Blood donation (from the Latin donare - “to give”) and (or) its components is the voluntary donation of blood and (or) its components by donors, as well as activities aimed at organizing and ensuring the safety of the collection of blood and its components. Blood taken from a donor (donor blood) is used for research and educational purposes; in the production of blood components, medicines and medical devices. The clinical use of donor blood and (or) its components is associated with transfusion (transfusion) to the recipient for therapeutic purposes and the creation of reserves of donor blood and (or) its components.
Artificial blood substitutes have side effects, are toxic, expensive and are not able to completely replace all components and reproduce all the functions of blood in the body, therefore donor blood is practically irreplaceable for transfusions to victims of burns and injuries, during complex operations and during difficult childbirths. Blood is also vital for patients with hemophilia, anemia and cancer patients during chemotherapy. Every third inhabitant of the Earth needs donor blood at least once in his life.
Detailed description of the study
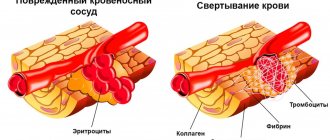
Platelets are nuclear-free blood cells, blood platelets. They are formed in the red bone marrow and remain viable for 7-10 days. Platelets have properties such as adhesion (the ability to stick to the vascular wall) and aggregation (the ability to stick together). These properties ensure the implementation of the main functions of platelets: hemostatic and angiotrophic. Platelets also contain some active substances and coagulation factors, which, when activated, are released into the blood.
The hemostatic function of platelets is the secretion of vasoconstrictor substances, the formation of a platelet plug when the integrity of blood vessels is disrupted, and the acceleration of the formation of a fibrin clot.
The angiotrophic function is that platelets supply growth factors for the cells of the vascular wall, necessary for its restoration. Therefore, thrombocytopenia is often accompanied by the appearance of pinpoint hemorrhages in the skin or mucous membranes. In addition, platelets perform a protective function by “gluing” (agglutination) bacteria. Marked changes in the number of platelets in the blood can lead to various pathological processes: blood clotting disorders (thrombosis or bleeding), vascular fragility (the appearance of bruises and petechiae), and a decrease in the body’s protective properties. Sometimes counting platelets in a complete blood count can be difficult. This is observed with a pronounced tendency of platelets to aggregation, with certain diseases, as well as with exposure to toxic substances.
In such cases, platelet count according to Fonio is recommended. The advantage of this method is that the platelet count is calculated per thousand red blood cells in stained blood smears. Then the resulting amount is recalculated in proportion to a certain volume using a special formula.
City blood transfusion station of St. Petersburg
June 23, 2021
Dear donor! This section provides a navigator to the main questions donors ask. To get as much information as possible, we kindly ask you to visit all sections of this page. It's comfortable! Read the text, click on the words with blue font text and a new page will open in your browser with important information for your review. Quick section navigation will help you find important information. If you do not find the answer to your question, then write to us on WhatsApp or VKontakte.
- Who can become a blood donor;
- What documents must the donor present;
- How to prepare for donation;
- What diseases should you not donate blood for?
- Where and when can you donate blood;
- Possible restrictions on accepting donors;
- What is the donation procedure like?
- Social support for donors;
- Rest periods between donations;
- Who are Kell+ donors?
- Platelet cell donation;
- Donation code;
- Why is it important to donate blood regularly?
1) Who can become a blood donor.
A person who is 18 years old on the day of donation can become a donor. There is no upper age limit if a transfusiologist at a blood service institution decides on admission to donation based on the results of a medical examination. The donor must present at the institution a passport of a citizen of the Russian Federation, as well as SNILS. Foreign citizens can donate blood if they have resided legally in the Russian Federation for at least a year (supporting documents must be provided). The standard blood collection volume is 450 ml + 10% for analysis (up to 40 ml), which is recommended for donors weighing over 55 kg. The decision on admission to donation and the type of donation is made by a transfusiologist at a blood service institution based on the results of a medical examination. Medical examination of donors contains a procedure common to all types of donation and categories of donors and additional individual requirements for each type of donation and categories of donors. Work with donors and medical examination of donors are carried out in full compliance with the Federal Law “On the Donation of Blood and Its Components” {↑}
2) What documents must the donor present?
