Detailed description of the study
An extended blood test is a primary study that is used to assess the general condition of the body, identify a wide range of diseases and monitor their treatment.
The main indicators that are included in the extended clinical blood test:
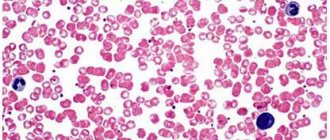
Erythrocytes are cells also called red blood cells. The main function of red blood cells is to transport oxygen to tissues and remove carbon dioxide (CO2) from them.
Hemoglobin is the main protein in red blood cells. It directly allows for gas exchange in tissues by combining with oxygen, or CO2. Insufficiency of hemoglobin in the body, along with a decrease in red blood cells, serves as the basis for the development of anemia.
Hematocrit is the ratio of all formed elements of blood (mainly red blood cells) to the liquid component of blood. Allows you to judge the excess or deficiency of red blood cells, dehydration or overhydration of the body.
The color indicator reflects how adequately the saturation of erythrocytes with hemoglobin is, helps the specialist to establish anemia and differentiate it into normochromic, hypochromic or hyperchromic.
MCH (Mean Cell Hemoglobin) - an indicator reflecting the average hemoglobin content in red blood cells, is a modern and more accurate analogue of the color indicator.
MCV (Mean Cell volume) determines the average volume of a red blood cell. Used in conjunction with MCH to identify anemia and its causes.
RDW (Red cell Distribution Width) reflects the heterogeneity of red blood cells by volume. The indicator is also important in the diagnosis of anemia; it depends on the mean erythrocyte volume (MCV), therefore, when MCV increases or decreases, its increase is observed, which indicates that there are cells of different volumes in the blood.
MCHC (Mean Cell Hemoglobin Concentration) helps estimate the mean hemoglobin concentration in red blood cells. Changes in the indicator are observed in cases of impaired hemoglobin synthesis, hypochromic and hyperchromic anemia.
Platelets also belong to the formed elements of blood; they play a key role in the processes of hemostasis and ensure timely blood clotting in case of vascular damage. Changes in this indicator may be associated with impaired cell production in the bone marrow or their accelerated destruction.
Leukocytes are called white blood cells. They participate in various immune processes and protect the body from infection. There are several types of leukocytes: eosinophils, neutrophils, lymphocytes, basophils, monocytes. Their percentage ratio allows you to evaluate the leukocyte formula to understand the current state of the immune system, identify and determine the severity of inflammatory and allergic processes in the body.
Neutrophils , the largest population of white blood cells, are aimed at fighting foreign microorganisms - including bacterial infections - in the body.
Lymphocytes play an important role in recognizing pathogenic microorganisms and forming and regulating immunity to various infections by releasing antibodies and destroying infected cells.
Monocytes are white blood cells that can differentiate into macrophages and dendritic cells after they migrate to peripheral tissues. Viral and bacterial particles are absorbed, then target proteins appear on the surface of the cell to recognize the infectious agent by the immune system. This helps in fighting pathogens and building adaptive immunity. Monocytes also take part in cleansing the body of dead cells and tissue healing.
Basophils and eosinophils are actively involved in the development of allergic reactions. They contain many granules with bioactive molecules that cause allergy symptoms. Eosinophils also play a role in protecting the body from parasites.
Reticulocytes serve as precursors of red blood cells. Their number reflects erythropoiesis - the rate of formation of red blood cells in the bone marrow. This indicator is important when assessing the effectiveness of anemia therapy. Additionally, the percentage of reticulocytes, the content of their immature forms and the production index of these cells are determined. Taken together, these data are used to manage patients with hematopoietic disorders.
Taken together, the indicators of an extended clinical blood test are necessary for the doctor as a stage of primary laboratory diagnosis of a wide range of diseases. The test can also be used to assess general health.
Classification
Erythrocytosis is diagnosed when the following indicators are exceeded: in men – 5.5x109/ml, in women and children under 13 years of age – 4.7x109/ml.
In newborns, the number of red blood cells should exceed 5.6x109/ml. The following types of erythrocytosis are distinguished: 1. Based on the presence or absence of a connection with pathological processes:
- Physiological
. The change in the indicator is not associated with diseases. Occurs as part of adaptation to hypoxia caused by environmental conditions. - Pathological
. Accompanies some diseases and develops as a result of disturbances in homeostasis caused by various traumatic and non-traumatic causes.
