Editor: Andriyanov G.Yu., general practitioner, Ph.D. April, 2019.
Synonyms: hematocrit, hematocrit number, hematocrit value, Ht, Hct, Hematocrit.
The hematocrit number is the ratio of the red blood cell volume to the liquid amount of blood (i.e., the ratio of the volume of red blood cells to plasma). The determination of this indicator is included in the mandatory list for determining other indicators in a general blood test (CBC). Hematocrit measurement is not performed separately.
The hematocrit value is used to judge the thickness of the blood and its ability to transport oxygen.
Photo: with a decrease in hematocrit value, the ratio of red blood cells to plasma volume decreases
Indications
The appointment of an OAC, which includes a hematocrit study, is included in the standard patient examination plan and is mandatory:
- when undergoing a medical examination and/or medical examination;
- if any disease is detected or suspected by a clinic doctor;
- in preparation for planned surgery;
- during hospitalization (on the day of admission and on the eve of discharge).
Calculation of the hematocrit number is required for certain indications;
- blood clotting disorder;
- dehydration (dehydration);
- assessment of the degree of anemia (anemia), polycythemia (increase in blood cells);
- bleeding.
Methods for determining hematocrit
The indicator is determined as a percentage by calculating the amount of formed elements in whole blood. It is calculated using special instruments or manually.
Centrifugation using the Wintrobe method
The blood is exposed to centrifugal force for 10-30 minutes. The formed elements are heavier than plasma, so they settle to the bottom of the test tube. The hematocrit is determined by the ratio of sediment to the total volume of biomaterial.
Calculation of the indicator using the formula
The ratio of the number of red blood cells to the total blood volume can be calculated mathematically. To do this, the following indicators are required:
- total hemoglobin concentration (ctHB);
- red blood cell count (RBC);
- mean erythrocyte volume (MCV);
- mean erythrocyte hemoglobin concentration (MCHC).
The hematocrit number (HCT) is determined by one of the formulas:
- HCT (%)=(ctHB (mmol/l)*0.0485+0.0083)*100
- HCT (%)=0.1*MCV*RBC
- HCT (%)=ctHB/MCHC*100
Direct blood cell counting method
In a given volume of biomaterial, visible blood elements are counted manually or using hematological analyzers. The method is highly accurate, and the measurement process does not take much time - no more than five minutes, but the equipment required is very expensive.
Manual counting method
Blood collected using an anticoagulant is placed in a dry, clean tube and allowed to settle. In this case, the formed elements that have greater weight settle to the bottom of the container, and the light plasma rises to the top, forming two fractions of red and yellow colors, respectively. The hematocrit indicator can be determined by the divisions on the test tube. This method is the least accurate, its error is up to 20%, so it is currently not used in laboratories.
Hematocrit norms
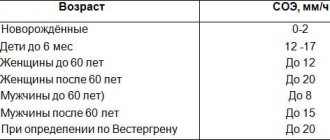
Hematocrit values depend on age, as well as gender (in adults).
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory.
That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement. Generalized standards adopted in Russia are given in the table:
Western medical literature provides more general reference values:
- Men - 0.40-0.54 / 40-54%
- Women - 0.36-0.46 / 36-46%
- Newborns - 0.53-0.69 / 53-69%
Factors influencing the result:
Hematocrit increases against the background
- stress,
- taking corticosteroid drugs and diuretics,
- traumatic shock accompanied by intense pain.
A decrease in hematocrit is facilitated by:
- prolonged immobility;
- taking blood thinners (disaggregants, anticoagulants);
- high fluid intake;
- chronic alcoholism.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Reasons for decreased hematocrit
Gestational period. Starting from the second trimester, the volume of circulating blood increases, but the number of red blood cells does not change.
Overhydration. Intravenous massive infusions lead to an increase in the volume of circulating blood, that is, to dilution of the blood, while the number of red blood cells remains the same.
Anemia of various origins. The lack of red blood cells naturally affects hematocrit values.
Intensive destruction of red blood cells. Occurs in the presence of hemolytic anemia of hereditary or acquired origin, in case of poisoning with hemolytic toxins (salts of heavy metals, consumption of toadstool) or serious infectious diseases (malaria, typhoid fever).
Blood loss (internal or external bleeding). Replenishment of circulating blood volume can be done quickly with crystalline or colloidal solutions. Restoration of lost red blood cells occurs only after a certain time or through blood transfusion.
Hyperproteinemia (increased total protein in the blood). This condition is observed in myeloma, lymphogranulomatosis, paraprotienemic hematoblastoses, diarrhea and vomiting. Excess protein in the blood draws fluids from the body into the bloodstream, increasing the volume of circulating blood while maintaining the same number of red blood cells.
A disorder of the formation of new red blood cells in the bone marrow. May be caused by blood diseases (anemia, leukemia), taking cytostatics and antitumor drugs, and renal paresis.
Tactics depending on the degree of reduction in the indicator:
- A decrease in hematocrit in the range of 35-30% requires outpatient observation by a doctor and changes in diet (increase consumption of meat, leafy greens, liver).
- When the hematocrit value decreases to 29-24%, iron supplements, B vitamins and folic acid are prescribed.
- If the rate drops to 13% or less, the condition is considered extremely serious and requires emergency hospitalization.
When the hematocrit decreases and anemia is detected in people over 65 years of age, the examination should be more thorough, since anemia in old age often accompanies serious diseases, for example, renal failure, hypo- or hyperthyroidism.
Increased hemoglobin
Diarrhea
Vomit
Thyrotoxicosis
14162 04 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Increased hemoglobin, or erythrocytosis: causes of occurrence, in which diseases it occurs, diagnosis and treatment methods.