To perform the donor function, the donor is required to present a passport of a citizen of the Russian Federation or another identification document. With an identification document, the donor must present SNILS once. Please note that photocopies, electronic versions of documents and other types of documents other than originals are not accepted. Identity documents of a universal nature are here. For foreign citizens, we note that, together with an identity document of a foreign citizen, a person must present documents confirming residence in the territory of the Russian Federation legally for at least one year. {↑}
3) How to prepare for donation.
Taking medications: antibiotics - donation is possible no less than 14 calendar days after the end of the dose. Analgesics, anticoagulants, antiplatelet agents (including salicylates) - donation is possible no less than 3 calendar days after the end of administration. 48 hours before donation, it is not recommended to consume alcoholic beverages, fatty, fried, spicy and smoked foods, as well as dairy products, eggs and butter, chocolate and dates. In the morning, it is recommended to have breakfast in compliance with the “donor diet”. Before blood donation you need to rest. It is not advisable to donate blood after a night shift, heavy physical work, nervous strain, or prolonged food restriction.
Possible options for the first breakfast: Oatmeal porridge with water, boiled beef tongue, tea with sugar, toasted bread and porridge with water, chopped fresh vegetables, cereal with water with the addition of dried fruits.
Possible options for second breakfast: Fresh fruits (except those in the NO category), freshly squeezed juice, dried fruit compote, jelly, soaked dried apricots, mineral water, fruit juice, drying.
Possible lunch options: Vegetarian vegetable soup, boiled chicken breast, noodle soup, rice, buckwheat, pearl barley soup, boiled noodles, meat balls or boiled fish without marinade, warm salad to taste without dressing.
Possible dinner options: Carrot zrazy, mashed potatoes (in water), low-fat fish (baked in the oven without marinade, boiled potatoes, steamed meat cutlets, vegetable salad without dressing, potato casserole with meat, grated carrot salad with apple without dressings, steamed fish balls, boiled potatoes with herbs, sweet bell peppers, carrot and apple balls, boiled low-fat fish without dressing and sauces, vegetable stew, stewed cabbage, steamed vegetables, water pasta.
Not allowed: Smoked, spicy and fried foods, pickles, dairy products (including yoghurt, cheese, cream, butter), eggs, nuts, dates, bananas, beets, blueberries, sausages, halva, seeds, snacks (chips, croutons) etc.), ketchup, mayonnaise, sauces and marinades, fatty meats or fish.
Such dietary restrictions are due to the fact that many products contain harmful synthetic substances that help the products retain their taste, color and freshness for a long time. Also, consuming even a small amount of fats and animal proteins affects the composition and quality of the blood, and interferes with its separation into components. In addition, due to microparticles of fat, the blood serum becomes too thick, viscous, and takes on a cloudy appearance called plasma chylosis. We will determine dietary violations before and/or during donation. Violations in the diet lead to changes in the quality of blood and its components. A donor who violates the diet is suspended from donations for a certain period of time {↑}
4) What diseases should you not donate blood for?
There are certain medical temporary and absolute contraindications to donating blood and its components, a full list of which is available here. You may be disappointed that you will not be able to donate if you have persistent contraindications. However, the Blood Service hopes that you will understand our main goal - ensuring the safety of donated blood components for patients. The presence of contraindications to donation does not mean that you cannot contribute to the development of voluntary blood donation! In the volunteer section you can find out how to help the donor movement. Save lives with the Blood Service! {↑}
5) Where and when can you donate blood.
