrotoxicosis develops in those who live in areas with iodine deficiency.
Various hypotheses regarding the mechanisms of occurrence of these complications of cordarone therapy are currently being discussed.
The occurrence of hypothyroidism is associated with a long-term block in the organization of iodine in the thyroid gland due to a violation of the “escape” effect from the suppressive Wolf-Chaikov effect.
Hypothyroidism may be a consequence of cordarone inhibition of TSH-dependent cAMP production in intact thyrocytes, which reduces the synthesis of thyroid hormones and iodine metabolism, possibly through an effect on lipid-protein relationships in TSH receptors and, as a result, disruption of signal transmission.
In addition, cordarone inhibits the activity of 5-deiodinase, a selenoprotein that mediates the conversion of T4 thyroxine to T3 and reverse T3 (rT3), and then to diiodothyronine. If this metabolic process is disrupted, the T3 content decreases.
With the development of thyrotoxicosis induced by amiodarone (AT), 2 variants are considered with different mechanisms of occurrence depending on the initial state of the thyroid gland.
The first variant of AT develops in individuals with initial thyroid pathology due to increased synthesis of TG in existing zones of automaticity under the influence of iodine released from cordarone.
The second variant of AT can be observed in patients without initial thyroid pathology and develops as a result of the direct cytotoxic effect of cordarone and iodine on thyroid cells, leading to their destruction and release of stored hormones.
After discontinuation of cordarone, the process of restoration of thyroid function proceeds very slowly due to its long half-life. When discussing patient management tactics, if such patients need to continue taking cordarone, it is indicated that appropriate doses of L-thyroxine are prescribed to normalize TSH levels. In the first variant of induced hyperthyroidism, the abolition of cordarone and the prescription of large doses of antithyroid drugs are required to block further iodine entry into the thyroid gland; in the second variant, corticosteroids are required.
To summarize, it should be noted that there are conflicting opinions regarding the possibility of cordarone-induced thyroid dysfunction. The established contradiction can be explained by the analysis of data with different periods of use of cordarone, as well as the heterogeneity of the study groups and dosages of the drug.
Based on the presented studies, the following conclusions can be drawn.
1. Induced dysfunction of the thyroid gland was observed mainly with long-term use of cordarone (more than 6 months) in a small number of patients. The incidence of this complication can be significantly reduced if the minimum effective maintenance dose (100-200 mg/day) is prescribed if long-term use is necessary.
2. In order to reduce the incidence of cordarone-induced hyper- or hypothyroidism in cardiac patients, before the intended long-term use of the drug, it is necessary to first determine the levels of T3, T4 and TSH in plasma, then also periodically monitor (once every 6 months) these indicators throughout treatment for early detection of subclinical forms of the disease, to reduce its dose or timely discontinuation of the drug. In addition, it is important to clarify the family history for the presence of thyroid diseases in relatives in order to exclude a possible genetic predisposition.
3. As the disease is compensated in the presence of risk factors for the development of induced hypo- or hyperthyroidism, it is possible in the future to replace cordarone with cardioselective beta-blockers with their further prolonged use (if necessary).
The use of cordarone is possible in elderly patients with thyroid diseases and concomitant cardiac pathology (atherosclerosis, ischemic heart disease, hypertension), aggravated by HF, taking into account its antianginal and antiarrhythmic properties, for faster relief compared to other antiarrhythmic drugs of extrasystolic arrhythmia, fibrillation and atrial flutter , as well as in cases of resistance to the latter. It is also important to be able to control the heart rate in patients with a permanent form of AF in order to prevent complications associated with the long-term existence of arrhythmia (thromboembolism, sudden death); in this case, the therapy of choice is the prescription of highly cardioselective blockers with a high degree of bioavailability and a long-lasting effect throughout the day.
Tachycardia - what tests should I take?
Among the laboratory tests necessary for correct diagnosis and the most effective treatment of tachycardia, the following are worth mentioning first:
- general blood analysis;
- lipid profile, which examines total cholesterol and triglycerides, as well as levels of “good” and “bad” cholesterol - high-density lipoproteins (HDL), low-density lipoproteins (LDL) and very low-density lipoproteins (VLDL);
- electrolyte analysis;
- tests for thyroid hormones - thyroid-stimulating hormone (TSH) and free T4, as well as a test for antibodies to thyroid peroxidase (ATPO).
In addition, to diagnose tachycardia, the cardiologist prescribes some other non-laboratory examinations: electrocardiography (including daily Holter ECG monitoring), echocardiography, etc.