Definition
Erythrocytosis is an increase in the content of red cells per unit volume of blood, accompanied by an increase in hemoglobin levels. The main symptoms of these changes are headaches, muscle pain, dizziness, nosebleeds, fatigue; more specific symptoms depend on the relevant disease.
Types of erythrocytosis
Erythrocytosis can be primary or secondary.
Primary erythrocytosis
is considered as an independent disease of the hematopoietic system and is of a genetic nature. Medically it is known as congenital polycythemia, or Vaquez's disease. This pathology provokes an increase in bone marrow volume and increased production of red blood cells and hemoglobin.
Secondary erythrocytosis is not considered a separate disease, but only a symptom of acute or chronic diseases and conditions. Relative erythrocytosis is a consequence of dehydration caused by excessive diarrhea or vomiting.
Also, an increase in hemoglobin levels can be the result of an overdose of medications, smoking, alcohol abuse and exposure to chemicals (nitrites).
Absolute erythrocytosis is a consequence of increased erythropoiesis, the process of formation of red blood cells in the bone marrow. This form of pathology is always associated with diseases of internal organs or systems.
Possible causes of increased hemoglobin
I. Hereditary:
- Changes in the structure of the Jak2 V617F gene, responsible for the production of red blood cells.
- Inability of blood to bind and transport oxygen to tissues.
- Reduced oxygen supply to the kidney tissues (this leads to the fact that they begin to intensively produce the hormone responsible for the formation of red blood cells (erythropoietin)).
- Deficiency of enzymes responsible for the production of red blood cells and their function of transporting oxygen to tissues.
II. Purchased:
- Kidney diseases (hydronephrosis, polycystic kidney disease, cancer and renal artery stenosis).
- Lung diseases (chronic obstructive bronchitis, bronchial asthma, diseases affecting lung tissue, sometimes of unknown cause).
- Heart diseases (congenital and acquired heart defects).
- Liver diseases (liver tumors).
- Brain diseases (in particular, cerebellar tumors).
- Diseases of the female reproductive system (ovarian cancer).
- Diseases of the endocrine system that affect the adrenal glands and contribute to increased blood pressure, in which the main drugs used for hypertension (Cushing's disease, pheochromocytoma) are usually ineffective, as well as diseases of the thyroid gland.
- Carbon monoxide poisoning.
- Staying at high altitudes.
- Obstructive apnea syndrome, characterized by temporary cessation of breathing during sleep.
Which doctors should you contact if your hemoglobin is increased?
If you detect an increase in the number of red blood cells, hematocrit, or hemoglobin, you must first contact a hematologist as soon as possible.
To clarify the diagnosis, a sternal puncture or bone marrow trepanobiopsy may be required.
Reasons for increasing hematocrit
Dehydration (dehydration). Loss of fluid due to repeated vomiting and/or diarrhea, sunstroke, burn disease, pathology of the digestive tract, intestinal obstruction, hyperhidrosis (excessive sweating), peritonitis leads to blood thickening due to an unchanged number of red blood cells.
Hypoxia. People suffering from diabetes, smokers, people located high in the mountains or in unventilated areas experience a lack of oxygen, which leads to the release of red blood cells into the bloodstream.
Cardiovascular pathology. Heart defects, coronary disease, and cardiovascular failure are accompanied by a lack of oxygen in the blood.
Bronchopulmonary pathology. Chronic hypoxia leads to: bronchial asthma, emphysema, obstructive bronchitis and other pulmonary diseases.
Neoplasms in the kidneys. Any kidney tumor provokes increased production of erythropoietin, which increases the formation of red blood cells.
Erythrocytosis. The pathology is characterized by increased production of red cells (true erythrocytosis) or redistribution of formed blood elements in some diseases (redistribution).
Erythremia. Refers to true erythrocytosis, synonymous with Vaquez-Osler disease. It is one of the variants of chronic leukemia.
Leukemia. Accompanied by an increase in white blood cells and a decrease in its liquid part.
Preparation
Donating blood for a general analysis does not require special preparation, but to identify an adequate clinical picture of the formed elements and hematocrit, it is recommended to adhere to the following rules:
- Blood donation is performed on an empty stomach;
- stopping smoking in the morning on the day of the test (blood is donated in the morning);
- refusal of physical activity the day before and on the day of delivery of the biomaterial;
- prohibition of taking anticoagulants, antiplatelet agents and other drugs that affect the blood coagulation system 3 days before the study;
- abstaining (if possible) from stress and emotional experiences on the eve of the study;
- refusal to carry out diagnostic procedures (x-ray, ultrasound and other studies) the day before donating blood.
Sources:
- A.A. Kishkun, Doctor of Medical Sciences, Prof. Guide to laboratory diagnostic methods, - GEOTAR-Media, 2007.
- Mandy Flannery O'Leary, MD, MPH, FCAP. Hematocrit. — Laboratory Medicine, Medscape, 2014.
- Andrew S Artz, MD, MS. Anemia in Elderly Persons. - Hematology, Medscape, 2015.
When is a hematocrit test performed?
Most often, hematocrit is determined as part of a general (clinical) blood test. Therefore, at present this parameter of a clinical blood test is not prescribed separately. The hematocrit level changes when:
- disorder of the blood coagulation system;
- dehydration;
- anemia or polycythemia;
- bleeding.
Assessing the hematocrit level is important when determining indications for the need for blood transfusion or the effectiveness of blood transfusion, during hemodialysis, and some operations. To determine the hematocrit number, venous or capillary blood is taken.