The city blood transfusion station accepts donors on weekdays from 09:00 to 13:00 and the first Saturday of the month from 09:00 to 13:00. Sunday: no donors are accepted. Additional weekends and holidays are established according to the production calendar. Restrictions on admission are possible based on the needs of the institution and requests from medical organizations in St. Petersburg. Current admission information is published here. We recommend visiting our website or VKontakte group on the eve of visiting the station to familiarize yourself with possible restrictions and the data of the current Donor traffic light. You can ask your question to the institution’s specialists via the WhatsApp messenger. The city blood transfusion station is located five minutes from the Moskovskie Vorota metro station (map). There may be restrictions on accepting primary donors, i.e. those who have not previously passed in our institution. In the section “Where to donate blood in St. Petersburg” you will find contact information for all blood service institutions in the city. We recommend contacting your chosen institution before visiting. {↑}
6) Possible restrictions on accepting donors.
It is impossible to predict the need of hospitals for donor blood of a particular blood group and Rh factor. It is unknown how many patients and with what blood group will require donor blood transfusion. Situations arise when there is not enough blood of a certain group and rhesus, and there is an excess of another. To create an optimal supply of donor blood, a “Donor traffic light” was created. A special section provides information about accepting donors and which blood groups are in demand and which are in full supply. Why is personnel donation so important and why are there restrictions on admission? Whole blood taken from a donor is divided into components: red blood cells, platelets and plasma. But red blood cells and platelets cannot be stored for long and must be transfused soon after donation. But blood plasma (in the presence of infections, it is this that contains the bulk of viruses!) can be preserved, and this property is used for additional prevention of infections. 4 months after donating, the whole blood donor must return to the institution where he donated and donate whole blood, one of the blood components, or simply a test for HIV and viral hepatitis pathogens. And only if all repeated tests of the donor 4 months after blood donation again show the absence of infections, his plasma will be transfused to patients in need. This storage of plasma until the donor is retested is called quarantine. It is precisely because of quarantine that it is very important that the donor comes back to the blood service institution a certain time after giving blood. This is especially important to know for donors who come to donate blood for the first time after major disasters, accidents, or terrorist attacks. As a rule, on such days a lot of people come to the blood transfusion station, but after six months the enthusiasm has already evaporated and donors forget about the need to come again. Please remember her! If a donor makes donations on a regular basis (at least twice a year), then each of his donations is an analysis of the previous donation, which was made 4 months ago. {↑}
7) How does the donation procedure work?
Point No. 1 - registration. At the registry, the donor provides a passport of a citizen of the Russian Federation and SNILS, and after checking in the information databases, our specialist draws up a card and gives the donor a questionnaire in which he must indicate information about his state of health and lifestyle. Try to answer all questions as truthfully as possible to ensure the safety of you and our patients. A donor who deliberately concealed or distorted information known to him about the state of health when performing a donor function bears liability established by the legislation of the Russian Federation if such actions resulted or could result in harm to the life or health of recipients.
- You can save your time at the institution - fill out the donor form and 3 informed consents and come with the completed documents. The file can be downloaded here. It must be completed legibly with your own hand (in block letters in black or blue ink). Consents filled out in the wrong form will not be accepted.
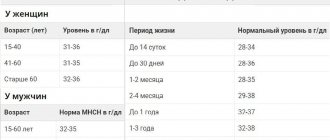
Point No. 2 - laboratory for rapid blood finger test. The donor takes a finger prick blood test in the laboratory, this is necessary to determine the donor's hemoglobin level, as well as other blood factors. The results of this analysis determine whether a person can become a donor on that day.
Point No. 3 - transfusiologist. The doctor examines the donor, studies the questionnaire, and asks additional questions about health, lifestyle and habits. The doctor examines the results of a finger prick blood test and makes a decision on whether to allow donation. The doctor complies with the rules of medical ethics: the information received from the donor is subject to medical confidentiality. An examination by a doctor and a conversation between a doctor and a donor are mandatory procedures before donating blood or its components. Do not hide your ailments from the doctor, answer his questions and the questionnaire honestly, and then donation will be safe both for you and for those who need a transfusion of blood or its components. We remind you that the final decision on the donor’s admission to the procedure, as well as determining its type and volume, is made only by the transfusiologist of our institution. If, during the examination of the donor and the collection of his medical history, assessment of general health, as well as the associated lifestyle, there is a suspicion of drug addiction or behavior leading to the risk of contracting infectious diseases transmitted by blood, the donor should be diverted from donating blood and its components . When determining admission to donation, type of donation and volume of blood or its components taken, the doctor is guided by the List of contraindications to donation of blood and its components, Standards for the composition and biochemical parameters of peripheral blood, Intervals between types of donation (in days). In case of medical withdrawal, the transfusiologist explains to the donor the reason and duration of the withdrawal. If there are temporary contraindications, any visible health problems are detected, or contact with an infectious disease is suspected, the donor is sent for examination to an outpatient clinic at the place of residence.