If you “catch” the disease in the early stages and determine the cause of its development as accurately as possible, tachycardia can be cured completely . Therefore, under no circumstances should you be indifferent to any alarming symptoms associated with your heart rhythm, because otherwise the disease will progress, the danger will increase, and treatment will ultimately be much longer and more expensive.
Full treatment of tachycardia is not only taking medications, but also revising your own lifestyle and diet. Try to maintain normal physical activity (but without overwork), sleep at least 7–8 hours a day, reduce the consumption of animal fats, refined sugar, caffeine, and alcohol. The ideal basis of nutrition for tachycardia and other heart problems is dairy-vegetable. As prescribed by your doctor, you can take multivitamin and mineral supplements with potassium and magnesium, or take these elements separately.
Tachycardia - symptoms
The main symptoms of tachycardia are:
- increased heart rate (90 or more beats per minute);
- increased heart rate (ventricular tachycardia);
IMPORTANT! The heart rate (HR) and pulse should normally match the number of beats per minute. Heart rate is the number of heart contractions per minute, and pulse is the number of dilations of the artery during the same time, at the moments of “ejection” of blood by the heart. With tachycardia and other heart diseases, heart rate and pulse indicators may differ.
- lowering blood pressure;
- a feeling of heaviness in the chest, even suffocation;
- shortness of breath, sometimes even with minor physical exertion or at rest;
- skin moisture;
- interruptions and “failures” in the work of the heart;
- dizziness, darkness in the eyes, presyncope (sometimes fainting associated with cerebrovascular accident);
- pain in the heart area - this symptom is characteristic of tachycardia against the background of vegetative-vascular dystonia (VSD) and some other pathological conditions.
If you find yourself with one or more of the listed symptoms and suspect that you have tachycardia, what should you do first? Of course, contact a cardiologist who will refer you to certain examinations and tests, and then prescribe treatment. You can take the necessary tests in advance so that you can come to the doctor with ready-made results.
Clinical picture
Manifestations of the disease are very variable - from extremely pronounced forms to erased variants. The latter are especially common when the disease begins in old age.
- The thyroid gland, as a rule, is enlarged due to both lobes and the isthmus, and is painless. In older people and men, thyroid disease often occurs with normal or only slightly increased thyroid volume. The absence of thyroid enlargement in itself does not exclude the diagnosis of thyroid disease.
- Cardiovascular system : constant, less often sudden palpitations; interruptions in heart function; increased blood pressure, and in severe thyrotoxicosis – heart failure (“thyrotoxic heart”).
- Metabolism: weight loss, increased body temperature, hot skin, sweating, muscle weakness.
- Nervous system : increased excitability, tearfulness, fussiness, tremor of outstretched arms and the whole body.
- Digestive system: abdominal pain, unstable stool with a tendency to diarrhea, loss of appetite (in young people - increased, in older people - absent).
- Endocrine glands : menstrual irregularities up to amenorrhea, in men gynecomastia and decreased libido, impaired carbohydrate tolerance.
- Eye symptoms: glossy eyes, widening of the palpebral fissures, lag of the upper eyelid from the iris when looking up, lag of the upper eyelid from the iris when looking down, loss of the ability to fix the gaze at close range, lack of wrinkling of the forehead when looking up, rare blinking - develop as a result of the disorder autonomic innervation of the eye.
The ocular symptoms of thyrotoxicosis are fundamentally distinguished from the independent disease of endocrine ophthalmopathy.
Endocrine ophthalmopathy (EOP) is a lesion of periorbital tissues of autoimmune origin, in 95% of cases combined with autoimmune diseases of the thyroid gland (thyroid gland), clinically manifested by dystrophic changes in the extraocular muscles (EOM) and other structures of the eye.
EOP is an independent autoimmune disease, however, in 90% of cases it is combined with diffuse toxic goiter (DTZ), in 5% with autoimmune thyroiditis, in 5-10% of cases there is no clinically detectable thyroid pathology. In some cases, DTZ manifests itself later than the image intensifier. Men suffer 5 times more often. In 10% of cases, the image intensifier is unilateral.
Antibodies to TSH receptors (ATrTSH) have several functionally and immunologically distinct subpopulations. ATrTSH can cause immune inflammation and swelling of the retrobulbar tissue, which leads to a decrease in the volume of the orbital cavity with the development of exophthalmos (bulging eyes) and dystrophy of the extraocular muscles.
The image intensifier begins gradually, often on one side. Initial symptoms: a feeling of pressure behind the eyeballs, increased sensitivity to light, a feeling of a foreign body, “sand in the eyes.” Further, the symptoms increase.