2. According to the changes underlying erythrocytosis:
- Absolute
. It becomes a consequence of increased erythropoiesis against the background of hypoxia, increased production of erythropoietin due to kidney disease, endocrine diseases, and hormonally active tumors. - Relative
. Formed after a decrease in plasma volume as a result of profuse sweating, vomiting, and diarrhea.
3. By time of occurrence:
- Primary
. It is hereditary in nature, provoked by gene mutations that cause changes in the structure of hemoglobin or the enzyme that is responsible for transporting oxygen into red blood cells and its subsequent “return” to tissues. - Secondary (symptomatic)
. It develops throughout life and is potentiated by diseases and pathological conditions.
Symptomatic erythrocytosis is the most common type of this condition. Identified in men and women, it can be absolute or relative. Absolute symptomatic erythrocytosis is found more often than relative erythrocytosis and is provoked by the following factors:
- Kidney diseases
: ischemia of various etiologies, neoplasms, condition after kidney transplantation. - Neurohumoral regulation disorders
: excessive stimulation of the autonomic nervous system. - Endocrine disorders
: increased levels of thyroid hormones, glucocorticoids, catecholamines, adrenocorticotropic hormone. - Blood diseases
: hemoblastosis with increased production of red blood cells. - Hemic hypoxia
: poisoning with substances that reduce the oxygen capacity of the blood. - Circulatory hypoxia
: insufficient blood supply to organs and tissues due to impaired cardiac function. - Respiratory hypoxia
: a decrease in the volume of ventilation of the lungs against the background of bronchopulmonary pathologies. - Exogenous hypoxia
: normobaric hypoxia with a lack of oxygen in the air, hypobaric hypoxia with decompression sickness.
Among the relative symptomatic erythrocytoses, hemoconcentration ones predominate - arising as a result of a decrease in the amount of fluid in the vascular bed. Less common in women and men are redistributive erythrocytosis - conditions in which there is a sharp release of red blood cells from the depot.
Erythrocytosis
References
- Nazarenko, G.I., Kishkun, A.A. Clinical evaluation of laboratory results. - M.: Medicine, 2006. - 544 p.
- Tatkov, O.V., Stupin, F.P. General blood analysis. Information collection. - M.: Publishing solutions, 2021. - 72 p.
- Fauci, A., Braunwald, E., Kasper, D. et al. Harrison's principles of internal medicine, 17th edition, 2009.
- Pagana, K., Pagana, T., Pagana, Th. Mosby's Diagnostic and Laboratory Test Reference. 14th Edition. Elsevier Publishing Hall, 2019. - 1094 p.
Why does erythrocytosis occur?
Physiological reasons
A high number of red blood cells is detected in residents of high mountain areas. Even in the absence of somatic diseases, the body suffers from hypoxia; due to a decrease in the amount of oxygen in the external environment, more blood cells are produced compensatoryly to transport it. In native-born residents of the highlands, physiological erythrocytosis is observed throughout their lives; in visitors, it develops during a long stay in the area.
Another example is erythrocytosis in infants after birth. In the womb, the fetal blood was saturated with oxygen from the mother's blood. There is less oxygen in a woman's blood than in the air, so the unborn child needed a lot of red blood cells to carry it. With the beginning of breathing atmospheric air, the supply of oxygen increases, the number of blood cells gradually decreases.
Respiratory hypoxia
Erythrocytosis is detected in pathologies accompanied by a decrease in the volume of pulmonary ventilation:
- Bronchial asthma.
Can be allergic, non-allergic (for example, aspirin), mixed. An attack of suffocation is accompanied by a feeling of tightness in the chest, a reduction in the duration of inspiration, an increase in the duration of exhalation, wheezing, forced positioning, and swelling of the neck veins. - Chronical bronchitis.
It can be obstructive or non-obstructive. Manifests itself as a cough with mucopurulent sputum. The amount of sputum increases during an exacerbation. Symptoms of obstruction are expiratory shortness of breath, persistent cough, wheezing, and swelling of the jugular veins. - COPD
Characterized by a progressive course of bronchitis or emphysematous type. In the first case, the symptoms of obstructive bronchitis predominate, in the second - expiratory shortness of breath. - Restrictive violations
. Chronic pneumonia, pneumosclerosis, pneumothorax, exudative pleurisy, widespread adhesions in the pleural cavity, and other conditions lead to restriction of the movements of the lung tissue.