Point No. 4 - rest and tea before donation. Before donating blood, the donor is asked to eat before the procedure. To balance fluid in the body, it is recommended to drink more, for example, water or weak tea with cookies or a bun. We offer our donors delicious sweet tea and fragrant cookies =)
Point No. 5 - donation. The donation procedure is carried out in the most comfortable conditions for the donor. Blood is collected in specialized sterile and closed systems.
Point No. 6 - compensation for food and rest days. After donation, each donor is issued a certificate, which gives the right to certain benefits and privileges (Read in the “Documents for Donors” section). The donor also receives lunch or compensation for food in order to regain strength after donating blood or its components. Read more about power compensation below.
 Social support for donors.
Social support for donors.
Rest days. After donating blood, the donor receives a certificate that gives him the right to 2 days off during the calendar year from the date of donation (Article 186 of the Labor Code of the Russian Federation). Full text of explanations for the employee and employer with all references to legislative acts.
Nutrition compensation. In accordance with regulatory legal acts, a gratuitous blood donor is paid monetary compensation for food in the amount of 5% of the subsistence minimum established for residents of the city of St. Petersburg (as of June 2021 - 654 rubles). City institutions, in accordance with regulations, pay a gratuitous blood donor monetary compensation for food in the amount of 5% of the cost of living established for residents of the city of St. Petersburg (as of June 2021 - 654 rubles), as well as in accordance with Chapter 12 of the Law of St. -Petersburg “Social Code of St. Petersburg” we make an additional one-time payment for food to a donor who has confirmation of permanent residence in St. Petersburg (as of June 2021 - 814 rubles).
Summarizing this point, we give a short conclusion: any donor in federal and departmental clinics receives compensation for food in accordance with federal law (as of June 2021 - 654 rubles), and a donor who donates blood in city institutions (including at the City Blood Transfusion Station ) and having permanent registration in St. Petersburg, receives food compensation in accordance with federal law (as of June 2021 - 654 rubles) + additional payment in accordance with the “Social Code of St. Petersburg” (as of June 2021 - 814 rubles). Based on the Law of St. Petersburg “Social Code of St. Petersburg”, additional measures of social support for donors in the form of an additional one-time payment for food are paid to donors who confirm their place of residence or place of stay in St. Petersburg with the provision of a document issued by the registration authorities ( temporary or permanent registration). Please note that food compensation is not payment for blood. With the funds received, the donor must replenish his strength, namely, eat more and drink more fluids.
Social support for donors is provided in full compliance with the Federal Law “On the Donation of Blood and Its Components” and the Law of St. Petersburg “Social Code of St. Petersburg” {↑}
9) Rest periods between donations.
The frequency of donation depends on gender, type of donation and doctor’s recommendations. Whole blood is allowed to be donated no more than 5 times a year for men and no more than 4 times a year for women, and the intervals between blood donations must be at least 60 days. When donating plasma, you are allowed to donate a total of no more than 16 liters of plasma per year. As for plateletpheresis, an interval of 2 weeks between platelet donations is allowed. The blood service institution reserves the right to increase these intervals depending on the needs of medical organizations for certain components of donor blood. The final decision on the types of donation and the rest period is made by the doctor at our institution. {↑}
11) Who are Kell+ donors?
The Kell system is a blood group system that includes 25 antigens, including the most immunogenic after A, B and D, antigen K. Based on the presence or absence of K antigen in red blood cells, all people can be divided into two groups: Kell- negative and Kell-positive. The presence of antigen K (Kell-positive) is not a pathology and is inherited, like other human group antigens. In Russia, it occurs in 7-10% of residents. Currently, blood service institutions determine the presence of antigen K, as the most dangerous for the occurrence of immunological complications. Many cases of blood transfusion complications and hemolytic disease of newborns have been described, the cause of which was isoimmunization with the K antigen. Kell-negative patients should receive only blood from donors who do not have the K antigen to prevent hemolysis. Kell-positive individuals are universal recipients of blood, since they do not experience rejection of its components. “In order to prevent post-transfusion complications caused by the K antigen of the Kell system, departments and blood transfusion stations issue red blood cell suspension or mass that does not contain this factor for transfusion into medical institutions.” (Order of the Ministry of Health No. 363 of November 25, 2002). You can find out about the possibility of donating KELL-positive blood yourself on the page of blood service institutions. {↑}
12) Donation of platelet cells.
Thrombocytapheresis (platelet donation) is a procedure for removing platelet cells from a donor’s blood. Platelets are blood cells responsible for blood clotting. The speed of stopping bleeding in children with cancer, women after difficult births, and patients with bleeding disorders depends on their quantity. The plateletpheresis procedure takes from 1 to 1.5 hours. Platelets are prepared according to requests from medical organizations (by appointment via phone 635-68-85 or messengers). If there are no requests for platelets, the donor will be offered a whole blood donation if the rest interval between donations is observed. In accordance with regulatory legal acts, platelet donation is equal to blood donation and, based on the possibility of more frequent platelet donation, people performing this gratuitous donor function receive the titles “Honorary Donor of St. Petersburg” and “Honorary Donor of Russia” faster.
The doctor’s confidence in the donor’s candidacy should be maximum. This is associated not only with the risk of complications for the recipient, but also with the high price of consumables and large time costs for medical personnel and the donor. We urge you to review all of our recommendations and prepare responsibly for each platelet donation. The importance of platelet procurement is due to the relatively short “life”: the next day after donation, a fully examined dose of donor platelets must be delivered to the medical institution that submitted the application. Platelets are procured only upon request and cannot be procured for future use. Recently, the number of high-tech operations using donor platelets has increased and for this reason the need for this blood component is growing. Platelet donation is a noble and difficult mission, but very necessary for those who, for medical reasons, need one-time or regular health support and further recovery. Platelet donors are the golden fund of the blood service, because the help of this category of donors may be needed at any moment and there is no time to delay!
- During the meeting, the doctor at the City Blood Transfusion Station will provide information on how to properly donate platelets, as well as how to prepare for the procedure. Failure to comply with its requirements is fraught with blood clotting disorders, a decrease in platelet levels and, as a result, temporary exclusion from donation. You can learn more about platelet cell donation during your next visit to the City Blood Transfusion Station. You can ask questions to transfusiologists or the head of the department of donor recruitment, Elena Mikhailovna Kachurina. {↑}
13) Donor code for the application and donor’s personal account on the website yadonor.ru
What is a donation code? The donation code is a unique 20-digit code that is generated by the automated transfusiology information system and contains information about your donation displayed in the information base.
Where can I get a donation code? You can receive a donation code by contacting the reception of the City Blood Transfusion Station or the specialists of the institution’s visiting team after making at least 1 (one) donation. ATTENTION! In the case of donation in an off-site setting (on-site team), the code can initially be obtained only at the second donation. The code is issued once in printed form or as an SMS. The code can be sent to the donor via SMS when contacting the institution’s specialists with the following information provided: full name (full name), date of birth (full), mobile phone number. If the mobile phone specified in the system differs from the mobile phone indicated in the donor’s message, the donor must contact the institution in person with a passport to receive a code and enter current data into the system.
Why does the code give an error? Please note that it may take up to 24 hours from the time you receive your donation code to be activated for access to your Personal Account. The results of a complete laboratory test will be available no earlier than 48 hours after the complete donation. If more than 24 hours have passed since receiving the code, but it is still inactive, we recommend contacting technical support
14) Why is it important to donate blood and/or its components regularly.