Along with nonspecific diseases, various forms of pulmonary tuberculosis and pneumoconiosis play a significant role in the development of respiratory hypoxia with symptomatic erythrocytosis: silicosis, silicosis. In addition, this type of hypoxia is observed in smokers. Caused by the constant intake of tobacco smoke, the occurrence of smoker's bronchitis (a type of COPD). Men are more often affected.
Circulatory hypoxia
The phenomena of hypoxia are most clearly expressed in blue heart defects, accompanied by venous discharge or mixing of blood with hypovolemia of the pulmonary circulation, hypoxemia. Secondary erythrocytosis and the development of collaterals to a certain extent make it possible to compensate for hemodynamic disturbances. Due to the threat of irreversible dystrophic changes in the myocardium, children are recommended to undergo surgery at an early age. Erythrocytosis is characterized by the following defects:
- Fallot's disease: triad, tetrad, pentad;
- tricuspid valve atresia;
- transposition of the great vessels;
- anomalies of the confluence of the pulmonary veins;
- common arterial trunk.
Hemic hypoxia
A decrease in the oxygen capacity of the blood and compensatory erythrocytosis are potentiated by some exogenous intoxications. Carbon monoxide poisoning occurs at home or at work. Accompanied by a pressing headache, nausea, dizziness, unsteadiness of gait. Sometimes convulsions and coma are observed. Subsequently, retrograde amnesia, cardiac conduction disturbances, pneumonia, and bronchitis are possible.
Nitrate poisoning is caused by drinking water, agricultural products grown with nitrogen fertilizers, taking large doses of certain pharmaceuticals, and inhaling toxic fumes. Manifested by gastrointestinal disorders, jaundice, shortness of breath, hypotension, and disturbances of consciousness.
Exogenous hypoxia
At normal atmospheric pressure, but limited air flow, normobaric hypoxia occurs. Erythrocytosis is observed in victims of natural disasters, industrial accidents (for example, staying in a confined space without access to air after a mine collapse). The cause of hypobaric hypoxia is a decrease in barometric pressure when pilots spend a long time at high altitude. There is an extremely rapid change in environmental conditions with the development of decompression sickness.
Kidney diseases
Insufficient blood supply to the kidneys and the presence of space-occupying formations in the organ stimulate increased release of erythropoietin and activation of the red germ of hematopoiesis. Erythrocytosis is accompanied by:
- Pyelonephritis.
Acute inflammation is characterized by increased body temperature, weakness, dull pain in the lumbar region, and change in the color of urine. In a chronic process, the symptoms are smoothed out, the general condition is not disturbed. - Glomerulonephritis.
The acute form occurs with hyperthermia, signs of intoxication, hematuria, hypertension, edema, more pronounced on the face. Chronic glomerulonephritis typically has a relapsing course with the periodic appearance of acute inflammation. - Hydronephrosis.
Occurs due to obstruction of urine flow. It manifests itself as discomfort, dull pain in the lower back, which is later joined by progressive fatigue, transient hypertension, and hematuria. - Renal artery stenosis.
Increasing arterial hypertension and ischemic nephropathy are noted. The first syndrome includes cerebral manifestations, the second – low back pain, sometimes hematuria. The development of secondary hyperaldosteronism is possible. - Kidney cyst.
Erythrocytosis develops with compression of blood vessels and stimulation of the juxtaglomerular apparatus, accompanied by an increase in blood pressure. Other possible symptoms are pain and urodynamic disturbances.
The list of neoplasms that provoke erythrocytosis includes nephroblastomas, hypernephromas, and neoplasias that secrete erythropoietin. Sometimes the rate increases in patients who have undergone a kidney transplant.
Neurohumoral regulation disorders
Increased activity of the sympathetic nervous system, causing erythrocytosis, accompanies chronic heart failure and neurogenic essential arterial hypertension. A similar change in the level of red blood cells against the background of neurohumoral disorders is observed with severe sleep apnea or frequent panic attacks.