In recent years, about 70% of Russia's donor potential consists of donors who donate blood repeatedly and repeatedly. The blood of this category of donors is the safest in terms of the transmission of infectious diseases due to regular examination and monitoring of the health status of personnel donors. People who regularly come to the Blood Service institution in the future receive the titles “Honorary Donor of St. Petersburg” and “Honorary Donor of Russia”.
And the most important thing. Help is never one-time. The future of the Blood Service lies with professional donors. Donate blood regularly. Come to the blood transfusion station at least twice a year. The importance of repeat donation is due to the fact that blood plasma is not transfused immediately, but first undergoes a quarantine procedure: it is deep frozen and stored for 6 months. If, after this period, the donor comes again and no infections are detected in his blood, then the first portion of his frozen plasma is sent to medical organizations for transfusion to patients, and the fresh one is quarantined. This measure allows you to avoid a blood transfusion from a person who may already be infected, but does not yet know about it, and laboratory tests have not yet shown the presence of dangerous pathogens in his body; the virus is either blocked by antibodies, or there is still too little of it. For example, for HIV infection this period ranges from 3 weeks to 3 months, for viral hepatitis B – 37-81 days. This period is called the seronegative “window” and lasts up to 4 months, after which infections begin to show up in blood tests. If for some reason you cannot visit our station after 4 months to donate blood again, please come just to get tested. The cost of your time will be small, and quarantined plasma, which is extremely necessary for maternity hospitals and children's institutions, will be distributed to medical institutions on time. If a donor does not come to the donor site a second time within a year, his blood, which has been quarantined, will be virus inactivated. {↑}
When reprinting information, it is mandatory to use a hyperlink to the original source of information:
- Share:
- Livejournal
- Blogs@Mail.ru
- LiveInternet
- MySpace
Print page
Bone marrow donation is a complex issue, much more complex than blood donation. The likelihood of tissue compatibility between a specific patient and a random stranger is very low. In order to find a suitable donor with a high enough probability, you need to search among tens and hundreds of thousands of people. This is why bone marrow donor registries operate in various countries. This means that many thousands of volunteers undergo so-called typing (determination of the required HLA proteins), the results are entered into a database, and when it is necessary to find a donor for a specific patient, he can be pre-selected from this database, and then compatibility can be clarified, carrying out additional tests.
The largest registries number millions of potential bone marrow donors, while the Russian one currently has only 63 thousand. Searching for donors in the registries of other countries is quite expensive, and it is simply impossible to find a donor for some nationalities that live only in Russia. That is why it is so important that as many people as possible enter a single database.
When is a bone marrow transplant needed?
Bone marrow transplantation (BMT) is used primarily in the treatment of oncological diseases such as leukemia, lesions of the lymphatic system, neuroblastoma, as well as aplastic anemia and a number of hereditary blood defects. Transplantation of bone marrow cells from a donor is sometimes the only chance for a cure.
What is a bone marrow transplant?
A bone marrow transplant actually refers to a hematopoietic stem cell transplant. Hematopoietic (blood-forming) stem cells are formed in the human bone marrow and are the founders of all blood cells: leukocytes, erythrocytes and platelets.
Who can become a donor?
Any healthy citizen of the Russian Federation under the age of 45.
How is bone marrow typing done?
To determine your HLA genotype (typing), a blood test tube will be taken from you. A blood sample (up to 10 ml) of a person who wishes to become a donor of hematopoietic cells is examined in a specialized laboratory. Information about typing is entered into the Russian register of hematopoietic cell donors.
What happens after entering data into the register?
When a patient appears who needs a bone marrow transplant, his HLA genotype data is compared with the data of potential donors available in the registry. As a result, one or more “compatible” donors can be selected. The potential donor is informed about this, and he makes a decision whether or not to become an actual donor. For a potential donor, the probability of becoming a real donor is no more than 1%.
What are the chances that a potential unrelated donor will be found?
About 80% of all patients have at least one potential donor at the preliminary search stage. This percentage is constantly growing (in 1991 it was 41%), as many countries around the world are making great efforts at both the government and community levels to increase the number of potential unrelated donors and include all racial and ethnic groups .
Unfortunately, Russia has nothing to boast about in this regard—the unrelated donation program still does not enjoy government support. It is important to add that of these 80%, not all can serve as real donors, and for the remaining 20%, transplantation can often be successfully carried out from a donor who is not a perfect match, but only partially.
Can a potential donor refuse to donate?
Sometimes a potential donor who is suitable in all respects may decide not to become a real donor. There are a number of reasons not to donate, including poor health, time and effort, and fear of the risk of complications or painful procedures. As a volunteer, a potential donor is under no obligation. However, since human life depends on the decision of a potential donor, the significance of such a decision is explained to the potential donor repeatedly and from the very beginning. Changing your decision at the last minute can have fatal consequences for the patient waiting for a bone marrow donor. Donation imposes serious obligations on a person. Most potential donors go all the way, having weighed the pros and cons and understanding the importance of their decision not only for the patient, but also for themselves.
How does the stem cell donation procedure work?
There are two options. You donate either some of your bone marrow or stem cells from your blood. The choice is usually dictated by medical necessity.
If a donor donates bone marrow, a puncture is made under anesthesia in the pelvic bone, usually making 4 to 9 tiny incisions in the pelvic area, so small that subsequent stitches are not required, and then the required amount of bone marrow is removed with a surgical needle. The procedure takes about 30 minutes. The donor's bone marrow is completely restored within a few weeks. After such a procedure, the donor remains under the supervision of a doctor for several days in a specialized hospital.
If the donor donates peripheral blood cells, then a few days before donating blood, you need to start taking a special drug that promotes the release of stem cells from the bone marrow into the blood. That's because stem cells are taken from the bloodstream through a process called apheresis (similar to plasma or platelet donation), where blood from a vein in one arm is passed through a special hematopoietic stem cell separation device and returned to the bloodstream through the vein in one arm. other hand. Of course, this procedure is performed under sterile conditions. You need to spend 5-6 hours in a relatively motionless state, but there is no need for hospitalization or anesthesia. Recovery of the taken cells takes place in 7-10 days.
Is there a risk to the donor's health?
Bone marrow donation is a surgical procedure that carries minimal risk. Serious complications are rare. They can be caused by individual reactions to anesthesia; cases of infection and reactions to the insertion of a surgical needle have been recorded. After bone marrow collection, the donor may experience pain in the operated area for some time. A hematopoietic stem cell donor may experience bone pain, muscle pain, nausea, insomnia, and fatigue from the drug taken before surgery. The most common side effects are headache and bone pain. These painful sensations go away immediately after the stem cells are collected. During apheresis, some donors complain of tinnitus due to the use of an anticoagulant to prevent blood clotting. At the end of the procedure, these effects gradually disappear. Observations of 20,000 hematopoietic stem cell donors over a long period of one to five years after transplantation showed that the risk of side effects after the apheresis procedure is extremely low. As an illustration, we note that the youngest related donor of hematopoietic stem cells in Russian practice was 1.5 years old; a donor of 11 months of age is known in the world.
Why are there so few people willing to become a bone marrow donor and what should be done?
The main thing is basic education. Many people simply do not understand what it means to be a bone marrow donor. They believe it is a procedure involving sawing through bones and removing a vital organ. It is important to explain that the collection of bone marrow cells does not pose any danger to the donor and he will be restored to the required quantity within a few days.
Entry into the register of potential bone marrow donors at City Clinical Hospital No. 52
The blood transfusion department of City Clinical Hospital No. 52 joined the creation of a national register of potential bone marrow donors. Now all donors who come for donation can undergo typing and be included in the register.
To join the register you need:
- sign an agreement on voluntary entry into the bone marrow donor register;
- donate 10 ml of blood from a vein.
Information on the Rusfond website. Register News
 Social support for donors.
Social support for donors.