Endocrine pathologies
Some hormones increase the level of oxygen utilization, so their overproduction is accompanied by secondary erythrocytosis:
- Thyroid hormones
. Hyperthyroidism is observed in diffuse toxic goiter, autoimmune thyroiditis, and toxic thyroid adenoma. - Adrenocorticotropic hormone
. Hypercorticism is determined by pituitary microadenoma, Itsenko-Cushing syndrome caused by adenomas and adenocarcinomas of the adrenal glands, ACTH-ectopic syndrome. - Catecholamines and glucocorticoids
. Increased levels of hormones are found, respectively, in tumors of the medulla and cortex of the adrenal glands.
In addition, erythrocytosis is diagnosed in people taking androgenic steroids as doping to stimulate muscle growth and improve athletic performance.
Polycythemia
Erythremia (polycythemia or Vaquez's disease) is a chronic leukemia accompanied by increased proliferation of all hematopoiesis, primarily erythrocyte. Typical signs of the disease are plethora (telangiectasia, red or cherry skin tone, scleral hyperemia), unbearable skin itching. Many patients have erythromelalgia. As it progresses, bone pain, migraines, hypertension, and myalgia are observed.
Hereditary familial erythrocytosis
It is a group of genetically determined diseases with changes in the structure of hemoglobin, metabolic disorders in red blood cells, and excessive release of erythropoietin by the kidneys. The severity and time of onset of symptoms are determined by the form of hereditary familial erythrocytosis. Possible tachycardia, varicose veins, hemorrhoids, hepatosplenomegaly, shortness of breath, increased bleeding.
Fluid loss
Hemoconcentration with the formation of erythrocytosis occurs with significant fluid losses. In a healthy person, a transient disturbance in a laboratory indicator can be determined during prolonged thirst, after profuse sweating when working in conditions of high ambient temperature. The latter option is more common among men engaged in heavy physical labor. Erythrocytosis is also found in the following conditions:
- Intestinal infections:
cholera, dysentery, salmonellosis. Fluid is lost through repeated vomiting and profuse diarrhea with watery stools. - Extensive burns:
more than 15% of the body surface for burns of II and more severe degrees. The cause of hemoconcentration is the release of burn exudate. - Ketoacidosis:
ketoacidotic coma in patients with diabetes mellitus. The fluid is excreted from the body through the kidneys along with glucose.
Red blood cell count
Diagnostics
Diagnosis of lung diseases is carried out by pulmonologists. Patients with suspected kidney pathology are examined by nephrologists. Other diseases require the participation of hematologists, oncologists, and other specialists. Erythrocytosis is confirmed by a general blood test. Other indicators determined during the study are hemoglobin and hematocrit levels, the number of reticulocytes, leukocytes, and platelets.
Leukocytosis with a shift of the formula to the left indicates the presence of an inflammatory process. Reticulocytosis is detected in broncho-obstructive diseases, restrictive lesions of lung tissue, cyanotic heart defects, and polycythemia. Vaquez disease is also characterized by increased levels of platelets and leukocytes, and microcytosis is possible.
To clarify the diagnosis, the patient is prescribed an extensive laboratory examination. The level of erythropoietin is determined and the blood gas composition is examined. If endocrine diseases are suspected, hormonally active tumors are analyzed for adrenal hormones, thyroid hormones, and ACTH. Patients with polycythemia undergo trephine biopsy followed by histological examination. The list of instrumental techniques depends on the nature of the pathology:
- Lung diseases
. The basic study is chest x-ray. The images reveal signs of bronchitis, pneumonia, pneumosclerosis, tuberculosis, and other diseases. The method can be supplemented by MRI, bronchoscopy, spirometry, pneumotachography. - Heart defects
. The list of diagnostic procedures includes electrocardiography, phonocardiography, Holter monitoring, echocardiography, and chest radiography. Patients with pulmonary hypertension are advised to undergo angiography and cardiac probing. - Kidney diseases
. Patients are prescribed ultrasound, MRI, CT scan of the kidneys. Pyelography, excretory urography, nephroscintigraphy are performed. To identify secondary disorders from other organs, fundus examination, ECG, and ultrasound of the pleural cavity are performed. To clarify the nature of the pathological process, a biopsy with morphological examination is performed. - Endocrine disorders
. Depending on the existing symptoms, ultrasound or MRI of the adrenal glands or thyroid gland, radiography of the sella turcica, and contrast MRI of the brain may be recommended.